Biomarker Variability Severity of CORADS and Impact of Psychotropic Medications on Course and Outcome of Neuropsychiatric Sequalae of COVID-19 ICU Patients: A Preliminary Observation from South India
Ashwini Kamble MD1, Srinivas Kandrakonda MD, MPH2, Praveen Khairkar MD3*, Sravanasandya Penugonda MD DM4, Dheeraj Jain5
1Professor, Department of Biochemistry and Laboratory Director, Pacific Institute of Medical Sciences Udaipur Rajasthan India
2Professor and Head, Department of Psychiatry, Kaminemi Institute of Medical Sciences, Narketpally, Telangana State, India
3Professor and Head Department of Psychiatry and Clinical Neuroscience, Pacific Institute of Medical Sciences Udaipur Rajasthan India and Senior Visiting Consultant, AIG and Apollo DRDO Hospital Hyderabad, India
4Professor and Head, Department of Pharmacology, T Rammohan Reddy Institute of Medical College, Hyderabad, India
5Chairman, Redcliffe Labs India
*Corresponding author:Praveen Khairkar, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Received: November 25, 2025;Accepted: December 17, 2025;Published: December 29, 2025
Article Information
Citation: Praveen Khairkar. Biomarker Variability Severity of CORADS and Impact of Psychotropic Medications on Course and Outcome of Neuropsychiatric Sequalae of COVID-19 ICU Patients: A Preliminary Observation from South India. Archives of Clinical and Biomedical Research. 9 (2025): 562-568.
View / Download Pdf Share at FacebookAbstract
Introduction: There is growing evidence of neuropsychiatric presentations in patients of COVID-19, but literature is scarce on laboratory, clinical and radiological markers as well as impact of psychotropic medications during the course of hospitalization in critically ill patients.
Materials and methods: We screened 430 ICU patients admitted to our tertiary care hospitals, out of whom 67 were diagnosed positively with definitive neuropsychiatric sequalae and receive psychotropic interventions during their hospital stay. We compared their D-dimer levels, C-reactive proteins, serum ferritin levels, serum procalcitonin and Vitamin D levels and further analyzed CORADS severity score with psychiatric severity and outcome.
Results: The mean age of the patients was 42.38 years, majority (44.8%) of them belonged to 21-34 years with slight (52.2%) male preponderance and none of them were more than 60 years. We observed a 43.3% were having organic mood disorder and 37.3% of individual had significant history of alcohol dependence while hypertension and diabetes mellitus were noted in 34.3% and 29.9% respectively.Only D-dimer levels were found to be significant and positively associated with outcome of psychiatric disorders (p<0.05), accounting for 41% of covariance on linear regression analysis.
Conclusions: Our study has found significant association of elevated levels of D-dimer variability but not the other laboratory biomarkers among various neuropsychiatric comorbid sequalae in ICU admitted COVID 19 patients. This particular observation might have potential for serum D-dimer levels to be possibly used as an early biomarker to screen or suspect for comorbid neuropsychiatric presentations.
