Comparative Effectiveness of and Maternal Acceptability with Cervical Ripening using Cervical Massage Versus Membrane Sweep (CEASELESS): A Randomized Controlled Trial
Madugalle TMSSB*, Jayasundara DMCS
De Soysa Hospital for Women, Colombo, Sri Lanka
*Corresponding author: Madugalle TMSSB, De Soysa Hospital for Women, Colombo, Sri Lanka.
Received: 24 April 2022; Accepted: 02 May 2022; Published: 28 May 2022
Article Information
Citation: Madugalle TMSSB, Jayasundara DMCS. Comparative Effectiveness of and Maternal Acceptability with Cervical Ripening using Cervical Massage Versus Membrane Sweep (CEASELESS): A Randomized Controlled Trial. Archives of Clinical and Biomedical Research 6 (2022): 587-599.
View / Download Pdf Share at FacebookAbstract
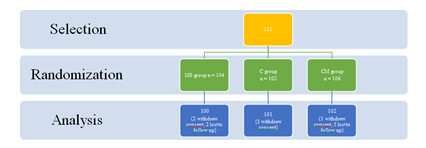
Methods: This randomized controlled non-blinded clinical trial conducted at a leading tertiary obstetric care unit in Colombo, Sri Lanka, compared the maternal acceptability and effectiveness of membrane sweep (MS) and cervical massage (CM) in ripening uterine cervix to avoid formal induction of labour. MS, CM, and control (C) groups had 104, 106 and 102 women after randomization. Primiparous women underwent either MS or CM at 39th and 40th weeks while multiparous women underwent at 40th week of gestation only. All were followed up until 24 hours postpartum. 100, 102 and 101 women in MS, CM and C groups respectively were included in the analysis.
Results: Overall, MS significantly improved Modified Bishop’s Score (MBS) to ≥7 compared to C (p=0.0310) but not compared to CM (p=0.2639). There was no significant improvement of MBS after CM compared to C (p=0.2795). Among primiparous (p=0.047) and multiparous (p=0.038) women separately, mean survival times without going into labour (MBS≥7) were significantly shorter after MS compared to C but not compared to CM. Hospital stay for delivery was less overall after both MS (p=0.0015) and CM (p=0.0197). There were no significant differences between MS, CM and C groups about synthetic oxytocin use, uterine hyperstimulation during labour, emergency cesarean section rate in labour, postpartum hemorrhage, maternal fever, and APGAR score at 5 minutes. Maternal acceptability was assessed using a validated questionnaire consisting of 4 Likert scale items (S-CVI = 0.875; Cronbach’s Alfa= 0.876). Maternal acceptability score of CM was significantly higher than that of MS during overall analysis as well as during subgroup analysis according to parity (p=0.0011).
Conclusions: MS is an effective adjunct to induction which ripens cervix, prevents formal induction
Keywords
<p>Cervical ripening; Induction of labour; Cervical massage; Cervical sweep; Membrane sweep; cervical priming; Mechanical methods of induction of labour</p>
Article Details
Abbreviations:
C: Control group; CM: Cervical massage MS – Membrane sweep; MBS: Modified Bishop’s Score; NNT: Number needed to treat; WHO-ICTRP: International Clinical Trials Registry Platform of the WHO
1. Introduction
WHO Global Survey on maternal and perinatal health reports that 9.6% of all deliveries start with an induction worldwide, and Sri Lanka tops the list at 35.5% [1]. Induction of labour is the artificial stimulation of the uterus to start labour and consists of initiation of uterine contractions and cervical ripening [2]. The phrase ‘induction of labour’ is sometimes used to denote the artificial initiation of contractions on a favorable cervix. And the phrase ‘cervical ripening’ is used to denote a separate process of achieving a Modified Bishop’s Score (MBS) of ≥7. In accordance to accepted definition of labour, it is logical to consider artificially initiating uterine contractions and cervical ripening as two components of process of induction of labour.
