Comparative Study between the Functional Outcome of Arthroscopic Reconstruction of Anterior Cruciate Ligament Tear by Quadriceps and Peroneus Longus Tendon Autograft
Dr. Md. Nazrul Islam1*, Prof. Dr. Abu Zaffar Chowdhury2, Dr. Chowdhury Iqbal Mahmud2, Dr. Debashish Dey1, Dr. Md. Golam Shaikh Ferdous1, Dr. Aynun Nahar Rabeya Diba2, Dr. Aminur Rasul1
1DGHS, Deputed to Bangladesh Medical University, Dhaka, Bangladesh
2Department of Orthopaedic, Bangladesh Medical University, Dhaka, Bangladesh
*Corresponding Author: Dr. Md. Nazrul Islam, DGHS, Deputed to Bangladesh Medical University, Dhaka, Bangladesh; E-mail: dr.nazrul06@gmail.com
Received:10August2025; Accepted:20 August 2025; Published:27August2025
Article Information
Citation: Md. Nazrul Islam, Abu Zaffar Chowdhury, Chowdhury Iqbal Mahmud, Debashish Dey, Md. Golam Shaikh Ferdous, Aynun Nahar Rabeya Diba, Aminur Rasul. Comparative Study between the Functional Outcome of Arthroscopic Reconstruction of Anterior Cruciate Ligament Tear by Quadriceps and Peroneus Longus Tendon Autograft.Journal of Orthopedics and Sports Medicine. 7 (2025): 428-434.
View / Download Pdf Share at FacebookAbstract
Background: Anterior Cruciate Ligament Reconstruction (ACLR) is among the most frequently performed orthopedic procedures globally. Despite its prevalence, controversy persists regarding the optimal graft choice. Recently, alternative grafts such as Quadriceps Tendon (QT) and Peroneus Longus Tendon (PLT) have gained attention over the traditional Hamstring graft.
Aim of the study: To compare the functional outcomes, graft characteristics, and donor-site morbidity of arthroscopic ACLR using QT versus PLT autografts.
Methods: A prospective comparative study was conducted on 36 patients with isolated ACL injuries at the Department of Orthopaedic Surgery, BSMMU, Dhaka, between September 2022 and September 2024. Patients were equally allocated into two groups: QT (n = 18) and PLT (n = 18). Functional outcomes were assessed preoperatively and at 1, 3, 6, and 12 months postoperatively using the Lysholm and IKDC subjective scores. Donor site morbidity in the PLT group was evaluated using the AOFAS score. Statistical significance was set at p < 0.05.
Result: The comparative study had a mean age of 28.44 ± 5.70 years (range, 20–42), with a male predominance of 83.3%. The right knee was involved in 63.9% of cases, and injuries primarily resulted from road traffic accidents (47.2%) and sports-related trauma (44.4%). The mean interval from injury to surgery was 5.08 ± 3.37 months, and preoperative demographic and clinical parameters were comparable between the QT and PLT groups. The QT group demonstrated a significantly larger graft diameter than the PLT group (8.53 ± 0.56 mm vs. 8.08 ± 0.43 mm; p = 0.027). Both groups showed significant improvements in Lysholm (QT: 90.11 ± 3.72; PLT: 91.61 ± 3.17) and IKDC scores (QT: 89.22 ± 4.33; PLT: 90.56 ± 4.39) at final follow-up, without significant intergroup differences. Knee range of motion was slightly higher in the PLT group (136.11 ± 3.23° vs. 132.50 ± 5.75°), and donor site morbidity remained low (AOFAS: 95.11 ± 3.69). Complications occurred in 27.8% of QT and 11.1% of PLT patients, with excellent outcomes achieved in 77.8% and 88.9%, respectively.
Conclusion: Arthroscopic ACLR using QT or PLT autografts provides excellent functional improvement. The PLT group demonstrated slightly better functional outcomes and lower donor-site morbidity, whereas the QT group offered a larger graft diameter. Both graft options are viable alternatives to traditional Hamstring grafts.
