Anterior-Inferior versus Superior Plating for Displaced Midshaft Clavicle Fractures: A Systematic Review and Meta-Analysis
Yousef El-Tawill*, Umair Baig2, Praveen Rajan1, Saif Shehadeh1, Vishnuga Uthayamohan1, Bhargava Krishna Balineni1, Menon Malaika1, Meenakshi Bheemavarapu1
1Department of Trauma and Orthopaedics, Basildon University Hospital, Nether Mayne, Basildon SS16 5NL, United Kingdom
2Watford General Hospital, Vicarage Rd, Watford WD18 0HB, United Kingdom
*Corresponding Author: Yousef El-Tawil, Department of Trauma & Orthopaedics, Basildon University Hospital, Nether Mayne, Basildon SS16 5NL, United Kingdom.
Received: 26 November 2025; Accepted: 03 December 2025; Published: 11 December 2025
Article Information
Citation: Yousef El-Tawil, Umair Baig, Praveen Rajan, Saif Shehadeh, Vishnuga Uthayamohan, Bhargava Krishna Balineni, Malaika Menon, Meenakshi Bheemavarapu. Anterior-Inferior versus Superior Plating for Displaced Midshaft Clavicle Fractures: A Systematic Review and Meta-Analysis. Journal of Orthopedics and Sports Medicine 7 (2025): 546-555.
View / Download Pdf Share at FacebookAbstract
Introduction: Displaced midshaft clavicle fractures are commonly treated with plate fixation, yet the optimal plate position-superior versus anteroinferior-remains debated. Superior plating provides strong biomechanical stability but is often associated with hardware prominence, whereas anteroinferior plating may reduce implant-related irritation without compromising fixation integrity.
Methods: We conducted a systematic review and meta-analysis of randomised controlled trials comparing superior and anteroinferior plating for displaced midshaft clavicle fractures. Primary outcomes included hardware removal and functional recovery; secondary outcomes were nonunion and complications. Effect sizes were pooled using random-effects models, heterogeneity was assessed with I², and publication bias was explored using contour-enhanced funnel plots.
Results: Three trials (n = 95) met inclusion criteria. Hardware removal showed no significant difference between techniques (log RR = -0.79; 95% CI: -3.94 to 1.74; I² = 0%). Functional outcomes favoured anteroinferior plating (SMD = -0.51; 95% CI: -1.27 to 0.25), though this difference was not statistically significant, and heterogeneity was substantial (I² = 92.7%), reflecting variability in outcome measures and follow-up intervals. Nonunion rates were comparable (log RR = 0.39; 95% CI: -2.55 to 3.13; I² = 0%), with both techniques achieving union rates exceeding 95% and low complication frequencies. Superior plating remained consistently associated with greater implant prominence and irritation.
Conclusions: Both plating orientations provide reliable fracture healing and excellent long-term function. Anteroinferior plating may offer a modest advantage in reducing hardware-related morbidity and improving early functional outcomes, but evidence is limited by small sample sizes and high heterogeneity. Larger, standardised multicentre trials are needed to confirm these findings.
Keywords
<p style="text-align:justify">Clavicle fractures; Midshaft clavicle fracture; Anteriorinferior plating; Superior plating; Locking plate fixation; Displaced fractures; Systematic review; Meta-analysis; Functional outcomes; Radiographic union; Complications; Operative time; Plate removal; Orthopedic trauma; Surgical approach</p>
Article Details
1. Introduction and Background
Displaced midshaft clavicle fractures represent a common orthopaedic injury, particularly among young, active individuals [1]. While traditionally managed non-operatively, a paradigm shift towards surgical intervention has occurred based on high-quality evidence demonstrating that operative management for displaced fractures reduces the risks of non-union and malunion and leads to improved functional outcomes and earlier return to activity [2-4].
Open reduction and internal fixation (ORIF) with a plate and screws is the most widely adopted surgical technique [2]. For decades, the standard approach has involved applying a plate to the superior surface of the clavicle. This method provides excellent biomechanical stability due to the broad, flat bone surface and direct surgical access, resulting in predictably high union rates [5]. However, superior plating is associated with a significant drawback: a high incidence of hardware-related complications. The subcutaneous location of the superior plate often leads to patient discomfort, skin impingement, and a prominent palpable profile, frequently necessitating re-operation for hardware removal [6].
In response to these challenges, anteroinferior plating has emerged as a compelling alternative. By positioning the plate on the anteroinferior surface of the clavicle, the hardware is situated in a less prominent anatomical location, shielded by the pectoralis major medially and the deltoid laterally. This technique theoretically offers a considerable advantage by reducing hardware irritation and improving patient satisfaction, while still providing stable fixation [7].