Methods of induction of labour are classified into mechanical and pharmacological categories. Mechanical methods of induction are membrane sweeping, cervical massage and balloon catheter. Principle of these mechanical methods of induction is to potentiate a local release of endogenous prostaglandin by physically stimulating the cervix. Pharmacological methods of induction introduce exogenous prostaglandin achieving high local concentrations at the cervix. Prostaglandin leads to dilatation, shortening and softening of cervix through complex interactions with cervical cells and matrix [3]. In addition, Prostaglandin acts on myometrial cellular receptors triggering rhythmic uterine contractions which are augmented by oxytocin [4, 5]. Balloon catheter, while not recommended for routine use by NICE, is widely utilized in Sri Lanka. Membrane sweep and cervical massage are considered as adjuncts to induction and not as formal methods of induction of labour in NICE guidance (CG70, 2008) 6. NICE recommends offering membrane sweep to nulliparous women at 40th and 41st weeks of gestation, to parous women at 41st week of gestation [6] and additional membrane sweeps offered as needed. NICE (CG70) also suggests that if the cervical OS is closed to admitting the examining finger, massaging around the cervix may achieve a similar effect. Boulvain et al
concludes on the utility of membrane sweeping towards avoiding formal induction of labour (number needed to treat
– 8) [7]. But there are hardly any studies comparing membrane sweep to cervical massage.
The theoretical framework of acceptability of a clinical intervention in seven-fold. It consists of, affective attitude, burden, perceived effectiveness, ethicality, intervention coherence, opportunity costs, and self-efficacy. Affective attitude is the emotional reaction to the intervention, for example “I feel scared when I think about the intervention”. Burden refers to the effort or toll taken by the health care system for the implementation of an intervention. Perceived effectiveness refers to the impression patients have about the effectiveness of an intervention. Ethicality means ensuring beneficence, non-maleficence, justice, and autonomy. Coherence of an intervention is the quality of being logical and consistent. Opportunity cost means the benefits lost elsewhere due to implementation of one intervention. Self-efficacy of an intervention refers to the ability of an intervention to achieve its aims on its own without and external compounding factors [8]. This randomized controlled non-blinded clinical trial compares the effectiveness and acceptability of cervical massage vs membrane sweep at cervical ripening.
2. Methods
This study was a non-blinded randomized controlled trial conducted in De Soysa Hospital for Women, Colombo 08, Sri Lanka from 20th February 2020 to 04th July 2020. Ethics approval was granted by the Ethics Review Committee of Faculty of Medicine, University of Colombo on 17th October 2019 for application no Protocol-19-064 [9]. Trial was registered in Sri Lanka Clinical Trials Registry which is a primary registry of the Registry Network of the International Clinical Trials Registry Platform of the WHO (WHO-ICTRP) since March 2008. (Registration No - SLCTR/2020/003, Date of registration – 22/01/2020, Universal Trial Number - U 1111-1244- 8026) [10]. Based on a study by Zamzami et al, where need of formal induction was 10% in the membrane sweep group compared to 25% in the control group, a 15% difference was considered of clinical importance [11]. The minimum sample size required to detect such a difference at an 80% statistical power and at a 95% confidence interval was 100 per group. Interventions compared were membrane sweep and cervical massage. Cervical Massage (CM) consisted of three circumferential passes of around the cervix massaging the cervix with examiner’s examining fingers for 15-30 seconds. Membrane Sweep (MS) involved insertion of the operator’s finger through the internal OS of cervix followed by three circumferential passes separating the chorio-amnion from the lower segment of the uterus 12. Ability to insert at least a part of one examining finger is a prerequisite for MS which was checked during screening to ensure all 3 interventions were possible in all women recruited. Principle investigator himself performed these interventions to ensure standardization throughout the study. MBS was confirmed to be ≤6 before initial intervention.
Pregnant women between 38 - 40 weeks of gestation attending antenatal clinic of Professorial Obstetrics and Gynaecology Unit of Faculty of Medicine of University of Colombo were given sequential pink numbers as they were registered. A set of random numbers between 1-500 were computer generated, sorted in ascending order, and compared with the given pink numbers to select a simple random sample. Throughout the screening process, 349
nulliparous and parous women in total were assessed for eligibility according to predetermined eligibility criteria (Table 1). Thirty- seven women were excluded according to exclusion criteria and 312 women were recruited and randomized into the three study groups. Membrane sweeping cervical massage and no intervention (C) was allocated to three computer generated sets of random numbers. Equal sized red colored cards were prepared with the random number and its allocated method of induction printed overleaf. These cards were kept locked in an opaque container in the ward. After a study participant signed the consent form, the next available sequential number was extracted, and the method mentioned was administered as the method of induction of labour.
