Clinical Value of NT-proBNP and Performance Myocardial Index as an Echocardiographic Predictor of Early Cardiac Involvement in Patients with Carcinoid Syndrome
Ileana Nitu1,2*, Ionela Baciu1,2, Simona Galoiu1,2, Cristina Capatana1,2, Iulia Florentina Burcea1,2, Daniela Greere1,2, Catalina Poiana1,2
1C.I. Parhon” National Institute of Endocrinology, Bucharest, Romania
2Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania
*Corresponding author: Ileana Nitu, C.I. Parhon” National Institute of Endocrinology, Bucharest, Romania.
Received: 05 July 2021; Accepted: 15 July 2022; Published: 19 August 2022
Article Information
Citation: Ileana NiÈ›u, Ionela Baciu, Simona Găloiu, Cristina Căpățână, Iulia Florentina Burcea, Daniela Greere, Cătălina Poiană. Clinical Value of NT-proBNP and Performance Myocardial Index as an Echocardiographic Predictor of Early Cardiac Involvement in Patients with Carcinoid Syndrome. Archives of Clinical and Biomedical Research 6 (2022): 732-739.
View / Download Pdf Share at FacebookAbstract
Introduction: Carcinoid heart disease is a rare cause of right-sided valvular dysfunction, primarily mediated by serotonin. It is an important complication in patients with carcinoid syndrome which represents a major cause of morbidity and mortality.
Objectives: We aim to present our own experience regarding early myocardial dysfunction in patients with carcinoid syndrome by using predictive two-dimensional echocardiographic parameters and cardiac biomarkers.
Methods: 40 patients (35-90 year old, 62% female and 38% male patients; 20 non-hypertensive patients and 20 patients with arterial hypertension) with carcinoid syndrome and 20 healthy sex and age-matched subjects were consequently enrolled between October 2017 and June 2021. All patients underwent comprehensive two-dimensional echocardiography with additional tissue Doppler and speckle-tracking techniques. The Myocardial Performance Index (MPI) of both ventricles was calculated as (isovolumic contraction time “ICT”+ relaxation time “IRT”)/Ejection time “ET”. Besides, cardiac biomarkers (plasma level of pro-brain natriuretic peptide- NT-proBNP) were measured for each patient.
Results: Patients with carcinoid syndrome and arterial hypertension present higher values of MPI in comparison to non-hypertensive patients; moreover, all of the patients with carcinoid tumour tend to develop early myocardial dysfunction and higher MPI values than healthy subjects. This might be of particularly clinical interest in carcinoid syndrome with aggressive outcome.
Discussion: in the present study, higher values of MPI of both left and right ventricles, as well as plasma level of NT-proBNP proved to be of extremely importance in order to
Keywords
<p>Plasma; Gastrointestinal; Imaging; Carcinoid Syndrome; Echocardiographic</p>
Article Details
1. Introduction
Neuroendocrine neoplasia constitutes infrequent neoplasms that mostly originate from the gastrointestinal tract. They are reported in 2.5-5 persons per 100000 people [1].The secretion of vasoactive substances by these tumors is responsible for carcinoid syndrome [2].Carcinoid tumors usually develop gradually, over years, and are likely to show few or no symptoms until they are bulky enough to be symptomatic or have metastasized, mostly to the liver, followed by the skeletal and pulmonary systems [1,3]. One of the common complications of carcinoid syndrome is cardiac involvement due to the direct action of vasoactive substances. [2]Carcinoid syndrome can occur in up to 60% of cases during the course of the disease, but Carcinoid Heart Disease (CaHD) can be the first manifestation in approximately 20% of patients [3,4].As cardiac manifestations are associated with a poor long-term medical prospect and mortality,[3,5] the detection of cardiac disease in its early stages has a significant value. Cardiac surgeries such as valve replacement, if performed at the optimal time, significantly contribute to the treatment of symptomatic patients and the improvement of their quality of life [6].Transthoracic echocardiography is indicated in all patients diagnosed with carcinoid syndrome, and it should be performed on a routine basis every 3-6months depending on the clinical presentation of the patient and the severity of the disease [4].Cardiac involvement can vary widely in patients. In fact, all heart valves may be affected, but the involvement of the tricuspid valve is most common [5].Tricuspid leaflets show a specific involvement with thickened leaflets that have reduced mobility and are retracted. The concomitant regurgitation can vary from mild to severe [6-8].Right