Keywords
COVID-19; Neuropsychiatry; Laboratory Biomarkers; CORADS score; Outcome
Article Details
Introduction
The Corona virus disease 2019 (COVID-19) has infected over 250 million people by 30th November 2021and caused more than 5 million deaths irrespective of existing healthcare treatment facilities throughout the globewhich has brought the fields of critical care medicine, laboratory medicine and psychoneuroimmunology into limelight as never before [1]. As evident from a large database from United States (US), as much as 80% of the all COVID-19 patients have self-limiting course and the need for intensive care unit (ICU) admission was just 2% in confirmed patients with case fatality rate of 5% [2]. Further, lungs remain the primary target organ as 30.8% of those with acute respiratory distress syndrome (ARDS) due to severe pneumonia died in ICU settings and comparative mortality rates for those in the 18-to-65 and older-than-65 age groups who did not receive mechanical ventilation in ICU were 1.98% and 26.6%, respectively [3,4]. While a proteomic analysis report by Leng et al found whopping 641 differentially expressed proteins in lung tissue from deceased COVID-19 patients reflecting the complexities of biomolecular interplay in its pathogenesis, Poggiali et al. [6] identified lactate dehydrogenase and C-reactive proteins as predictors of lung damage and respiratory failure and further emphasized that early identification using these biomarker levels of CoVID-19 patients who could be athigh risk for acute respiratory failure are paramount to avoid ARDS andend-organ damage [5,6]. So far, most of laboratory biomarker investigations in critically ill COVID-19 patients have focused around neutrophil-to- lymphocyte ratio, indicators of hypercytokinemia like IL-6, IL-10, anti-SARS-CoV-2 spike RBD immunoglobulin M and G, growth differentiated factor-15, procalcitonin, D-dimer or serum ferritin as a marker of severity and prognosis of infection [7-10]. This was interesting to note as it sparked the biomarker exploration that began extending the boundaries from cardiorespiratory to neuropsychiatric domains as this highly contagious COVID-19 continued to contribute to delayed neuropsychiatric complications reported in as much as 1771 studies in Medline/PubMed database as of now. In fact, two large meta-analyses [11,12] reported a cumulative prevalence of 20% to 25% for major psychiatric disorders like mood disorders, anxiety disorders, insomnia, memory/ cognitive impairment, fatigue and hypochondriacal disorder. The findings of hypoperfusion of frontotemporal regions [13] in delirious ICU admitted COVID-19 patients, demyelinating structural abnormalities of thalamus [14] and striatum [15] reflecting evidence of brain parenchymal invasion which further supported by SARS-CoV-2 RNA protein detected in cerebrospinal fluid of these individuals. However, in one of the comprehensive postmortem studies suggests that presence of SARS-CoV-2 was not associated with severity of neuropathologic changes observed which in turn suggests that immune-mediated processes, rather than direct virus effects, drive the pathogenesis of CNS symptoms and syndromes associated with SARS-CoV-2 [16]. Nevertheless, it allows us the window for exploring variabilities of biomarkers for biological neuropsychiatric presentations related to severely affected COVID-19 patients in ICU.Further, the mounting evidence from recent literature probably suggests that psychotropic medications like risperidone and aripiprazole potentially modulate the cytokine storms by suppressing the expression of inflammatory cytokines and inducible inflammatory enzymes (i.e., cyclooxygenase) and microglia activation and this can significantly play the role in course and outcome in critically ill COVID-19 patients admitted in ICU with some or other comorbid neuropsychiatric sequalae [17-20]. In fact, aripiprazole demonstrated better anti- inflammatory effects on TNF-α, IL-13, and IL-17α and also share the pathways related to immune system for enrichment of common genes with altered expression in COVID-19 [21]. Thus, the present preliminary study evaluated laboratory biomarker variabilitywith psychotropic medications like risperidone, aripiprazole, specific serotonergic inhibitors like escitalopram and also with severity of CORADS in course and outcome of neuropsychiatric sequalae of COVID-19 ICU Patients from South India. To the best of our knowledge, such comprehensive integral exploration which can perhaps link and strengthen psychoneuroimmunological domains is not directly conducted in any of the previously published studiesas yet.
Methodology
The present study is a prospective, cross-sectional qualitative study aimed to investigate correlation of laboratory biomarker variability, CORADS score and effect of psychotropics especially antipsychotic medications like risperidone and aripiprazole in critical patients of COVID 19 admitted to ICU who had diagnosed with one or other neuropsychiatric sequalae. It was conducted in collaboration with department of psychiatry, pulmonology, emergency medicine and biochemistry of tertiary health care hospital and corporate hospital, Hyderabad, South India. The study was done between the duration of February 2021 to April 2021 after obtaining the ethical approval and consent from patient or their relatives.