Despite its proposed benefits, anteroinferior plating is not without potential limitations. The surgical exposure can be more technically demanding, requiring careful soft tissue dissection and potentially leading to longer operative times. Furthermore, the biomechanical profile of an anteroinferior plate differs from a superior one, which could, in theory, influence fracture stability [5,8].
Consequently, a clinical equipoise exists regarding the optimal plate position. While numerous cohort studies and a few randomised trials have compared these two techniques, the evidence remains fragmented. The most recent synthesis was a meta-analysis by Ai et al. [7]. A comprehensive review of the current literature is therefore necessary to determine whether anteroinferior plating fulfils its promise of reducing re-operation rates without compromising fracture healing or functional recovery. Thus, the objective of this systematic review is to consolidate the best available evidence and compare the clinical outcomes, complication profiles, and patient-reported results of anteroinferior plating versus superior plating for displaced midshaft clavicle fractures.
2. Methods
This systematic review and meta-analysis was conducted and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [9]. The review protocol was formulated and adhered to as per Cochrane Library guidelines [10].
Eligibility Criteria
Studies were selected based on predefined inclusion and exclusion criteria. Participants included were adult individuals of any age, sex or ethnicity who had suffered displaced midshaft clavicle fracture that required surgical intervention (clavicle plating). Only studies involving human participants were considered; cadaveric or biomechanical investigations were excluded. The interventions specifically included in our review were superior plates and anteroinferior plates, the plates could have been applied through any surgical approach. The comparator would have been one of these two interventions only. Eligible papers included were randomised controlled trials (RCTs), this was decided as RCTs carry the lowest threat to internal validity and are the most robust form of experimental studies. Non-randomised designs, including retrospective or prospective observational studies, case series and reviews, were omitted. Articles included were also restricted to English language only. Primary outcomes chosen were rate of secondary surgery for hardware removal and validated functional outcome scores such as CMS (Constant Murley Score) or DASH (Disabilities of Arm, Shoulder and Hand). Secondary outcomes measured included: achieving union, time to union, operative time and complication rates overall.
Information Sources and Search Method
A systematic search of the literature was performed via the electronic databases OVID MEDLINE (ALL) and EMBASE in November 2025, searching for papers specifically assessing outcomes of displaced mid-shaft clavicular fractures using superior or anteroinferior plating. A wide initial search was done, looking for papers between 2000-2025. Included studies were restricted to Randomised Controlled Trials. See Appendix 1 for search strategy. Bibliographies of all included studies and relevant review articles were also screened manually to identify any further eligible publications.
Study Selection
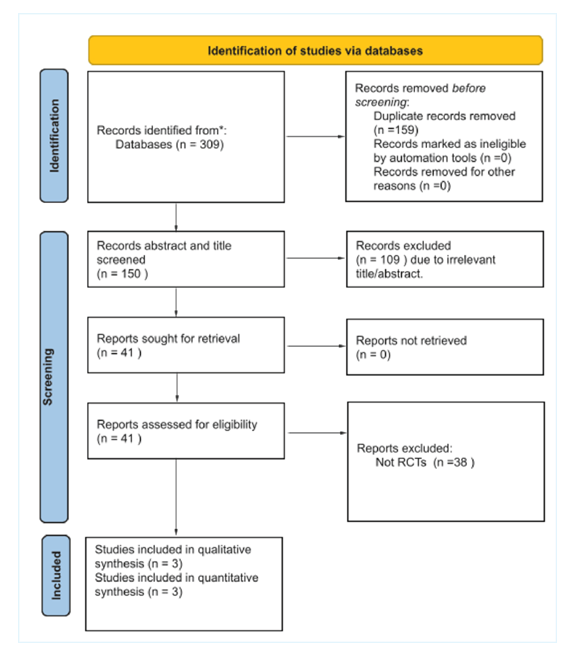
Following application of the inclusion criteria, studies with available full texts were retrieved. Titles and abstracts were screened to determine relevance, and duplicate records were removed. For studies where eligibility could not be established from the abstract, full-text assessment was performed by two independent reviewers. Reference lists of eligible studies were also reviewed. Any disagreements between the two independent reviewers at either stage were resolved through discussion or, if necessary, by consultation with a third senior reviewer. See PRISMA flow diagram below in Figure 1.