ventricular volume overload can result in these two valves becoming dysfunctional and can lead to right heart failure [9]. As serotonin produced by the carcinoid tumour is inactivated in the lungs, right-sided carcinoid heart disease is more frequent than left-sided heart involvement (>90% of the cases) [5,10].Therefore, the presence or absence of an atrial septum defect or a Patent Foramen Ovale (PFO) needs to be thoroughly evaluated, because in the presence of PFO, left heart valve involvement is more frequent. Cardiac magnetic resonance imaging and Computed Tomogaphy (CT) can be helpful tools to assess damage of heart structures, as well as to evaluate cardiac metastases. Nuclear medicine imaging may be useful to detect the primary tumour; however, it may be of limited use when diagnosing carcinoid heart disease, except for depicting cardiac metastases [11]. Right ventricular function is the primary determinant of prognosis and effort tolerance in many groups of patients. Clinicians require measures that are widely available, easily obtained, highly reproducible, and provide clear information on prognosis, likely response to therapy or provide feedback on the success of therapeutic interventions [11]. In addition to transthoracic echocardiography, biomarkers such as N-terminal pro-brain natriuretic peptide (NT-proBNP), which is a well-established marker for heart failure, has been shown to also have diagnostic and prognostic relevance in patients with carcinoid tumours [12].
2. Objectives
There is limited data on echocardiographic and Doppler indices of cardiac function as predictors for Congestive Heart Failure (CHF) in patients with carcinoid syndrome. Myocardial performance index (MPI, also denoted TEI-Doppler index) reflects both Left And Right Ventricular (LV, RV) systolic and diastolic function. We aim to present our own experience regarding early myocardial dysfunction in patients with neuroendocrine metastatic tumours by using predictive two-dimensional echocardiographic parameters and cardiac biomarkers.
3. Methods
Patients were enrolled regarding both inclusion and exclusion criteria. Study approval was provided by the Ethics Committee of “ Carol Davila” University of Medicine and Pharmacy, Bucharest. All procedures were in agreement with Helsinki declaration concerning ethical principles for medical research involving human subjects. After patient’s consent by completing an informed consent, a clinical evaluation and necessary investigation of each patient was carried out. Diagnosis of carcinoid disease was based on review of outside records, pathology specimens, thoracoabdominal computed tomography, and increased levels of 5-Hydroxyindole Acetic Acid (5-HIAA) in a 24-hour urine sample. The exclusion criteria were: age under 18 years old, ischemic heart disease, history of percutaneous coronary intervention, arrythmias, congenital heart disease, valvulopathies such as aortic and mitral stenosis, aortic and mitral regurgitation either rheumatic or degenerative, hypertrophic and restrictive cardiomiopathy, chronic kidney disease, peripheral artery disease, diabetes mellitus, Cushing syndrome, acromegaly, pregnancy and lactation, poor transthoracic windows. To ascertain that the patient had no exclusion criteria, the following prerequisites were performed: clinical evaluation, measurement of blood pressure, 12- leads electrocardiogram, serum creatinine and urea, serum ionogram and echocardiogram. 40 patients: 22 women and 18 men with median age= 63 years (range: 35-90 year old, 55% female with median age= 69.5 year old and 45% male patients with median age= 51 year old) with Carcinoid Syndrome (CS) were consequently enrolled between October 2017 and June 2021. Among these: 20 patients (mean age 56.0±4.16years) associated arterial hypertension (CS HTN group) and the other 20 (mean age 54.1±4.96years) had normal blood pressure (CS group). The control group includes 20 healthy subjects (mean age 54.9±3.99years). 2D and Doppler echocardiography was performed with standard techniques and equipment. All studies were performed by experienced sonographers and reviewed by staff cardiologists with advanced training in echocardiography. All patients underwent comprehensive two-dimensional echocardiography with additional tissue Doppler and speckle-tracking techniques, using commercially available echocardiography machines (General Electric Vivid-T8, EchoPac). All patients took the test several times in follow up, minimum 6 months apart, with a total number of explorations of 256 between October 2017 and June 2021 (160 explorations in women, 96 explorations in men).