Population and sample
All the patients less than 60 years old who were diagnosed as COVID 19 positive confirmed by Reverse Transcription Polymerase Chain Reaction (RT-PCR) on nasopharyngeal or oropharyngeal swab and had undergone HRCT and were admitted to the intensive care units with moderate to severe illness during these 3 months (February to April 2021, wherein the second wave of COVID 19 was at its peak in India) irrespective of their genders were included in the study. We excluded those who were not able to express their opinion or provide valid consent for study. An expert psychiatric referral was sought in the ICU for those who essentially developed one or other neuropsychiatric problems during their hospital stay. We screened non-probability sample of about 430 ICU patients out of whom 67 were diagnosed positively with definitive neuropsychiatric sequelae and received psychotropic intervention. The standard laboratory tests were administered as a part of the treatment protocol of COVID 19 and none of the patients were burdened with unnecessary or repeated evaluations. Routine blood analysis, D-dimer levels, C-reactive protein levels, serum ferritin, procalcitonin and Vit D levels were noted in the purposive sample of 67 patients. Neuropsychiatric evaluation for diagnosis and treatment were performed by consultant psychiatrist based on diagnostic and statistical manual-5 version of psychiatric classification system [22] and the severity of disorders were by Global Clinical Severity Scale [23]. Since plenty of factors like sleeplessness due to ICU disturbances, hypoxia, sepsis, cytokine surge and metabolic derangements could affect the quality of the response in an individual, we ensured that patients gets proper treatment for each of their disturbances using our multispecialty consultation-liaison model with at least twice daily patient visits and for the sake of convenience on day 5 to day 7 measurement of levels of biomarker(s) were taken up for assessment of variability between different neuropsychiatric disorders.
Data collection and analysis
All the data were analyzed using SPSS for windows version 23.0. Most of the evaluation of the data was conducted just before the time of the discharge of the patients who were apparently recovered during their stay at ICU while those patients who were still on ventilator or pregnant during the time of evaluations were excluded. Demographic data such age, gender, clinical diagnosis, psychiatric diagnosis, CORADS score, treatment received, and laboratory biomarkers were recorded. Categorical variables were evaluated by frequency and percentage while means and standard deviations were used for qualitative continuous variables. One-way ANOVA was used to identify the level of significance between mean value of biomarkers like D-dimers, serum ferritin, CRP levels, serum procalcitonin and Vit D levels with various psychiatric diagnosis. Finally, we conducted the linear regression analysis to identify the degree of co-variance explained with reference to significant laboratory biomarkers, CORDS scores and use of psychotropics in these neuropsychiatric sequelae. A p value of 0.05 was considered significant and less than 0.005 was considered very significant.
Outcome measures
The primary outcome measure was variability of clinical biomarkers and CORADS scores with severity of COVID-19 infections and the impact of psychotropic medications like risperidone and aripiprazole.
Results
The current study included in-patients who were hospitalised in a COVID clinic where neuropsychiatric examinations and face-to-face interviews were performed. During the study, we screened 430 ICU patients out of whom 67 were diagnosed positively with definitive neuropsychiatric sequelae and received psychotropic intervention during their stay in critical care unit. Out of 67, nearly four-fifth (n=53) were voluntary admissions (79.1%) and remaining (n=14) were emergency admissions (20.9%).The mean age of the patients was 42.38 years (SD+15.81), however majority (44.8%) of them belonged to 21-34 years with slight (52.2%) male preponderance and only 4.5% of them were less than 20 years old while none of them were more than 60 years. 37.3% (25 out of 67) of individual had significant history of alcohol dependence while hypertension and diabetes mellitus were noted in 34.3% (23 out of 67) and 29.9% (20 out of 67) respectively. The HRCT severity scores were screened, and it was found that nearly 46.3% of the COVID-19 patients moderate score and almost 28% of the participants scored severely on HRCT as noted in Table 1. On contrary, CORADS scoring were almost equivocally distributed from CORADS 3 to CORADS 6 throughout the sample. Among neuropsychiatric presentations, most (43.3%) had organic mood disorder and only 6.0% had organic psychosis whilecognitive decline in range of mild dementia and delirium were present in 6% and17.9% of ICU patients respectively. 45% of our patients were on aripiprazole or risperidone and about 40% were on one or other antidepressants while 15% were on cognitive enhancers.