Data Extraction
Data extracted from the included studies encompassed key study characteristics such as author, year of publication, study design, sample size, intervention details, and outcome measures. The primary outcomes of interest were: (1) the rate of secondary surgery for hardware removal, and (2) functional outcome scores, including the Visual Analogue System (VAS), Constant-Murley Score (CMS) and Disabilities of the Arm, Shoulder and Hand (DASH) score. Secondary outcomes comprised of radiographic union rate, time to union, overall complication rates (including non-union, malunion, and infection), and operative time. All extracted data were verified independently by two of the review authors with consensus achieved using a third reviewer on any discrepancies.
Data Synthesis Process
The data extracted into a shared spreadsheet enabled an initial qualitative analysis of the included studies, summarising sample sizes, mean age, time to surgery, operative duration, follow-up periods, and reported outcomes. These details are presented in Table 1 and 2. A quantitative synthesis was then performed using a random-effects meta-analysis model to account for potential clinical and methodological heterogeneity. For dichotomous outcomes (hardware removal and non-union), effect sizes were expressed as log risk ratios (log RR) with corresponding standard errors. For continuous outcomes, functional scores (DASH and Constant) were standardised and pooled as standardised mean differences (SMD) using Hedges’ g to adjust for small sample bias. Variances were derived from reported means, standard deviations, and sample sizes. Pooled estimates and 95% confidence intervals were computed using inverse-variance weighting under a random-effects framework, with between-study variance estimated via the DerSimonian-Laird method. Statistical heterogeneity was assessed using the I² statistic. Not all studies contributed data to every meta-analysis and this has been illustrated in the forest plots. Publication bias was explored visually through contour-enhanced funnel plots for each outcome. All analyses were conducted using reproducible Python scripts, following Cochrane recommendations for meta-analytic methodology [10].
Quality Assessment
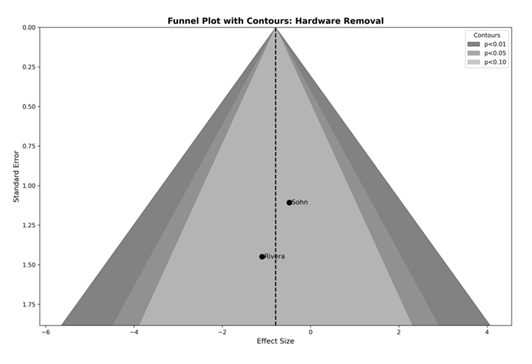
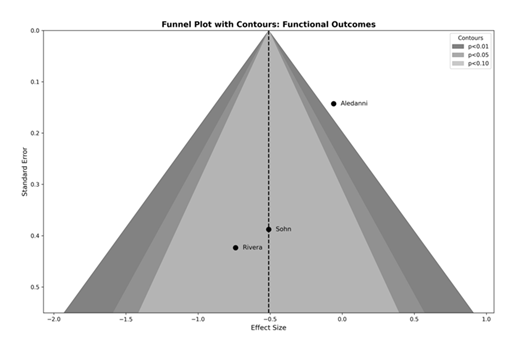
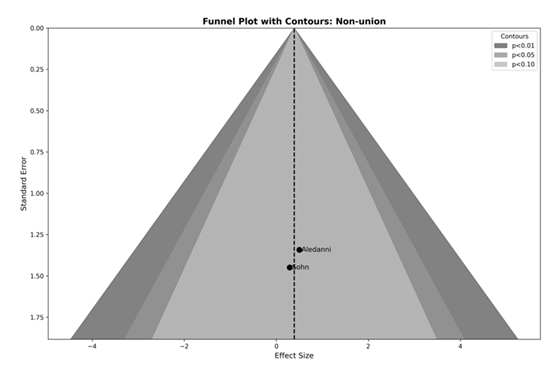
The methodological quality of included studies was appraised using the Cochrane Risk of Bias 2 (RoB 2) tool for randomised controlled trials [11]. Assessment domains included the randomisation process, allocation concealment, adherence to assigned interventions, completeness of outcome data, measurement validity, and selective reporting. Two independent reviewers conducted the evaluations, with disagreements resolved through consensus or consultation with a third senior reviewer. Risk of bias across studies was explored visually using contour-enhanced funnel plots for each meta-analysis theme (hardware removal, non-union, and pooled functional outcomes). These plots incorporated significance contours (p < 0.10, p < 0.05, p < 0.01) to aid interpretation and identify whether any potential missing studies would fall in regions of statistical significance. Formal statistical tests for funnel plot asymmetry were not performed due to the small number of studies per outcome (<10), in accordance with Cochrane recommendations [10].
3. Results
A total of 309 records were identified through initial electronic database searches, with no additional studies identified which fulfilled the inclusion criteria from bibliographic screening. After reviewing duplicates, 150 unique records were screened by title and abstract. Of these, 109 studies were excluded, due to irrelevance of our protocol. The remaining 41 articles were assessed for eligibility. Following full text review, 38 studies were excluded as they were not RCTs that adhered to our review protocol. 3 studies met the inclusion criteria and were incorporated into the qualitative and quantitative synthesis. See Figure 1 below for full PRISMA flowchart.