Tissue Doppler Imaging (TDI) of themitral annuluswas obtained from the apical four-chamber view. A 1.5-mm sample volume was placed sequentially at the medial mitral annulus. Early diastolic velocityE′ was measured andE/E′ was calculate. TDI of the tricuspid annulus was obtained similarly. Myocardial performance index (MPI or Tei index) was calculated as follows: (isovolumic contraction time+isovolumic relaxation time)/RV ejection time. The mean normal value of the Tei index is 0.39±0.05 for the LV, while for theRight Ventricle(RV) it is 0.28±0.04. In adults, values of the LV index<0.40 and for the RV<0.30 are considered normal [10]. All pulsed Doppler tissue imaging parameters were measured on 4-6 consecutive heart cycles and mean value was calculated.
All patients had multiple plasma samples quantitatively analyzed for pro-brain natriuretic peptide (NT-proBNP). For this study, the highest values before or at the time of diagnosis of carcinoid disease were recorded. Blood samples were taken at the baseline visit. For NT-proBNP testing, plasma or serum was separated by centrifugation and aliquots were stored at − 80 °C. NT-proBNP was measured for each participant using the BNP Fragment EIA kit. NT-proBNP values were converted to pg/ml as recommended by current clinical practice guidelines. Furthermore, a statistical analysis was performed using IBM SPSS Statistics version 20. A simple regression, multinomial regression analysis and correlation tests were performed as appropriate to evaluate the relation between patients’ characteristics and echocardiographic and biochemical parameters.
4. Results
The clinical characteristics data are listed inTable 1. There was no significant difference between CS and control group as regards the age, sex, and blood pressure while blood pressure was significantly higher in CS HTN group when compared with either CS alone group or control group.
|
CS Group (n=20) |
CS HTN Group (n=20) |
Control Group (n=20) |
|||||
|
Age (years) |
54.1±4.96 |
56.0±4.16 |
54.9±3.99 |
||||
|
Men |
10 |
50% |
8 |
40% |
9 |
45% |
|
|
Women |
10 |
50% |
12 |
60% |
11 |
55% |
|
|
HTN Duration (years) |
- |
7.8 ±2.8 |
- |
||||
|
SBP (mmHg) |
125.1 ± 2.2 |
150 ± 6.5 |
121.2 ± 1.9 |
||||
|
DBP (mmHg) |
79 ± 3.4 |
89 ± 5 |
77 ± 3.8 |
||||
|
Data are means ± S.D. |
|||||||
Table 1: Clinical characteristics of the studied patients.
The parameters derived from pulsed wave myocardialTDIat the level of tricuspid and mitral annulus are listed inTable 2. Right and left ventricular myocardial performance indices (RV MPI, LV MPI) were significantly higher in carcinoid group (0.54 ± 0.14 versus 0.29±0.02; 0.48 ± 0.1 versus 0.273±0.04 ), and CS HTN group versus control group (0.58 ± 0.17 versus 0.29±0.02; 0.51± 0.09 versus 0.273±0.04). RV MPI and LV MPI were significantly higher in CS HTN group when compared with CS alone group. No significant correlation between RV MPI and LV MPI and HTN duration was found. NT-proBNP plasma levels were also compared between groups: significantly higher values were identified among CS HTN and CS patients versus control group, according to MPI (Table 2 ). Neither significant correlation between NT-proBNP level and HTN duration was found, nor between NT-proBNP and blood pressure.
|
Parameters |
CS Group |
CS HTN Group |
Control Group |
|
LV MPI |
0.48 ± 0.1 |
0.51± 0.09 |
0.273±0.04 |
|
RV MPI |
0.54 ± 0.14 |
0.58 ± 0.17 |
0.29 ± 0.02 |
|
NT-proBNP (pg/ml) |
261.18 ± 55 |
295.87 ± 62 |
93 ± 12 |
|
Data are means±S.D |
|||
Table 2: Comparative analysis of myocardial performance index and NT-proBNP plasma level in different groups.