|
Inclusion criteria Recruited women who, i. Had a gestational age more than 38 completed weeks, ii. Didn’t have a clear indication for elective or emergency caesarian section or early delivery iii. Had reassuring fetal condition, (Had normal fetal growth parameters, doppler values and a normal cardiotocogram) iv. Had a Modified Bishops’ Score ≤6, |
|
Exclusion criteria Women were not selected for recruitment if, i. There was an intra uterine fetal demise, ii. Their membranes were ruptured, iii. Her fetus had abnormal liquor amount, iv. Her fetus had severe fetal anomalies, v. Had any contraindication for induction of labor such as Cephalo-pelvic disproportion, obstructive pelvic mass, major degree placenta previa or morbidly adherent placenta. vi. Had latex allergies (Latex gloves were worn during certain procedures during the study). |
Table 1: Eligibility criteria.
The allocated method was performed once at 39th and once at 40th weeks of gestation for primiparous women and once at 40th week of gestation for multiparous women. Study participants were followed up as outpatients regularly till 40+6 weeks where an MBS ≤6 was considered a failure and a formal induction method was administered as per unit protocol. If participants went into labour (MBS ≥7) they were followed up throughout labour and up to 24 hours postpartum. There were no changes made to pre-defined outcome measures (Table 2).
|
Overall outcome measures i. Percentages of primiparous women who progress to spontaneous labour as defined by a Modified Bishops’ Score of ≥7 or 2≤ moderate uterine contractions per 10 minutes after cervical massage or membrane sweep by 40+6 weeks of gestation. ii. Percentages of multiparous women who progress to spontaneous labour as defined by a Modified Bishops’ Score of ≥7 or 2≤ moderate uterine contractions per 10 minutes after cervical massage or membrane sweep by 40+6 weeks of gestation. iii. Maternal acceptability in using membrane sweep or cervical massage for cervical ripening among primigravida and multigravida |
|
Specific outcome measures – Delivery outcomes i. Time from membrane sweep or cervical massage to onset on labour in hours (Modified Bishops’ Score ≥7 ii. Vaginal delivery rate by 40 weeks and by 40+6 weeks for primiparous women after membrane sweep and after cervical massage. iii. Vaginal delivery rate by 40+6 weeks for multiparous women after membrane sweep and after cervical massage iv. Emergency caesarian section rates in women who underwent cervical massage and membrane sweep respectively v. Percentage of oxytocin augmentation in women who underwent cervical massage and membrane sweep respectively Specific outcome measures - Maternal outcomes i. Percentage of uterine hyperstimulation ii. Percentage of post-partum hemorrhage iii. Percentage of maternal fever iv. Duration of hospital stay v. Maternal acceptability score Specific outcome measures – Neonatal outcomes i. Apgar Score at 5 minutes |
Table 2: Outcome measures.
Extensive fetomaternal safety measures were set in place. Participants were admitted for 24 hours for intervention and peri-intervention monitoring. A cardiotocogram and a clinical assessment of the woman was performed to ensure fetomaternal well-being prior to and 2 hours after each intervention. Uterine contractions, maternal body temperature and fetal heart rate were monitored every 4 hours till 24 hours. Safety protocols were set in place for participants to be withdrawn from the study in case of latex allergy, cervical tears, vasovagal attacks, uterine rupture,features of maternal or fetal infection or any psychological concerns. Any adverse event was to be reported to Data Safety Monitoring Board, Ethics Review Committee and managed as per unit protocols. Data Safety Monitoring Board comprised of two external consultant obstetricians and an external biostatistician.
Blinding was not possible in this trial because of the need to assess participant’s affective attitude and perceived effectiveness of each intervention. Principle author provided all participants detailed information on each intervention based on a template to ensure uniformity and completeness. Contingency table analysis and survival analysis was used to compare the effectiveness of membrane sweep and cervical massage in achieving a MBS ≥7 (spontaneous onset of labour) and avoiding formal induction. Demographic characteristics, mean MBS, mean birth weights, rates of emergency caesarean section, oxytocin augmentation, uterine hyperstimulation, postpartum bleeding, maternal pyrexia, duration of hospital stay, APGAR scores at 5 minutes, maternal acceptability scores were compared using chi square test. We conducted an overall analysis as well as subgroup analyses in terms of intervention and parity. There were no changes to methods and study protocol made after commencement of the study.