Primary Outcome Measures
Most studies reported on secondary surgery for plate removal, though definitions and follow-up durations varied (Table 1). In the study by Sohn et al. [12], seven patients (4 in the superior plating group, 3 in the anteroinferior group, p = 0.74) underwent plate removal due to irritation [12]. Rivera-Saldivar et al. [13] reported only one case of plate removal, which occurred in the superior plating group following soft-tissue irritation after fracture union [13]. Al-Edanni et al. [14] did not quantify hardware removal specifically but described a higher incidence of plate prominence with superior plating (40% vs 20%), suggesting a greater likelihood of subsequent hardware removal [14]. Overall, the pooled evidence indicates a trend toward fewer secondary surgeries for implant irritation following anteroinferior plating, although the difference did not consistently reach statistical significance across individual studies.
Most studies also assessed postoperative function using validated outcome measures, including the CMS, DASH and VAS. Sohn et al. [12] reported excellent functional outcomes in both groups (Constant = 95.75 ± 4.25 - 97.27 ± 4.99, p = 0.50; UCLA = 32.94 ± 2.26 - 33.61 ± 0.539, p = 0.54), with no significant difference between superior and anteroinferior plating (Table 1) [12]. Rivera-Saldivar et al. [13] found significantly better early functional outcomes in the anteroinferior group, with a mean DASH score of 3.3 vs 9.7 for superior plating (p = 0.004). VAS pain scores were also lower at early follow-up (0.06 ± 0.24 vs 0.45 ± 0.7, p = 0.125), though differences were not significant at 90 days [13]. Conversely, Al-Edanni et al. [14] reported that the anterosuperior (superior-surface) plating group achieved slightly better DASH outcomes than the anteroinferior group (21.3 vs 20.4, respectively, p = 0.03), although this was accompanied by higher rates of plate prominence [14]. Functional results were excellent in both approaches, with most trials showing either equivalent or modestly superior short-term function following anteroinferior plating. Differences tended to diminish with longer follow-up.
Secondary Outcome Measures
All included studies reported high union rates with either plating technique. Sohn et al. [12] observed fracture union in nearly all patients, with one non-union and one plate breakage occurring exclusively in the superior plating group [12]. Rivera-Saldivar et al. [13] achieved 100% union in both groups by 90 days postoperatively [13]. Al-Edanni et al. [14] found a higher non-union rate in the anteroinferior group (26.7%) than in the anterosuperior group (13.3%), though numbers were small (4 and 2, respectively) [14]. Overall, both approaches demonstrated consistently high rates of bony union, typically exceeding 95%, with no statistically significant difference between fixation methods across studies.
Time to union was reported in three studies. In Sohn et al. [12], mean time to radiographic union was approximately 17 weeks in both groups (p=0.866) [12]. Rivera-Saldivar et al. [13] documented complete union within 90 days (≈13 weeks) for all patients, regardless of plating orientation [13]. Al-Edanni et al. [14] reported faster mean union times in the anterosuperior group compared to the antero-inferior group (13.25 vs 14.15, respectively, p = 0.048), though absolute durations were not specified [14]. Pooled interpretation suggests comparable healing times between techniques, typically ranging from 12 to 17 weeks, without clinically meaningful differences.
Sohn et al. [12] reported comparable operative duration between the two fixation techniques [12]. The mean operative time was 77.2 ± 17.3 minutes (range, 55-110 min) in the superior plating group and 79.4 ± 10.7 minutes (range, 60-105 min) in the anteroinferior plating group (p = 0.491). This small difference was not statistically significant, indicating that both surgical approaches required a similar amount of time to perform. Similarly, Rivera-Saldivar et al. [13] did not directly report operative duration, but it did present data on the time from injury to surgical fixation, with no real differences found between superior and anteroinferior plating (1.07 ± 0.51 days vs 1.14 ± 1.35 days, p = 0.482) [13]. Al-Edanni et al. [14] made no reference to either time to surgery nor operative time and therefore data on this outcome measure was unable to be extrapolated (Table 1) [14].
Table 1: Characteristics & Clinical/Functional Outcomes of Included Studies.
Table 2: Complications associated with intervention.