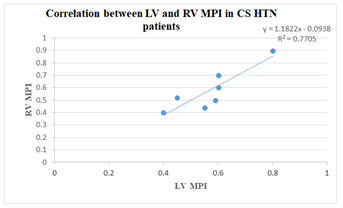
It has been reported that CS causes subclinical RV dysfunction. LV function could be affected by an impairedright ventricular function which is consistent with the idea that left ventricle might be also involved when vasoactive substances can’t be totally inactivated within the lungs [9]. The involvement of both ventricles in CS patients, suggest that this condition causes a global toxic effect on myocardial cells. Also the close correlation of the two ventricles as well as the sharing of theinterventricular septum, pericardium and ventricular interdependence may have a role [9,10]. These results suggest that the contributing effect of hypertension on RV function in carcinoid patients is not more than the effect of CS alone on RV function. This is concordant with Kosmola et al., who do not find any contributing effect of coexisting hypertension toRV dysfunctionin contrast to the LV [16]. The significant difference in MPI between CS and control group is indicative of the impairment of both RV systolic and diastolic functions in non-hypertensive carcinoid and carcinoid hypertensive patients. As other studies suggest, increasing NT-proBNP plasma level has a good performance in detecting of ventricular systolic function deterioration in long-term follow-up. Patients with higher NT-proBNP levels and higher myocardial performance indices showed significant risk of carcinoid heart disease with right heart failure during follow-up [10,11]. Moreover, plasma NT-proBNP and BNP reflect the degree of right ventricular overload in CS, even if there are no clinical signs of right heart failure. Elevated plasma levels of BNP/NT-proBNP are a potent predictor of poor survival in these patients [10]. Furthermore, we note that there is a correlation between left ventricle and right ventricle myocardial performance indices among hypertensive patients with CS (correlation coefficient of 0.91). Thus, this group of patients are prone to both left and right ventricle involvement, so this is important in clinical practice in order to assess subclinical myocardial dysfunction (chart 1).
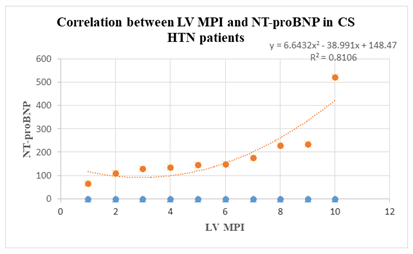
It can also be noticed that there is a correlation between left ventricle myocardial performance index and NT-proBNP values in carcinoid patients with arterial hypertension (correlation coefficient of 0.85). This is extremely important in clinical practice, left heart involvement being sometimes associated with high tumour burden (chart 2).
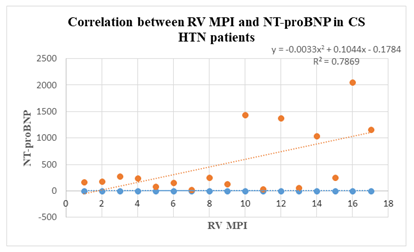
Moreover, there is also a correlation between right ventricle myocardial performance index and NT-proBNP values in CS HTN patients (correlation coefficient of 0.78). Echocardiographic and biochemical findings confirm that there is a strong predictibility to right heart involvement regarding this group (chart 3).
Regarding the gender-specific differences, there was no significant difference between men and women concerning the development of early myocardial dysfunction. There was no association between patients’gender, age, weight or body-mass index and grade of severity among tested patients.
5. Discussion
Cardiac dysfunction can manifest as both systolic as well as diastolic dysfunction, and routinely ejection fraction and conventional Doppler parameters are used for its evaluation. Ejection fraction is a less sensitive parameter in early systolic dysfunction and cannot be used routinely in asymptomatic patients. The sensitivity for the detection of diastolic dysfunction by conventional Doppler parameters is decreased by pseudonormalization pattern in Grade II diastolic dysfunction. This calls for the use of tissue Doppler-derived indices,i.e.,E/E′ for differentiation.
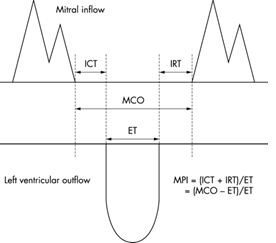
Figure 1: Schema for measurement of Doppler intervals. Myocardial Performance Index (MPI) is defined as the sum of Isovolumic Contraction Time (ICT) and Isovolumic Relaxation Time (IRT) divided by Ejection Time (ET). The sum of ICT and IRT is equal to the difference between the interval from cessation to onset of the Mitral Inflow (MCO) and ET. Myocardial Performance Index (MPI/Tei Index), which includes both systolic and diastolic time intervals to assess the global cardiac dysfunction was used by Tei and his co-workers in 1995. Tei Index uses the measurement possible on flow wave Doppler and is as sensitive as the tissue Doppler measurements. Tei index - myocardial performance index (MPI) is the ratio of the time spent in isovolumetric activity divided by the time spent in ventricular ejection [1]. In other words, it is the sum of isovolumic contraction and relaxation times divided by the ejection time [2].