3. Results
MS, CM and C groups had 104, 106 and 102 participants after randomization. Four participants withdrew consent, 1 in CM group, 1 in C group and 2 in MS group. Three participants in CM group and 2 participants in MS group were lost to follow up because they had delivered at other hospitals. These participants were excluded from analysis leaving MS, CM and C groups with 100, 102, 101 participants respectively. MS group had 53 primiparous and 47 multiparous women. CM group had 61 primiparous and 41 multiparous women. C group had 54 primiparous and 47 multiparous women (Figure 01 – Participant flow). There were no statistically significant differences in demographic characteristics between the three study groups (Table 03). There was no delay between randomization and initiation of intervention. There were no abnormal physical examination findings and pathological cardiotocogram traces before or after the allocated intervention. Each participant was followed up till 24 hours postpartum, thus duration of follow up was unique to each participant. Trial was concluded after completion without any adverse events.
MS: Membrane sweep, CM: Cervical Massage, C: Control
|
Membrane sweep (MS) |
Cervical massage (CM) |
Control (C) |
P value at 95% confidence interval |
|
|
Overall |
N = 100 28.48 3.3257 3.66 1.2888 |
N = 102 28.0392 3.5681 3.5196 1.2565 |
N = 101 28.4554 3.7431 3.6436 1.3310 |
MS vs C - 0.9608 CM vs C - 0.4184 MS vs CM - 0.3650 MS vs C - 0.294 CM vs C - 0.4956 MS vs CM - 0.4340 |
|
· Number of participants |
||||
|
· Age |
||||
|
Mean Age |
||||
|
SD |
||||
|
· MBS at recruitment |
||||
|
Mean MBS |
||||
|
SD |
||||
|
Primiparous |
||||
|
· Number of participants · Age Mean Age SD · MBS at recruitment Mean MBS SD |
N = 53 26.91 2.574 2.87 1.057 |
N = 61 26.75 2.737 2.85 1.078 |
N = 54 26.82 2.860 2.72 0.998 |
MS vs C - 0.8646 CM vs C - 0.8936 MS vs CM - 0.7496 MS vs C - 0.4520 CM vs C - 0.5054 MS vs CM - 0.9208 |
|
Multiparous |
N = 47 30.26 3.200 4.55 0.880 |
N = 41 29.95 3.827 4.51 0.746 |
N = 47 30.68 3.401 4.70 0.750 |
MS vs C - 0.5390 CM vs C - 0.3461 MS vs CM - 0.6800 MS vs C - 0.3158 CM vs C - 0.2376 MS vs CM - 0.8201 |
|
· Number of participants |
||||
|
· Age |
||||
|
Mean age |
||||
|
SD |
||||
|
· MBS at recruitment |
||||
|
Mean MBS |
||||
|
SD |
Table 3: Demographic comparison at baseline.
Overall, MS significantly improved MBS to ≥7 compared to C (p=0.0310, RR – 1.4195, 95% CI– 1.0326 – 1.9513), unlike CM (p=0.2795, RR – 1.2043, 95% CI – 0.6359-1.6867, NNT - 13). The Number Needed to Treat (NNT) with MS was 7 to prevent one formal induction of labour. But MS did not improve MBS beyond ≥7 compared to CM (p=0.2639, RR – 1.1787, 95% CI – 0.8834 – 1.5727)). Subgroup analysis of primiparous and multiparous women separately demonstrated that neither MS nor CM was able to significantly improve MBS beyond
≥7 compared to C (Table 4).