Table 1: Socio-demographic and clinical parameters in the study group (N=67).
|
Variables |
N=67 |
% |
|
|
Age (years) |
10-20 years |
3 |
4.5 |
|
21-30 years |
16 |
23.9 |
|
|
31-40 years |
14 |
20.9 |
|
|
41-60 years |
13 |
19.4 |
|
|
Gender |
Male |
35 |
52.2 |
|
Female |
32 |
47.8 |
|
|
CORADS Staging (RT-PCR Positive) |
Corads 3 |
17 |
25.4 |
|
Corads 4 |
16 |
23.9 |
|
|
Corads 5 |
19 |
28.4 |
|
|
Corads 6 |
15 |
22.4 |
|
|
HRCT Severity |
Mild (<8) |
17 |
25.4 |
|
Moderate (9-14) |
31 |
46.3 |
|
|
Severe (>15) |
19 |
28.4 |
|
|
History of Alcohol Abuse/Dependence |
Present |
25 |
37.3 |
|
Absent |
42 |
62.7 |
|
|
Comorbid |
Present |
20 |
29.9 |
|
Diabetes Mellitus |
Absent |
47 |
70.1 |
|
Comorbid |
Present |
23 |
34.3 |
|
Hypertension |
Absent |
44 |
65.7 |
|
Psychiatric Diagnosis |
Organic Mood disorder |
29 |
43.3 |
|
Organic Anxiety disorder |
13 |
19.4 |
|
|
Organic Psychosis |
4 |
6 |
|
|
Delirium |
12 |
17.9 |
|
|
Mild Dementia/MCMD |
4 |
6 |
|
|
Substance Use disorders |
25 |
37.3 |
|
|
Functional Somatic Symptoms Disorder |
1 |
1.5 |
|
One way ANOVA was used to identify the significance of the association between various neuropsychiatric diagnosis ranging from organic mood disorders to mild dementia and their intergroup variance with D-dimer levels, CRP, serum Ferritin, Vit D, Procalcitonin as well as CORADS score on HRCT in ICU admitted COVID-19 patients. Among the clinical laboratory biomarkers only D-dimer levels were found to be significantly impacting the variability among various psychiatric diagnosis (F=2.479, p <0.033). while serum ferritin levels were just marginally close to significance (F= 2.221, p=0.053). We observed that serum CRP, Vit D levels and serum procalcitonin levels were not significantly variable between seven domains of psychiatric disorders. However, CORADS score on HRCT was quite significant (F= 4.432, p=<0.001) as the highest value of CORADS were present in organic psychosis and the lowest was in hypochondriacal disorder/somatic symptoms disorder as observed in Table 2.
Table 2: Intragroup relationship of laboratory biomarkers with psychiatric diagnoses using ANOVA test (N=67).
*p-value <0.05 is considered statistically significant
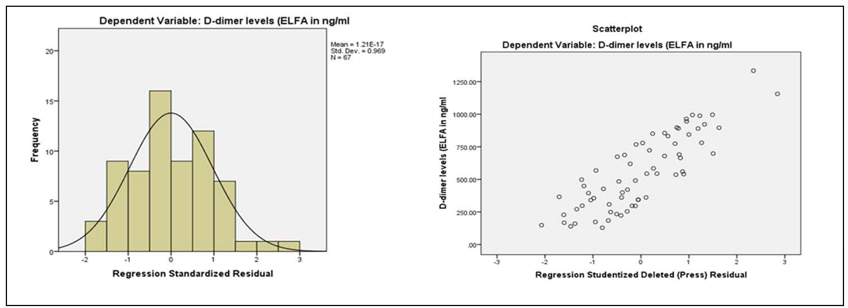
Table 3 showed Pearson’s correlation for quantitative laboratory biomarkers and CORADS score with psychiatric diagnosis during the course interval of ICU stay for any significant association. Only D-dimer levels were found to be significant and positively associated with psychiatric disorders (p<0.05). But, Vitamin D and procalcitonin levels were negatively correlated while serum ferritin and CRP levels were positively correlated to psychiatric diagnosis but none of them significantly (p>0.05). Further we conducted linear regression analysis of the significant D-dimer values as a dependent factor and evaluate for the degree of covariance with respect to use of psychotropics, CORADS score, psychiatric diagnosis and clinical outcome. Since all our patients recovered in due course secondary to psychotropic medications, our short-term outcome remained robust for their recovery irrespective of neuropsychiatric sequalae. We found almost 41% of covariance could be explained between D-dimer values, psychiatric outcome and CORADS score on HRCT very significantly as seen in Table 4 and scatterplot of D-dimer levels in Figure 1.