MPI = (ICT + IRT) / ET
ICT: isovolumic contraction time; IRT: isovolumic relaxation time; ET: ejection time.
Tissue Doppler Imaging (TDI) is a relatively new echocardiographic technique that uses Doppler principles to measure the velocity of myocardial motion. We describe the principles behind and the clinical utility of TDI [16,17].
Doppler echocardiography relies on detection of the shift in frequency of ultrasound signals reflected from moving objects. With this principle, conventional Doppler techniques assess the velocity of blood flow by measuring high-frequency, low-amplitude signals from small, fast-moving blood cells. In TDI, the same Doppler principles are used to quantify the higher-amplitude, lower-velocity signals of myocardial tissue motion [18]. There are important limitations to TD interrogation. As with all Doppler techniques, TDI measures only the vector of motion that is parallel to the direction of the ultrasound beam. In addition, TDI measures absolute tissue velocity and is unable to discriminate passive motion (related to translation or tethering) from active motion (fiber shortening or lengthening). The emerging technology of Doppler strain imaging provides a means to differentiate true contractility from passive myocardial motion by looking at relative changes in tissue velocity [17,18]. The normal values of left and right ventricle differ. Due to the high pressures which must be generated by the LV, the isovolumic times of the LV are relatively long. The RV generates less pressure and therefore the index also lower with an average at around 0.28. A Tei index above 0.55 (TDI) is considered abnormal. Myocardial performance index has an inverse relation with global ventricular function in that increasing values indicate worsening global ventricular function. There is good correlation between Doppler derived myocardial performance index and cath derived invasive measures as well as with the clinical outcome. Myocardial performance index has different normal ranges for different age groups and for the left andright ventricles, though it is roughly a little more than one third. A prolonged Tei index - Myocardial performance index of more than 1.14 has been shown to be a powerful and independent predictor of poor clinical outcome in patients with severe left ventricular dysfunction and symptomatic heart failure [4]. Some of the advantages of the Myocardial Performance Index include that it is less dependent on heart rate and blood pressure and that it is not influenced by geometric changes of the ventricle. The MPI is an easily performable, recordable and reproducible parameter by flow Doppler. The standardization of MPI is not required as number of studies have documented that the MPI is independent of arterial pressure, heart rate, ventricular geometry, atrioventricular valve regurgitation, afterload, and preload in patients who are in a supine position [19-21]. This is the first study to show that the MPI reflects myocardial perfusion and that MPI can be used to predict the outcome of left ventricular systolic and diastolic function in patients with carcinoid syndrome [22-24]. LV systolic as well as diastolic dysfunction induces impaired relaxation (prolongation of isovolumic relaxation- IRT). The fact that both phases of LV function are simultaneously reflected in the diastolic parameter of the index (IRT) renders the index sensitive in the identification of impaired relaxation.Thus, MPI has a close correlation with diastolic hemodynamic indices of relaxation and appears superior to conventional diastolic parameters in the detection of impaired relaxation. MPI in our study group was significantly elevated in all grades of diastolic dysfunction. MPI in our study effectively differentiated the pseudonormalization from normal and it prolonged as degree of diastolic dysfunction increases [25-27]. Because of the potent systolic parameters that contribute to the MPI, such as isovolumic contraction- ICT and ejection time-ET, the index detects with reliability current alterations of LV systolic function. Index in our study showed a strong inverse relation with ejection fraction, the higher the value of the index, the lower the ejection fraction, andvice versa.The results were comparable to other studies [27,28]. The increase in both indices was mainly caused by isolated and significant prolongation of the IRT, the only diastolic component of MPI. The systolic components, isovolumetric contraction time and ejection time, showed no significant difference compared to the control group. IRT tends to increase in isolated left-ventricular diastolic dysfunction since early diastolic relaxation proceeds more slowly; however, its duration depends on both LV relaxation velocity and the difference between LV end-systolic pressure and left-atrial pressure, and occasionally it may shorten or pseudo-normalize with significant increases in left ventricular filling pressures. MPI appears more resistant to pseudonormalization, as increased LV filling pressures are correlated with shorter ejection times [29]. MPI is a simply measurable Doppler derived