Keywords
<p>Anterior cruciate ligament reconstruction; Quadriceps tendon; Peroneus longus tendon; Functional outcome;Donor-site morbidity</p>
Article Details
1. Introduction
The knee joint is commonly injured due to its anatomical structure susceptibility to external forces and the functional requirements placed on it. Twisting knee injury often results in ligament tears [1]. The anterior cruciate ligament (ACL) is a crucial ligament that helps to stabilize the knee joint. However, it is also a common structure injured in the knee leading to permanent and severe impairments due to its significant role in knee function. Approximately 70% of cases of acute traumatic hemarthrosis resulting from sports injuries are attributed to the risk of partial or complete ACL tears. Anterior instability can develop over time as a result of acute or chronic ACL failure [2]. The ACL comprises two bundles that work together; the anteromedial (AM) bundle which is taut when the knee is bent while the posterolateral (PL) bundle is taut when the knee is straight. When a single-bundle (SB) ACL reconstruction is performed, it replicates the structure and movement of the AM bundle. Though traditional SB reconstruction typically yields satisfactory outcomes, issues related to rotational instability and long-term effects of degenerative changes still exist [3].The classic mechanism of injury involves deceleration or sudden changes in direction without contact. ACL reconstruction remains the preferred approach to reduce instability and prevent cartilage or meniscal damage in active individuals. Graft choice depends on factors such as activity level, concomitant injuries, expected outcomes, surgeon preference, age, gender, and donor-site morbidity. Grafts are broadly classified as autografts, allografts, or synthetic. Common autografts include bone–patellar tendon–bone (BPTB) and hamstring tendon (HT), with peroneus longus (PL) and quadriceps tendon (QT) gaining popularity. Initially limited by concerns over postoperative quadriceps weakness, quadriceps tendon grafts were mainly used in revisions but have gained attention for their effectiveness and lower donor-site morbidity. Morphometric and biomechanical studies support the quadriceps tendon as a viable alternative to bone–patellar tendon–bone grafts [4]. QT ACL reconstruction yields lower knee extensor but greater flexor strength than HT reconstruction, making knee strength outcomes an important consideration when selecting a QT graft [5]. Peroneus longus tendon (PLT) has been proposed as a viable autograft option for ACLR in some research. Its size is sufficient and biomechanical assessments have indicated that it possesses the necessary strength for ACLR [6]. Also, a PLT graft provides several advantages compared to traditional grafts. PLT has similar strength and biomechanical properties to native ACL [7]. There is minimal donor site morbidity as the peroneus brevis can compensate for its absence. The weakness of the hamstring or quadriceps muscle following its use as a graft is less likely with a peroneus longus graft which can enhance the rehabilitation process [8]. The aim of this study is to evaluate and compare the functional outcomes, ligamentous stability, graft characteristics, knee scores, and peri-operative events following arthroscopic anterior cruciate ligament reconstruction using Peroneus Longus Tendon versus Quadriceps Tendon autografts.
2. Methodology and Materials
This quasi-experimental study was conducted from September 2022 to September 2024 in the Department of Orthopaedic Surgery, Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbagh, Dhaka, Bangladesh.
2.1 Study Population and Sampling
Patients with isolated ACL tears attending the outpatient department (OPD) of the Department of Orthopaedic Surgery, BSMMU, during the study period were recruited using purposive, non-randomized sampling. A total of 36 patients met the eligibility criteria and were enrolled. Allocation to study groups was performed using an odd–even technique based on the serial number of admissions:
- • Odd-numbered patients: Quadriceps Tendon (QT) group
- • Even-numbered patients: Peroneus Longus Tendon (PLT) group
2.2 Inclusion Criteria
- Age between 20 and 45 years.
- Both male and female patients.
- Body mass index (BMI) less than 40 kg/m².
- Diagnosed case of symptomatic isolated ACL tear confirmed clinically and radiologically.