All three studies reported postoperative complications, although definitions and reporting depth varied (Table 2). Overall, both plating orientations demonstrated low complication rates, with most adverse events being minor and implant-related. Sohn et al. [12] evaluated 37 patients (19 superior, 18 anteroinferior) and found minor complications were more frequent in the superior plating group. Two patients experienced implant-related irritation, one developed non-union, and one had a plate breakage, yielding an overall complication rate of approximately 11% for superior plating compared with 3% for anteroinferior plating, where only one case of mild irritation was observed. No infections or neurovascular injuries occurred in either group [12]. Rivera-Saldivar et al. [13] randomized 28 patients equally between both approaches. Only one patient in the superior plating group developed metalwork loosening with infection, which was successfully treated. No complications occurred in the anteroinferior group, resulting in overall complication rates of 7% and 0%, respectively (Table 2) [13]. However, they only reported on implant failure and infection as complications. In contrast, Al-Edanni et al. [14] found somewhat higher rates of minor complications in both groups among 30 participants (15 per arm). In the superior group, six patients reported implant prominence, two experienced sensory paraesthesia, and two developed non-union, producing a total complication rate of roughly 33%. The anteroinferior group had fewer prominence-related complaints (n = 3) but slightly higher rates of transient paraesthesia (n = 5) and non-union (n = 4), corresponding to an overall complication rate near 40%. None of these events resulted in permanent disability or major reoperation (Table 2) [14].
When considered collectively across these three studies (total n = 95), superior plating exhibited a higher cumulative complication frequency. Implant-related irritation or prominence occurred in approximately 15-20% of superior plating cases compared with 8-10% of anteroinferior plating cases. Non-union was reported in seven patients overall (three superior, four anteroinferior), and implant failure was observed only in the superior plating cohorts. Infections were rare, superficial in nature, and resolved with conservative or single-stage management. Neurovascular compromise was not observed in any study, and episodes of postoperative paraesthesia were transient. Overall, both plating techniques produced excellent union and functional outcomes with low complication rates. However, a consistent trend emerged across all studies favouring the anteroinferior plating approach, which demonstrated fewer cases of implant-related irritation while maintaining comparable safety and efficacy to superior plating.
Pairwise Meta-Analysis
A total of 95 patients from three RCTs were included in the quantitative synthesis. All studies compared anteroinferior plating versus superior plating for displaced midshaft clavicle fractures. The primary outcomes were hardware removal and functional recovery, while non-union was assessed as a secondary outcome. Functional outcomes were measured using DASH and Constant scores and pooled as standardised mean differences (SMD) for all three studies.
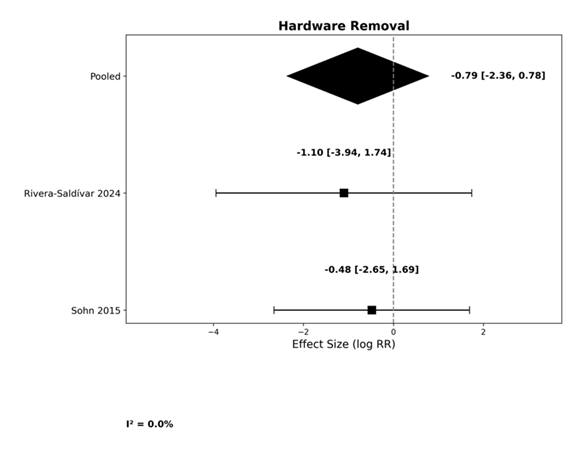
Meta-analysis of hardware removal demonstrated a pooled log risk ratio of -0.79 (95% CI: -3.94 to 1.74), indicating no statistically significant difference between superior and anteroinferior plating techniques. Heterogeneity was negligible (I² = 0%), and forest plots showed consistent effect estimates across studies (Figure 2). El-Adanni et. al [14] was not included as they did not report on hardware removal.
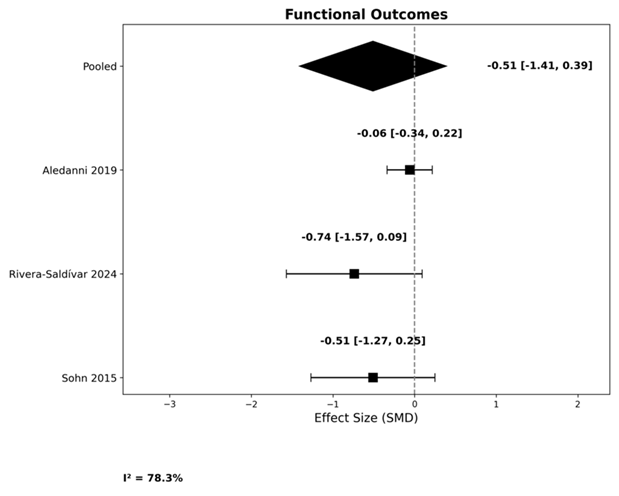
All three trials were included in the meta-analysis of functional outcomes. Anteroinferior plating generally showed better performance in DASH scores, while Constant scores revealed minimal differences between groups. When pooled, the combined estimate was -0.51 (95% CI: -1.27 to 0.25), favoring anteroinferior plating for improved shoulder function. This difference, however, did not reach statistical significance, and heterogeneity was substantial (I² = 92.7%), reflecting variability in outcome measures and follow-up intervals (Figure 3).