index of combined systolic and diastolic myocardial performance,which is easily applicable to the assessment of overall right and left ventricular myocardial function. In brief, left ventricular systolic dysfunction lengthens the pre-ejection period and shortens the ejection time, so that the pre-ejection period to ejection time ratio increases. The value of the time constant of left ventricular relaxation increases through all stage of diastolic dysfunction, so that isovolumic relaxation time becomes prolonged with abnormal relaxation. Shortened ejection time with premature mitral valve closure and prolongation of isovolumic contraction time compensate for increased left ventricular filling pressure. As a result, MPI increases and provides functional information. The advantages of this index are reported to be less dependence on the heart rate and blood pressure, no influence of geometric changes of the ventricle, easy quantitative assessment, suitability for follow up studies, and cost effectiveness.However, the MPI is unsuitable for the evaluation of left ventricular function in patients with atrial fibrillation, atrial flutter, atrioventricular block, severe mitral or aortic valvar disease, and severe pericardial effusion because these factors significantly influence the patterns of left ventricular inflow and outflow [27-29]. European Guidelines (2008) emphasized the role of Natriuretic Peptides (NP) as potential markers for heart failure. Therefore, NPs seem to be independent mortality predictors in patients with carcinoid heart disease. Although most studies showed that brain natriuretic peptide (BNP) is a marker with a higher sensivity and specificity; however the application of this analysis in clinical practice is often limited by the absence of a universally accepted normal range. A single determination of NT-proBNP at any time during the progression of carcinoid syndrome is a clinically useful tool for risk stratification. The hypothesis that repeated measurements could carry prognostic information beyond a single measure was confirmed in different settings. The importance of repeated determinations is in monitoring the progression of disease and in evaluating the clinical effects of medical therapy [28]. Arterial hypertension is accompanied by higher levels of NT-pro BNP, a reliable indicator of LV pressure and/or volume overload.NT-proBNP levels are closely associated with LV hypertrophy and filling impairment and may be used to facilitate the diagnosis of LV diastolic dysfunction in hypertensives [28].Wall thickness during arterial hypertension is the major compensatory mechanism to pressure overload and it is often associated with myocardial fibrosis collagen deposition and reduction in LV relaxation and distensibility.Experimental studies demonstrated that the genetic expression of NT-proBNP in myocardial tissue is one of the most important early indicators of LV pressure overload and it occurs before LV Hypertrophy (LVH) development [29].
Contemporary heart failure guidelines recommend natriuretic peptides as the biomarker of choice in diagnostic work-up of patients with heart failure [25]. In this regard, the diagnostic role of NT-proBNP is predominantly to exclude heart failure in carcinoid patients. In this present study, we confirmed NT-pro BNP, more stable counterpart of BNP as both diagnostic and prognostic marker that can largely influence decision making in framing treatment regimens for patients. NT-proBNP, 76 amino acid biologically inert molecule is generated by proteolytic cleavage by furin and corin, produced due to cardiomyocyte stress [23]. Inflammation, increased levels of oxidative stress and systemic angiogenic imbalance appear to play a crucial role in the pathophysiology of carcinoid heart disease. Through unknown mechanisms, increased levels of oxidative stress cause a cleavage of prolactin into a 16-kDa fragment, which causes endothelial dysfunction and induces cardiomyocyte apoptosis [23]. When interpreting NT-proBNP levels in heart failure, various clinical factors need to be considered. The level of natriuretic peptides increases with age, and therefore, higher cut-off values are suggested for the elderly. Whereas obesity lowers the concentration of natriuretic peptides, renal disease and atrial arrhythmias (Atrial Fibrillation(AF) in particular) are associated with higher NT-proBNPlevels. None of the patients in this cohort had AF; this was not surprising, as AF has previously been described to be rare in carcinoid disease [23].This will enable clinicians to start early and more specifically targeted treatment regimen. In addition to clinical judgement, NT-proBNP measurement may lead to a more effective combinational therapy. High serum NT-proBNP being indicative of increased risk of future cardiac dysfunction may enable clinicians to streamline more target oriented treatment, later followed by regular monitoring of clinical parameters. Although the left ventricle is considered the most important contractility chamber, several recent studies have shown the pivotal importance of RV function. Although initial