2.3 Exclusion Criteria
- Patients with associated meniscus, cartilage, or posterior cruciate ligament injuries.
- Bilateral ACL deficiency.
- Multiple ligament injuries of the knee.
- Ipsilateral ankle injuries.
- History of previous knee or ankle surgery.
- Fractures around the knee (femoral condyle, tibial plateau, patella).
- Presence of knee osteoarthritis.
- Knee sepsis or loss of knee motion due to acute injury.
- Patients unable to provide informed consent or uncooperative.
2.4 Preoperative assessment
After obtaining informed consent, a detailed history and thorough physical examination were performed for each patient. Baseline investigations included plain radiographs of the affected knee joint (anteroposterior and lateral views) and magnetic resonance imaging (MRI) to confirm isolated ACL injury. Standard preoperative investigations for anesthesia and surgical fitness were completed prior to surgery.
2.5 Surgical procedure
All procedures were performed by a single experienced orthopaedic surgeon under spinal anesthesia using standard arthroscopic techniques. Intraoperative details—including graft harvesting, tunnel preparation, fixation techniques, and perioperative complications—were meticulously recorded.
- • Quadriceps Tendon Autograft (QT group): A central portion of the quadriceps tendon was harvested. The graft was prepared to the appropriate length, diameter and secured using Endo-button on the femoral sides and interference screws on the tibial sides.
- • Peroneus Longus Tendon Autograft (PLT group): The peroneus longus tendon was harvested via a small lateral incision at the distal leg. The graft was doubled to achieve the desired thickness and fixed with standard femoral and tibial fixation techniques.
2.6 Data collection and outcome masures
Data were collected using a structured case record form. Functional outcomes were assessed using the Lysholm Knee Scoring Scale and the International Knee Documentation Committee (IKDC) subjective score. Donor site morbidity at the ankle (for PLT group) was evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) score. Patients were followed up postoperatively at 1 month, 3 months, 6 months, and 12 months. At each follow-up, clinical examination, radiological assessment, and functional outcome were recorded. Any post-operative complications were documented.
2.7 Statistical analysis
Data were analyzed using IBM SPSS Statistics version 26. Qualitative variables were expressed as frequency and percentage and analyzed using the chi-square test. Quantitative variables were expressed as mean ± standard deviation and analyzed using Student’s t-test for parametric data and Mann–Whitney U test for non-parametric data. A p-value of <0.05 was considered statistically significant, and a 95% confidence interval was applied.
2.8 Ethical considerations
The study was conducted in accordance with the Helsinki Declaration (1964). Participants were informed of the study objectives, potential risks, and benefits. Written informed consent was obtained from all participants. Privacy, anonymity, and confidentiality were strictly maintained. Ethical clearance was obtained from the Institutional Review Board (IRB) of BSMMU prior to study initiation.