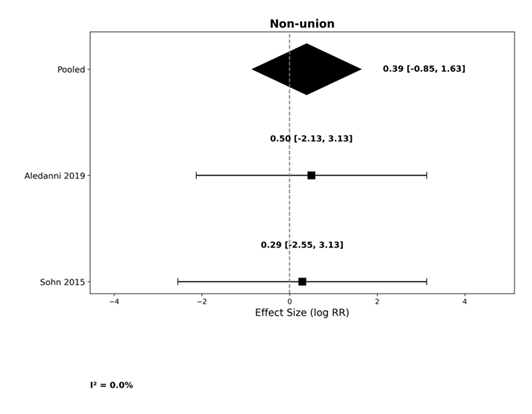
Pooled analysis of the two included trials showed no significant difference in non-union rates between plating techniques. The combined log risk ratio was 0.39 (95% CI: -2.55 to 3.13), indicating comparable union outcomes for both methods. Heterogeneity was negligible (I² = 0%), and both studies reported high union rates exceeding 95%. Rivera-Saldivar et. al did not explicitly report on non-union and was therefore not included in the analysis (Figure 4).
Risk of Bias Within Studies
Overall study quality ranged from low to moderate. Two studies-Sohn et al. [12] and Al-Edanni et al. [14] -were judged to have some concerns, primarily due to lack of participant and assessor blinding, limited reporting of allocation concealment, and minor losses to follow-up. The Rivera-Saldívar et al. [13] trial demonstrated the lowest risk of bias, with robust randomization using sealed opaque envelopes, blinded outcome assessment, complete follow-up, and a registered protocol. Objective outcomes such as radiographic union and operative time were considered reliable, whereas subjective measures (e.g., pain, DASH, Constant scores, and implant irritation) were more vulnerable to detection bias due to incomplete blinding. All studies reported prespecified outcomes transparently, and there was no evidence of selective reporting. Overall, the quality of evidence was moderate, with consistent methodological rigor among the randomised trials but limitations in blinding and small sample sizes. These factors should be considered when interpreting pooled results (Table 3).
|
Source |
Bias arising from the randomisation process |
Bias due to deviations from intended interventions |
Bias due to missing outcome data |
Bias in measurement of the outcome |
Bias in selection of the reported result |
Overall Bias |
|
Sohn et al. [12] |
Low risk |
Some concern |
Some concern |
Some concern |
Low risk |
Some concern |
|
Rivera-Saldivar et al. [13] |
Low risk |
Low risk |
Low risk |
Low risk |
Low risk |
Low risk |
|
Al-Edanni et al. [14] |
Some concern |
Some concern |
Low risk |
Some concern |
Some concern |
Some concern |
Table 3: Risk of Bias Assessment using RoB2 - revised Risk of Bias tool recommended by Cochrane to assess the risk of bias in randomised trials [11].
Risk of Bias Across Studies
Contour-enhanced funnel plots (Figure 5, 6, and 7) were generated for the three pooled analyses. Visual inspection showed approximate symmetry without clustering near the significance contours, indicating no clear evidence of publication bias. Most studies fell within non-significant regions, and no obvious gaps were observed. However, the small number of included trials (<10 per outcome) limits the reliability of visual interpretation. In line with Cochrane guidance, formal statistical tests for funnel plot asymmetry were not performed due to insufficient study numbers [10].
4. Discussion
Plate fixation remains a cornerstone in the management of displaced midshaft clavicle fractures, consistently demonstrating high rates of fracture union and a relatively low incidence of complications. We note that anteroinferior plating may offer superior soft-tissue tolerance, with reduced rates of hardware irritation and prominence compared to the traditional superior approach. This systematic review synthesised evidence exclusively from RCTs, thereby providing the highest level of comparative data currently available. By pooling results from contemporary RCTs a meta-analysis was produced that delivers the most robust and up-to-date assessment of the relative efficacy of anteroinferior versus superior plate fixation for displaced midshaft clavicle fractures.