studies showed that increased NT-proBNP levels were associated with the severity of LV dysfunction some authors have recently shown that patients with both RV and LV dysfunction have increased levels [29]. In our study carcinoid patients without hypertension have similar MPI values when compared with carcinoid syndrome and hypertension with no significant difference in parameters in patients with and without HTN. These results suggest that the contributing effect of hypertension on RV function in carcinoid patients is not more than the effect of carcinoid syndrome alone on RV function. The significant difference in MPI between CS and control group is indicative of the impairment of both RV systolic and diastolic functions in non-hypertensive carcinoid and carcinoid hypertensive patients. So in patients with early subclinicalcarcinoid heart disease, myocardial dysfunction is not confined to theright ventricle, but also involves the left ventricle, and the impairment of RV function encompasses both systolic and diastolic abnormalities. IncreasedNT-proBNP levels are associated with LV remodeling [24]. In this cohort, elevated levels of NT-proBNP tended to be associated with a higher MPI. Therefore, NT-proBNP bedside testing in patients with CS is an exciting prospect, especially in health care centres in low- and middle-income countries, where echocardiography is not readily available [29]. Because levels of brain natriuretic peptides are elevated significantly not only in pathologic conditions that affect the left ventricle but also in clinical conditions that lead to isolated acute or chronic right ventricular overload, it could be proposed that these peptides should not only be regarded as biomarkers of congestive heart failure, but also as indicators of carcinoid cardiovascular outcome [28,29]. The pathophysiological background of cardiac dysfunction in CS is multifactorial and may include both functional and structural alterations in heart muscle [28] In the present study, we have not found significant correlation between the duration of HTN and the RV and LV MPI. This study has some limitations. One is that the RV systolic function was evaluated withtransthoracic echocardiography. Other more accurate and objective methods to estimate RV systolic function, such as Magnetic Resonance Imaging (MRI), would have increased this study’s reliability. The other limitation is the study’s small population. Also data from large scale epidemiological studies regarding the application of Tei index are lacking.
6. Conclusion
The simple and easily obtained non-geometric MPI might be a strong predictor of subclinical myocardial dysfunction in patients with carcinoid syndrome; this echocardiographic parameter even correlates with cardiac biomarkers (NT-proBNP) in patients with neuroendocrine tumours, so this present study indicates the clinical feasibility and utility of MPI for assessing global right and left ventricular performance, incorporating both systolic and diastolic function. NT-proBNP can facilitate diagnosis and guides carcinoid heart disease therapy. Its increase is directly related to more advanced NYHA classes and to poor prognosis. However, the clinical application of these results requires further validation.
Declarations
Funding
No funding was received for conducting this study.
Conflicts of interest/Competing interests
The authors declare that there is no conflict of interest.
Ethics Approval
Study approval was provided by the Ethics Committee of “ Carol Davila” University of Medicine and Pharmacy, Bucharest
Consent to participate
A written informed consent was obtained from each participant
Consent for publication
Not applicable
Availability of data and material
All data generated or analyzed during this study are included in the published article.
Code of availability
Not applicable
References
- Riedel M, Jou CJ, Lai S, et al.Functional and pharmacological analysis of cardiomyocytes differentiated from human peripheral blood mononuclear-derived pluripotent stem cells.Stem Cell Reports 3 (2014): 131-141.
- Liu J, Backx PH.Patch-clamp technique in ESC-derived cardiomyocytes.Methods Mol Biol 1181 (2014): 203-214.
- Farre C, Fertig N.New strategies in ion channel screening for drug discovery: are there ways to improve its productivity? Expert Opin Drug Discov 9 (2014): 1103-1107.
- Poulin H, Bruhova I, Timour Q, et al.Fluoxetine blocks Nav1.5 channels via a mechanism similar to that of class 1 antiarrhythmics.Mol Pharmacol 86 (2014): 378-389
- Dobson R, Burgess MI, Pritchard DM, et al.The clinical presentation and management of carcinoid heart disease.Int J Cardiol 173 (2014): 29-32.
- Engelsman AF, van Duijvendijk P, Groenemeijer BE, et al.Tricuspid valve regurgitation as a presenting symptom of metastasized carcinoid tumor.Case Rep Gastroenterol 6 (2012): 643-649
- Chowdhury MA, Taleb M, Kakroo MA, et al.Carcinoid heart disease with right to left shunt across a patent foramen ovale: a case report and review of literature.Echocardiography 32 (2015): 165-169.
- Dashwood A, Rahman A, Pavicic M.Carcinoid heart disease.Eur Heart J 36 (2015): 2326.