Discussion
The outbreak of SARS-COVID-2 posed more emphasis on respiratory and cardiovascular symptoms due to its association with mortality in COVID-19 patients but neuropsychiatric sequalae in survivors of COVID-19 is on rise as noted from
Table 3: Pearson’s correlation for quantitative evaluation of laboratory biomarkers and CORADS score with diagnosed psychiatric patients during course of ICU-Stay.
|
Biomarker (N=67) |
Psychiatric Diagnosis |
|
|
D-dimer levels (ELFA in ng/ml) |
Pearson Correlation |
0.144 |
|
Sig. (2-tailed) |
.048* |
|
|
Serum ferritin (CMIA method) |
Pearson Correlation |
0.244 |
|
Sig. (2-tailed) |
0.701 |
|
|
CRP levels |
Pearson Correlation |
0.125 |
|
Sig. (2-tailed) |
0.313 |
|
|
Vitamin D levels |
Pearson Correlation |
-0.031 |
|
Sig. (2-tailed) |
0.801 |
|
|
Serum Procalcitonin |
Pearson Correlation |
-0.024 |
|
Sig. (2-tailed) |
0.845 |
|
|
CORADS score on HRCT |
Pearson Correlation |
0.052 |
|
Sig. (2-tailed) |
0.678 |
|
*p-value <0.05 is considered statistically significant
hundreds of evidence-based emerging reports of neurological studies. Commonly noted neuropsychiatric abnormalities include disorders of consciousness, confusional syndromes like delirium, neurocognitive deficits, pressure of speech, insomnia, depression, anxiety and psychosis [11,14,24].
Table 4: Linear regression of various factors associated with d-dimer values.
|
Biomarker (N=67) |
Unstandardized Coefficients |
Standardized Coefficients |
T |
Sig. |
95.0% Confidence Interval for B |
||
|
B |
Std. Error |
Beta |
Lower Bound |
Upper Bound |
|||
|
CORADS score on HRCT |
136.925 |
33.089 |
0.526 |
4.138 |
.000* |
70.782 |
203.069 |
|
Use of Psychotropics(Risperidone and aripiprazole) |
5.352 |
23.809 |
0.028 |
0.225 |
0.823 |
-42.242 |
52.946 |
|
Psychiatric Diagnosis |
17.706 |
18.976 |
0.11 |
0.933 |
0.354 |
-20.226 |
55.639 |
|
Clinical Outcome |
-11.765 |
99.075 |
-0.016 |
-0.119 |
0.906 |
-209.813 |
186.283 |
*p-value <0.05 is considered statistically significant.
In the present cross-sectional prospective analysis of 67 neuropsychiatric patients admitted in ICU, we measured the levels of various biomarkers like serum D-dimer, ferritin, procalcitonin and Vitamin D along with CORADS scores with backdrop of psychotropics like risperidone, aripiprazole, fluoxetine, escitalopram, venlafaxine and cognitive enhancers like memantine and piracetam. Among all laboratory biomarkers, the mean D-dimer value showed significant rise in those patients with substance use disorder followed by organic psychosis, delirium and mood disorder. Further as expected, D-dimer levels were much lower in somatic symptoms or mild cognitive deficits correlating directly to levels of clinical and CORADS scoring. This reflects that D-dimer has robust potential for future clinical laboratory biomarker in neuropsychiatric disorders in COVID-19 patients.A meta-analysis by Yu et al showed higher (>0.5microgram/ml) D-dimer levels to be associated with progression of COVID-19 as well as with higher mortality rates [25]. Unfortunately, we could not compare the levels of D-dimer in patients who died in ICU as none of those patients received neuropsychiatric consultation as most of them were on mechanical ventilators, which otherwise could have provided us the comparative figures for D-dimer in survivors versus those who died of COVID-19 specifically if being measured on the day of death.