|
SOL |
No SOL |
Total |
RR (95% CI) vs C |
NNT |
Percentage Of SOL |
P value at 95% CI (Compared to control) |
|
|
Overall |
|||||||
|
· MS |
52 |
48 |
100 |
1.4195 (1.0326-1.9513) |
7 |
52% |
MS vs C-0.0310 |
|
· CM · C |
45 37 |
57 64 |
102 101 |
1.2043 (0.6359-1.6867) MS vs CM 1.1787 (0.8834- 1.5727) |
13 |
44.12% 36.63% |
CM vs C-0.2795 MS vs CM P=0.2639 |
|
Primiparous |
|||||||
|
· MS |
28 |
25 |
53 |
1.3585 (0.8925-2.0678) |
7 |
52.83% |
MS vs C-0.1529 |
|
· CM · C |
28 21 |
33 33 |
61 54 |
1.1803 (0.7668-1.8168) MS vs CM 1.1509 (0.7928-1.6708) |
14 |
45.90% 38.89% |
CM vs C-0.4512 MS vs CM P=0.4598 |
|
Multiparous |
|||||||
|
· MS |
24 |
23 |
47 |
1.5000 (0.9222-2.4399) |
6 |
51.06% |
MS vs C-0.1024 |
|
· CM · C |
17 16 |
24 31 |
41 47 |
1.2180 (0.7104-2.0882) MS vs CM 0.8120 (0.5132 - 1.2849) |
13 |
41.46% 34.04% |
CM vs C-0.4734 MS vs CM P=0.3737 |
Table 4: Results of contingency table analysis and probability values.
Survival time was defined as the time duration between intervention and the first instance an MBS≥7 was detected. Survival times ranged from 18.5 to 336 hours among primiparous women and from 9.5 to 170 hours among multiparous women. Regardless of parity mean survival times of MS groups were significantly lower compared to C groups (Overall p=0.007, Primiparous p=0.047, Multiparous p=0.038). There were no such differences between CM and C groups as well as MS and CM groups (Table 5, Figure 2, 3, 4).
|
Comparison |
MS |
CM |
C |
|
Overall · Mean survival time · Chi square · Df · Sig (Long Rank – Mantel Cox) |
221.616 7.278 1 MS vs C - 0.007 |
255.871 1.266 1 CM vs C – 0.261 |
278.627 2.619 1 MS vs CM - 0.106 |
|
Primiparous · Mean survival time · Chi square · Df · Sig (Long Rank – Mantel Cox) |
260.651 3.938 1 MS vs C - 0.047 |
276.262 1.220 1 CM vs C - 0.269 |
308.491 0.805 1 MS vs CM – 0.370 |
|
Multiparous · Mean survival time · Chi square · Df · Sig (Long Rank – Mantel Cox) |
155.888 4.288 1 MS vs C - 0.038 |
142.171 0.556 1 CM vs C – 0.456 |
148.106 1.742 1 MS vs CM – 0.187 |
Table 5: Log rank test for survival plots of all women in MS, CM and C.
Figure 2: Survival functions – overall.
Figure 3: Survival functions – primiparous.
Figure 4: Survival function – multiparous
Overall and among multiparous women, both MS and CM significantly reduced the total duration of hospital stay for delivery (MS vs C – p=0.0015, 95%CI 0.1752-0.7166; CM vs C – p=0.0197,95%CI 0.0603-0.6757) compared to C.
Neither MS nor CM was able to reduce the hospital stay for delivery among primiparous women. Between MS, CM and C groups overall there were no significant differences with regards to synthetic oxytocin use, uterine hyperstimulation during labour, emergency cesarean section rate in labour, postpartum hemorrhage, maternal fever, and APGAR score at 5 minutes (Table 6).
|
Factor |
Comparison |
MS |
CM |
C |
|
Number of participants |
Total Primiparous multiparous |
52 28 24 |
45 28 17 |
37 21 16 |
|
Synthetic oxytocin use |
Overall Rate Significance p Primiparous Rate Significance p Multiparous Rate Significance p |
42/52 MS vs C - 0.0614 25/28 MS vs C - 0.1255 17/24 MS vs C - 0.2220 |