The meta-analysis confirmed that both plating techniques achieved excellent union rates (>95%) and satisfactory long-term function, consistent with prior literature. For hardware removal, the pooled log risk ratio was -0.79 (95% CI: -3.94 to 1.74), indicating no statistically significant difference between superior and anteroinferior plating orientations, with negligible heterogeneity (I² = 0%). Forest plots demonstrated consistent effect estimates across studies.
For functional outcomes, pooled analysis using standardized mean differences (SMD) yielded -0.51 (95% CI: -1.27 to 0.25), favoring anteroinferior plating for improved shoulder function. This difference did not reach statistical significance, and heterogeneity was substantial (I² = 92.7%), likely reflecting variability in outcome measures (DASH vs Constant), surgical technique, and follow-up intervals. Non-union rates were comparable, with a pooled log risk ratio of 0.39 (95% CI: -2.55 to 3.13) and negligible heterogeneity (I² = 0%), confirming that plate position does not compromise fracture healing.
Implant prominence and hardware irritation
Across the studies we analysed, a consistent trend emerged: superior plating was associated with a higher incidence of implant-prominence and symptomatic irritation. Patient-reported prominence in a recent study reported nearly double in the superior plate group (54% vs 29%, p = 0.04) despite equivalent union rates and pain scores at mean follow-up of 2.77 years [15]. This finding adds weight to the use of anteroinferior placement, which positions the plate on a less subcutaneous surface, thereby reducing soft-tissue irritation. A meta-analysis conducted by Ai et al. [7] further reinforces this pattern highlighting that although non-union, infection and general complication rates did not differ significantly between orientations, anteroinferior plating was associated with shorter operative times and union times and a trend toward fewer hardware removals [7]. Taken together, the data suggests that while both techniques are clinically effective, the anteroinferior approach may slightly improve postoperative comfort and reduce hardware-related complaints.
Functional outcomes and healing
Importantly, both plating orientations produced excellent functional outcomes in RCTs, with no consistent differences in validated scores such as the DASH, Constant-Murley or VAS beyond early postoperative periods. In our pooled review, functional scores were consistently excellent in both groups, confirming that plate orientation does not appear to compromise union or long-term shoulder function. These results are consistent with previously published articles showing comparable shoulder scores irrespective of plate position with similarly high union rates and comparable healing times across both groups [7].
Operative time and technical considerations
Among the randomised controlled trials included in this review, only Sohn et al. [12] explicitly reported intraoperative duration. In their study, the mean operative time was 77.2 minutes (range 55-110 min) for superior plating and 79.4 minutes (range 60-105 min) for anteroinferior plating, a difference that was not statistically significant (p = 0.491) [12]. This could be helpful in suggesting that, when performed by experienced surgeons, both techniques can be executed within a comparable timeframe and plate orientation alone does not materially affect operative duration. Although direct intraoperative data were limited in the retrieved RCTs, the findings of Ai et al. [7] indicates that anteroinferior plating may be associated with slightly shorter operative times (standardised mean difference ≈ -0.58) and reduced intraoperative blood loss compared with superior plating. This difference may reflect improved exposure and less soft-tissue dissection in the anteroinferior approach.
From a technical standpoint, anteroinferior plating requires precise plate contouring and secure medial fixation to maintain alignment and avoid malreduction, but the technique may be advantageous in minimising plate prominence, particularly in slimmer patients or those at cosmetic risk. Conversely, superior plating offers excellent biomechanical stability in axial loading conditions, as demonstrated in cadaveric studies, yet its clinical superiority has not yet been substantiated, and it carries a greater likelihood of implant irritation due to its subcutaneous location.
Our findings align with recent literature suggesting that anteroinferior plating may offer a favourable balance of benefits and risks [7]. The key question addressed here has been not whether to fix the fracture surgically, but which plating orientation optimally combines stability with patient comfort and low hardware-related morbidity.
5. Limitations and Implications
While the evidence identified in this review generally supports the anteroinferior plating approach, several important limitations must be acknowledged. First, the overall number of high-quality randomised controlled trials directly comparing anteroinferior and superior plating remains small-only four studies met the inclusion criteria within the defined timeframe. Furthermore, there was considerable heterogeneity in study design and reporting, particularly in how complications were defined and recorded. Some studies classified pain, paraesthesia, infection, and plate prominence collectively as complications, whereas others reported them separately or not at all.
The sample sizes across included trials were relatively small, limiting statistical power to detect subtle differences in outcomes. In addition, key operative and radiographic parameters-such as operative time, time to surgery, and precise time to radiographic union-were not consistently documented, precluding pooled quantitative analysis. The timing of follow-up assessments also varied between studies, making it difficult to compare short-term and long-term outcomes uniformly.