Paterson et a.l [26] in their emerging unique exploration in 33 COVID 19 patients for neurological, radiological and laboratory markers, could not find any distinctive abnormalities on MRI brain or CSF who developed delirium or psychosis in course of treatment [26]. Further, Kuzan et al. [27] lately compared 159 clinically diagnosed COVID 19 patients for laboratory biomarkers with diagnostic accuracy of CORADS and found high sensitivity but low specificity [27]. Similarly, in partial conformation to our study, Arshad AR et al evaluated 238 patients with SARS-CoV-2 with suggestive radiological findings and found that C-reactive protein, serum ferritin and lactate dehydrogenase levels of inflammatory biomarkers can predict mortality in these group of patients [28]. But there was no mention of any neuropsychiatric sequalae or psychotropic impact in their subjects and ours is perhaps the only study which integrated all these domains together. For each of neuropsychiatric disorders apart from global impression of severity, specificsymptom group severity scores or standardized mean differences could not be generated because control groups were not used in our study. Another limitation of our study lies in fact that 40% (26 out of 67) of our patients were also receiving steroids and later has the potential to cause mania or psychosis (0.7% causal prevalence) [29] but until a temporal causal association exists, it’s difficult to rule out the primary causality from COVID-19 brain involvement. It of worth to pinpoint the findings of Wang et al that those with chronic schizophrenic have lower association of COVID-19 severity compared to new onset psychosis or schizophrenia(AOR =1.48, 95% CI: 1.33–1.65 vs. AOR = 9.89,95% CI: 8.68–11.26), giving place to the speculation that antipsychotic treatment probably exerts a protective effect and specifically for aripiprazole which has the effect on gene expression modulation and could be of use in countering SARS-CoV-2 infection [21,23,30]. A separate analysis of immediate impact of aripiprazole on laboratory biomarkers would have actually identified better delineation which we could not conduct since it’s a preliminary observation study.D-dimer levels should have been measured at baseline in such dubious situations and also before the intervention of any psychotropic medication and then its impact would have been assessed systematically for severity and remission of neuropsychiatric presentations, however, given the circumstances of unpredictability of outcome in ICU admitted severe cases of COVID-19, its our first experience of evaluating biomarkers in neuropsychiatric disorders which would require to be cautious interpretations. Our study clearly has a few more limitations like small sample size and restrictive sample population, all being in- patient without any control group, which interferes with precocious generalizability of the results. We believe that a multicenter, large scale follow up studies in future will ensure to bridge and fill this important gap in evidence of identifying consistent biomarkers for organic psychiatric disorders and differentiating from functional presentations by enhancing their neurobiological underpinnings.
Conclusion
The serum D-dimer levels areparticularly increased in addictive, neurocognitive, and organic brain disorder more than others irrespective of CORADS or COVID-19 severity. Combining what we observed and tentatively inferred from impact of psychopathology on brain to the influence of psychotropics on clinical biomarker variability, we believe present study can potentially open up the new ways of conceptualizing mental health disorders, both organic and functional. Together with existing progress in preclinical, neurobiological and neuropsychopharmacological research, a ‘big data’ analytical approach with solid methodological strategies for range specificity across current diagnostic categories is warranted which can forward the field of biomarker development in psychiatric neurosciences [31].
Clinical Significance: We recommend implementing laboratory biomarker analysis in neuropsychiatric presentations and for evaluating the impact of psychotropic medications on these significant biomarkers like D-dimer levels in COVID-19 patients with further validations.
Conflict of Interest: None declared.
Source of Funding: Nil declared.
References
- Chawla R, Nasa P. Ventilatory management of COVID- 19-related ARDS: Stick to basics and infection control. Indian J Crit Care Med 24 (2020): 609-610.
- Stokes EK, Zambrano LD, Anderson KN, et Coronavirus disease 2019 case surveillance- United States, January 22-May 30, 2020. Morb Mortal Wkly Rep 69 (2020): 759-765.
- Notz Q, Schmalzing M, Wedekink F, et Pro- and Anti- Inflammatory Responses in Severe COVID-19-Induced Acute Respiratory Distress Syndrome-An Observational Pilot Study. Front Immunol 6 (2020): 581338.
- Richardson S, Hirsch JS, Narsimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 323 (2020): 2052-2059.
- Leng L, Cao R, Ma J, et al. Pathological features of COVID-19- associated lung injury: a preliminary proteomics report based on clinical Signal Transduction Targeted Ther 5 (2020): 1-9.
- Poggiali E, Zaino D, Immovilli P, et Lactate dehydrogenase and C-reactive protein as predictor of respiratory failure in Covid-19 patients. Clinica Chimica Acta 509 (2020): 135-138.
- Nalbant A, Kaya T, Varim C, et al. Can the neutrophil/ lymphocyte ratio have a role in the diagnosis of coronavirus 2019 disease? Rev Assoc Med Bras 66 (2020): 746-751.