41/45 CM vs C - 0.5496 27/28 CM vs C - 0.3866 14/17 CM vs C – 0.6847 |
35/37 MS vs CM - 0.1505 21/21 MS vs CM – 0.3038 14/16 MS vs CM – 0.4033 |
|
Uterine hyperstimulation |
Overall Rate Significance p Primiparous Rate Significance p Multiparous Rate Significance p |
6/52 MS vs C – 0.5989 3/28 MS vs C – 0.8928 3/24 MS vs C – 0.5239 |
3/45 CM vs C – 0.8044 1/28 CM vs C - 0.3947 2/17 CM vs C – 0.5879 |
3/37 MS vs CM – 0.4122 2/21 MS vs CM – 0.3038 1/16 MS vs CM – 0.9438 |
|
Emergency Cesarean sections |
Overall Rate Significance p Primiparous Rate Significance p Multiparous Rate Significance p |
5/52 MS vs C – 0.2020 4/28 MS vs C – 0.2804 1/24 MS vs C – 0.4140 |
6/45 CM vs C – 0.0884 5/28 CM vs C – 0.1706 1/17 CM vs C – 0.3321 |
1/37 MS vs CM – 0.5675 1/21 MS vs CM – 0.7185 0/16 MS vs CM – 0.8047 |
|
Postpartum hemorrhage |
Overall Rate Significance p Primiparous Rate Significance p Multiparous Rate Significance p |
0.52 MS vs C – 0 0/28 MS vs C – 0 0/24 MS vs C - 0 |
2/45 CM vs C – 0.1972 1/28 CM vs C – 0.6492 1/17 CM vs C – 0.3321 |
0.37 MS vs CM – 0.1267 0/21 MS vs CM – 0.5991 0/16 MS vs CM – 0.2349 |
|
Maternal fever |
Overall Rate Significance p Primiparous Rate Significance p Multiparous Rate Significance p |
4/52 MS vs C – 0.3136 2/28 MS vs C – 0.7335 2/24 MS vs C – 0.2422 |
0/45 CM vs C – 0.2703 0/28 CM vs C – 0.2483 0/17 CM vs C – 0 |
1/37 MS vs CM – 0.0588 1/21 MS vs CM – 0.1536 0/16 MS vs CM – 0.2281 |
|
APGAR at 5 minutes |
Overall Mean SD Significance p Primiparous Mean SD Significance p Multiparous Mean SD Significance p |
9.8269 0.5503 MS vs C – 0.5772 9.8929 0.4163 MS vs C – 0.9231 9.75 0.6757 MS vs C – 0.7612 |
9.8222 0.5756 CM vs C – 0.5737 9.7857 0.6299 CM vs C – 0.4616 9.8823 0.4851 CM vs C – 0.6946 |
9.8649 0.5851 MS vs CM – 0.9673 9.9048 0.4364 MS vs CM – 0.4557 9.8125 0.75 MS vs CM – 0.4037 |
|
Duration of hospital stay for delivery |
Overall Mean SD Significance p 95% CI Primiparous Mean SD Significance p Multiparous Mean SD Significance p 95% CI |
2.5 0.6104 MS vs C – 0.0015 0.1752 – 0.7166 2.5357 0.6926 MS vs C – 0.5068 2.4583 0.5090 MS vs C - <0.0001 0.5293 – 1.1791 |
2.5778 0.7226 CM vs C – 0.0197 0.0603 – 0.6757 2.75 0.7993 CM vs C – 0.6993 2.2941 0.4697 CM vs C – <0.0001 0.6816 – 1.3552 |
2.9459 0.6644 MS vs CM – 0.5667 2.6667 0.6583 MS vs CM – 0.2885 3.3125 0.4787 MS vs CM – 0.2151 |
Table 6: Comparison of study outcomes.
Maternal acceptability was assessed using a validated questionnaire consisting of 4 Likert scale items (S-CVI = 0.875; Cronbach’s Alfa = 0.876). Mean overall acceptability scores of MS and CM were 11.4400 and 13.2642 respectively (Table 7). Maternal acceptability score of CM was significantly higher than that of MS during overall analysis as well as during subgroup analysis according to parity (p=0.0011, 95% CI - 0.7349 to 2.9145).
|
Group |
MS |
C |
P value at 95% CI |
|
Overall Mean SD N |
11.4400 3.9500 100 |
13.2647 3.9046 102 |
0.011 (0.7344 – 2.9140) |
|
Primiparous Mean SD N |
8.6415 2.4502 53 |
11.5082 3.7755 61 |
0.0001 (1.6655 – 4.0679) |
|
Multiparous Mean SD N |
14.5957 2.7556 47 |
15.8780 2.3259 41 |
0.0216 (0.1928 – 2.3718) |
Table 7: Maternal acceptability scores.