- Bradette S, Papas K, Pressacco J.Imaging features of carcinoid heart disease.Can Assoc Radiol J 65 (2014): 214-217
- Patel C, Mathur M, Escarcega RO, et al.Carcinoid heart disease: current understanding and future directions.Am Heart J 167 (2014): 789-795.
- Simona Grozinsky-Glasberg ABG, Gross DJ.Carcinoid heart disease: from pathophysiology to treatment - ‘something in the way it moves’.Neuroendocrinology 101 (2015): 263-273.
- Catharina M, Korse BGT, de Groot CA, et al.Chromogranin-A and N-terminal pro-brain natriuretic peptide: an excellent pair of biomarkers for diagnostics in patients with neuroendocrine tumor.J Clin Oncol 27 (2009): 4293-4299.
- Lichtenauer M, Jirak P, Wernly B, et al.A comparative analysis of novel cardiovascular biomarkers in patients with chronic heart failure.Eur J Intern Med 44 (2017): 31-38.
- Schernthaner C, Lichtenauer M, Wernly B, et al.Multibiomarker analysis in patients with acute myocardial infarction.Eur J Clin Invest 47 (2017): 638-648.
- Jirak P, Fejzic D, Paar V, et al.Influences of Ivabradine treatment on serum levels of cardiac biomarkers sST2, GDF-15, suPAR and H-FABP in patients with chronic heart failure.Acta Pharmacol Sin 39 (2018): 1189-1196.
- Zurita AJ, Khajavi M, Wu HK, et al.Circulating cytokines and monocyte subpopulations as biomarkers of outcome and biological activity in sunitinib-treated patients with advanced neuroendocrine tumours.Br J Cancer 112 (2015): 1199-1205.
- Jirak P, Fejzic D, Paar V, et al.Influences of ivabradine treatment on serum levels of cardiac biomarkers sST2, GDF-15, suPAR and H-FABP in patients with chronic heart failure.Acta Pharmacol Sin 39 (2018): 1189-1196.
- Rachel P, Riechelmann AAP, Rego JFM, et al.Refractory carcinoid syndrome: a review of treatment options.Therapeutic Advances in Medical Oncology 9 (2017): 127-137.
- Castillo JG, Filsoufi F, Adams DH, et al.Management of patients undergoing multivalvular surgery for carcinoid heart disease: the role of the anaesthetist.Br J Anaesth 101 (2008): 618-626.
- Javier G, Castillo M, Federico Milla MD, et al.Surgical management of carcinoid heart valve disease.Semin Thoracic Surg 24 (2012): 254-260.
- IM Modlin, A Sandor. An analysis of 8305 cases of carcinoid tumors.Cancer 79 (1997): 813-829.
- M Kulke, R Mayer. Carcinoid tumors.N Engl J Med 340 (1999): 858-868.
- J Moller, P Pellikka, A Bernheim,et al. Prognosis of carcinoid heart disease: analysis of 200 cases over two decades.Circulation 112 (2005): 3320-3327.
- S Bhattacharyya, J Davar, G Dreyfus,et al. Carcinoid heart disease. Circulation 116 (2007): 2860-2865.
- Yeo TC, Dujardin KS, Tei C,et al.Value of a Doppler-derived index combining systolic and diastolic time intervals in predicting outcome in primary pulmonary hypertension.Am J Cardiol 81 (1998): 1157-1161.
- Szymanski P, Rezler J, Stec S,et al.Long-term prognostic value of an index of myocardial performance in patients with myocardial infarction.Clin Cardiol 25 (2002): 378-383.
- Botvinick EH, Perez-Gonzalez JF, Dunn R,et al.Late prognostic value of scintigraphic parameters of acute myocardial infarction size in complicated myocardial infarction without heart failure.Am J Cardiol 51 (1983): 1045-1051.
- Picano E, Sicari R, Landi P,et al.Prognostic value of myocardial viability in medically treated patients with global left ventricular dysfunction early after an acute uncomplicated myocardial infarction: a dobutamine stress echocardiographic study.Circulation 98 (1998): 1078-1084.
- Sicari R, Varga A, Picano E,et al.Comparison of combination of dipyridamole and dobutamine during echocardiography with thallium scintigraphy to improve viability detection.Am J Cardiol 83 (1999): 6-10.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 