- Mazza M, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain, Behavior, And Immunity 89 (2020): 594-600.
- Perrin P, Collongues N, Baloglu S, et Cytokine release syndrome associated encephalopathy in patients with COVID-19. European Journal of Neurology 28 (2021): 248-258.
- Dahan S, Segal G, Katz I, et al. Ferritin as a marker of severity in COVID-19 patients: A fetal correlation. Isr Med Assoc J 22 (2020): 494-500.
- Zhao YJ, Jin Y, Rao WW, et The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord 15 (2021): 145-157.
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta- analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7 (2020): 611-627.
- Helms J, Kremer S, Merdji H, et Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. Crit Care 24 (2020): 491.
- Montalvan V, Lee J, Bueso T, et Neurological manifestations of COVID-19 and other coronavirus infections: A systematic review. Clin Neurol Neurosurg 194 (2020): 105-921.
- Brun G, Hak J-F, Coze S, et COVID-19—White matter and globus pallidum lesions: Demyelination or small- vessel vasculitis?Neurol Neuroimmunol Neuroinflamm 7 (2020): e777.
- Matschke J, Lütgehetmann M, Hagel C, et Neuropathology of patients with COVID-19 in Germany: A post-mortem case series. Lancet Neurol 19 (2020): 919-929.
- Dinesh AA, Islam J, Khan J, et Effects of antipsychotic drugs: cross talk between the nervous and innate immune system. CNS Drugs 34 (2020): 1229-1251.
- Kato T, Monji A, Hashioka S, et Risperidone significantly inhibits interferon-gamma-induced microglial activation in vitro. Schizophr. Res 92 (2007): 108-115.
- Obuchowicz E, Bielecka-Wajdman AM, Paul-Samojedny M, et Different influence of antipsychotics on the balance between pro- and anti-inflammatory cytokines depends on glia activation: an in vitro study. Cytokine 94 (2017): 37-44.
- Juncal-Ruiz M, Riesco-Dávila L, Ortiz-García de la Foz V, et al. Comparison of the anti-inflammatory effect of aripiprazole and risperidone in 75 drug-naïve first episode psychosis individuals: a 3 months randomized study. Schizophr. Res 202 (2018): 226-233.
- Crespo-Facorro B, Ruiz-Veguilla M, Vázquez-Bourgon J, et al. Aripiprazole as a candidate treatment of COVID-19 Identified through Genomic Frontiers in Pharmacology 12 (2021): 646701
- American Psychiatric Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA: American Psychiatric Association (2013).
- Guy Clinical Global Impression. ECDEU Assessment Manual for Psychopharmacology, revised National Institute of Mental Health, Rockville, MD (1976).
- Nemani K, Li C, Olfson M, et Association of Psychiatric Disorders with Mortality Among Patients With COVID-19. JAMA Psychiatry 78 (2021): 380-386.
- Yu HH, Qin C, Chen M, et D-dimer level is associated with the severity of COVID-19. Thromb Res 195 (2020): 219-225.
- Paterson RW, Brown RL, Benjamin L, et The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings. Brain 143 (2020): 3104-3120.
- Kuzan TY, Murzoğlu Altıntoprak K, Çiftçi HÖ, et al. A comparison of clinical, laboratory and chest CT findings of laboratory-confirmed and clinically diagnosed COVID-19 patients at first Diagn Interv Radiol 27 (2021): 336-343.
- Arshad AR, Khan A, Shahzad K, et al. Association of inflammatory markers with mortality in COVID-19 Journal College Physician Surgeon Pakistan 30 (2020): S158-S163.
- Sheng B, Cheng SKW, Lau KK, et al. The effects of disease severity, use of corticosteroids and social factors on neuropsychiatric complaints in severe acute respiratory syndrome (SARS) patients at acute and convalescent Eur Psychiatry 20 (2005): 236-242.
- Wang Q, Xu R, Volkow Increased risk of COVID -19 infectionand mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry 20 (2021): 124-130.
- Pratt J, Hall Biomarkers in Neuropsychiatry: A prospect for the twenty-first century? Curr Top Behav Neurosci 40 (2018): 03-10.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 