4. Discussion
This study compares commonly performed hitherto un-standardized membrane sweep and cervical massage as adjuncts to induction of labour, suggests standardization and supports its incorporation into evidence based clinical practice. Techniques of MS and CM used in this study are easily practicable in ward. A standard obstetric unit is usually equipped to manage possible common complications of MS and CM such as latex allergy, cervical tears, vasovagal attacks, uterine rupture, features of maternal or fetal infection or any psychological concerns. Simple random sampling was selected to counter selection bias and increase external validity and generalizability. Higher proportion of pregnant women overall went into labour spontaneously after MS than without any intervention regardless of parity. Smaller the NNT, higher the effectiveness of the intervention and NNT for MS is 7 to prevent one formal induction of labour. Size of subgroups (primiparous – n=53 in MS group, n=61 in CM group; multiparous – n=47 in MS group, n=41 in CM group) being too small may be the reason for not detecting any significant improvement in MBS. Larger studies powered to detect these differences are required. After MS, women went into spontaneous labour within a shorter period compared to C regardless of parity. CM was unable to hasten spontaneous onset of labour compared to C. At a glance, survival distribution of MS among primiparous women demonstrated a higher event rate (steeper slop) in the second half of the plot compared to the first half. This is probably due to the additive effect of the second MS administered at 40th week of gestation to women who had not yet progressed into spontaneous labour. No such effect was seen in the primiparous CM group plot. Further studies comparing the effects of a single intervention compared to repeated interventions and the ideal interval between two such interventions are required. We measured survival time from intervention until the first moment an MBS ≥7 was detected. Cervical dilatation at that point ranged between 3cm – 10cm. Therefore, it was obvious that the speed of cervical dilatation differed among women. We did not study how fast each method dilated the uterine cervix in this study. Designing such a study would be difficult because it requires prolonged admission and repeated vaginal examinations inconveniencing women and increasing the risk of infections, discomfort, withdrawal of consent, dropout from the study, emergency cesarean sections, fetal and maternal distress. Both MS and CM reduced the duration hospital stay for delivery compared to C among multiparous women only.
5. Conclusions
MS is an effective adjunct to induction which ripens uterine cervix, prevents formal induction of labour (NNT = 7) and significantly reduces the duration of pregnancy regardless of parity. It shortens hospital stay of multiparous women admitted for delivery as an added advantage. Although CM is more acceptable to pregnant women than MS and shortens hospital stay of multiparous women admitted for delivery it is not an effective method to ripen the uterine cervix or to prevent formal induction labour regardless of parity.
Declarations
Ethics Approval and consent to participate
Ethics approval was granted by the Ethics Review Committee of Faculty of Medicine, University of Colombo on 17th October 2019 for application no Protocol-19-064. The study was performed in accordance with all the relevant guidelines and regulations adhering to the approved study protocol. Informed consent was obtained from all study participants by the principal investigator.
Consent for publication
Not applicable
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
None declared
Funding
This study was self-funded
Author’s contributions
TMSSBM designed, conducted the study and analyzed data. D. M. C. S. J. supervised the study and contributed to writing this article.
Acknowledgements
Special thanks to Dr. C Muthukuda MBBS, MSc for invaluable advice on statistical analysis.
Reference
- World Health Organization. WHO handbook for guideline development, 2nd ed. World Health Organization (2014).
- World Health Organization. Managing complication in pregnancy and childbirth: a guide for midwives and doctors, 2nd edition (2017).
- Leduc D, Biringer A, Lee L. Dy J. Induction of labour. Journal of Obstetrics and Gynecology Canada 35 (2013): 840-857.
- Edmonds DK. Dewhurst’s Textbook of Obstetrics and Gynecology. 8th edition. Wiley Blackwell.
- Standring S. Gray’s Anatomy: The anatomical basis of clinical practice. 41st Edition. Elsevier (2016).
- National Institute of Clinical Excellence. Inducing labour, National Institute of Clinical Excellence (2008).
- Finucane EM, Murphy DJ, Biesty LM, et al. Membrane sweeping for induction of Cochrane Database of Systematic Reviews (2020).
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 17 (2017):
- Ethics review Committee of Faculty of Medicine, University of Colombo, Sri
- Sri Lanka Clinical Trials
- Zamzami T, AL Senani N. The Efficacy of Membrane Sweeping at Term and Effect on the Duration of Pregnancy: A Randomized Controlled Trial. Journal of Clinical Gynecology and Obstetrics, North America 3 (2014).
- Hamdan M, Sidhu K, Sabir N, et al. Serial Membrane Sweeping at Term in Planned Vaginal Birth After Cesarean: A Randomized Controlled Trial. Obstetrics & Gynecology 114 (2009): 745-751.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 