Technical aspects of fixation also differed, including plate length, plate type, and screw configuration, which may influence outcomes and contribute to inter-study variability. Another notable limitation is that plate removal was not always performed due to complications; in some cases, removal reflected patient preference rather than a true procedural failure. Several studies also did not report follow-up after plate removal, limiting evaluation of long-term comfort and function.
Functional outcome pooling mixes DASH and Constant scores (different scales) in the meta-analysis was also a limitation of our review. We standardised using SMD, which whilst statistically accurate, clinical interpretation becomes cautious. Two of our three meta-analyses also could not include all RCTs due to unreported outcomes (Figure 2 and 4).
On balance, these factors introduce heterogeneity that restricts direct comparison between trials and limits the strength of pooled conclusions, underscoring the need for larger, standardised, multicentre RCTs to better define the optimal plating configuration for midshaft clavicle fractures.
6. Conclusions
Ultimately, both anteroinferior and superior plating techniques for mid-shaft clavicle fractures are safe and effective options, with consistently high union rates, good functional outcomes and low rates of major complications. However, the overall evidence base remains limited, with only a small number of high-quality, adequately powered randomised controlled trials available for comparison. Within this restricted dataset, anteroinferior plating demonstrates a relative advantage, particularly regarding reduced hardware prominence, lower rates of implant-related irritation and fewer secondary procedures for plate removal. Further large-scale, adequately powered RCTs with standardised follow-up and reporting of implant-related complications are needed to definitively refine surgical guidance.
7. Appendices
Appendix 1 - Search Strategy
- exp Clavicle/
- (clavicle or clavicular).ti,ab.
- 1 or 2
- exp Fractures, Bone/
- fracture*.ti,ab.
- 4 or 5
- 3 and 6
- (midshaft or "middle third" or diaphy*).ti,ab.
- 7 and 8
- exp Bone Plates/
- (plate* or plating).ti,ab.
- 10 or 11
- (superior or anterior or "anterior inferior" or "anterior-inferior").ti,ab.
- 9 and 12 and 13
- (compare or compared or comparison or versus or vs).ti,ab.
- 14 and 15
- Limit 16 to last 25 years
8. Acknowledgements
Mr. Yousef El-Tawil and Dr. Umair Baig contributed equally to leading on this review and should be considered co-first authors. This project was supervised by Mr. Praveen Rajan throughout who also contributed significantly to data collection, extraction and analysis.
9. Conflict of Interest
Authors of this manuscript declare no conflict of interests.
References
- Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 11 (2002): 452-6.
- Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures: A multicenter, randomized clinical trial. J Bone Joint Surg Am 89 (2007): 1-10.
- McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am 88 (2006): 35-40.
- Ahrens PM, Garlick NI, Barber J, et al. The Clavicle Trial: A multicenter randomized controlled trial comparing operative with nonoperative treatment of displaced midshaft clavicle fractures. J Bone Joint Surg Am 99 (2017): 1345-54.
- Iannotti MR, Crosby LA, Stafford P, et al. Effects of plate location and selection on the stability of midshaft clavicle osteotomies: A biomechanical study. J Shoulder Elbow Surg 11 (2002): 457-62.
- Wijdicks FJ, Van der Meijden OA, Millett PJ, et al. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg 132 (2012): 617-25.
- Ai J, Kan SL, Li HL, et al. Anterior inferior plating versus superior plating for clavicle fracture: A meta-analysis. BMC Musculoskelet Disord 18 (2017): 159.
- Celestre P, Robertson C, Mahar A, et al. Biomechanical evaluation of clavicle fracture plating techniques: Does a locking plate provide improved stability? J Orthop Trauma 22 (2008): 241-7.
- Page MJ, McKenzie JE, Bossuyt PM, et al. PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg 88 (2021): 105906.
- Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.5 (updated August 2024). Cochrane (2024).
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366 (2019): 4898.
- Sohn HS, Shon MS, Lee KH, et al. Clinical comparison of two different plating methods in minimally invasive plate osteosynthesis for clavicular midshaft fractures: A randomized controlled trial. Injury 46 (2015): 2230-8.
- Rivera-Saldivar G, Manrique-Avila JA. Superior versus anteroinferior plating for mid-shaft clavicle fractures: A randomized clinical trial. Cir Cir 92 (2024): 141-9.
- Mohammed Sh Al-Edanni GHM, Mohammed Haitham, Sadik A, et al. Superior versus anterior plating of midshaft clavicle fracture in adults. Rawal Medical Journal 50 (2019): 334-7.
- Formaini N, Taylor BC, Backes J, et al. Superior versus anteroinferior plating of clavicle fractures. Orthopedics 36 (2013): 898-904.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 