3. Result
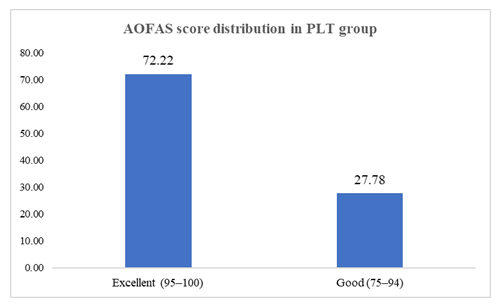
Among the 36 patients, the mean age was comparable between the QT group (29.50±6.16 years) and the PLT group (27.39±5.17 years) (p=0.239, 0.323). The 20–30-year age group was the most represented in both QT (66.67%) and PLT (61.11%). Males predominated in both groups, with a higher proportion in QT (94.44%) than PLT (72.22%) (p=0.074). Mean BMI values were similar (QT: 24.48±3.03 vs PLT: 24.32±1.77; p=0.963), with most patients in the normal range (Table 1). Table 2 showed that right-sided ACL injury was more frequent in QT (72.22%) than PLT (55.56%), while left-sided involvement was more common in PLT (44.44%), though not statistically significant (p=0.298). Road traffic accidents were the leading injury mechanism in QT (50.0%), whereas sports injuries predominated in PLT (55.56%). Most patients underwent surgery within 6 months of injury (QT: 72.22%, PLT: 83.33%), with no significant difference in mean delay to surgery (5.39±3.60 vs 4.78±3.19 months; p=0.743). The mean graft diameter was significantly greater in the QT group (8.53±0.56 mm) compared to PLT (8.08±0.43 mm) (p=0.027). In PLT, a notable proportion had smaller diameters of 7.5 mm (22.22%), whereas QT grafts more frequently measured 8 mm and 8.5 mm (Table 3). Table 4 presented that preoperatively, most patients in both QT and PLT groups had grade II laxity in the anterior drawer test (QT: 77.78%, PLT: 83.33%; p=0.674). Postoperatively, grade 0 stability was achieved in 88.89% of QT and 94.44% of PLT patients, with the remainder at grade I (QT: 11.11%). In the Lachman test, grade II laxity predominated preoperatively (QT: 72.22%, PLT: 77.78%), followed by grade III (QT: 27.78%, PLT: 22.22%), with none in grade 0 or I (p=0.700). Postoperatively, Lachman test (83.33% in QT vs. 88.89% in PLT) in grade 0, with no significant difference between the two (p=0.63). Importantly, no patient had grade II or III instability in either test after surgery. Preoperative Lysholm scores was 55.50±6.94 in the QT group and 57.56±5.47 in the PLT group (p=0.355), where postoperative Lysholm scores improved markedly in both groups (QT: 90.11±3.72 vs PLT: 91.61±3.17; p=0.171). The pre-operative IKDC scores was (QT: 55.50±6.94 vs PLT: 57.56±5.47; p=0.355) where the post-operative score was (QT: 89.22±4.33 vs PLT: 90.56±4.39; p=0.389). Mean postoperative knee ROM was slightly higher in PLT (136.11±3.23°) compared to QT (132.50±5.75°), though not statistically significant (p=0.068) (Table 5). Figure 1 demonstrated that in the PLT group, AOFAS score distribution revealed 72.22% excellent and 27.78% good outcomes. Final Lysholm-based outcomes showed most patients achieved excellent results (QT: 77.78%, PLT: 88.89%), followed by good outcomes, with only one fair result in QT. Complication rates were low and similar between groups; anterior knee pain occurred only in QT (16.67%), while paresthesia was noted only in PLT (5.56%). Superficial infection was observed in one patient from each group, and knee stiffness in one QT case (Table 6).
|
Variable |
QT Group (n=18) |
PLT Group (n=18) |
p-value |
||
|
n |
% |
n |
% |
||
|
Age (years) |
|||||
|
20–30 |
12 |
66.67 |
11 |
61.11 |
0.239* |
|
31–40 |
4 |
22.22 |
7 |
38.89 |
|
|
41–45 |
2 |
11.11 |
0 |
0 |
|
|
Mean± SD |
29.50 ±6.16 |
27.39 ±5.17 |
0.323** |
||
|
Gender |
|||||
|
Male |
17 |
94.44 |
13 |
72.22 |
0.074* |
|
Female |
1 |
5.56 |
5 |
27.78 |
|
|
BMI |
|||||
|
18.5- 24.9 (normal) |
12 |
66.67 |
13 |
72.22 |
0.341* |
|
25-29.9 (overweight) |
4 |
22.22 |
5 |
27.78 |
|
|
>30 (Obese) |
2 |
11.11 |
0 |
0 |
|
|
Mean ±SD |
24.48 ±3.03 |
24.32 ±1.77 |
0.963** |
||
|
Occupation |
|||||
|
Student |
8 |
44.44 |
7 |
38.89 |
0.693* |
|
Service Holder |
2 |
11.11 |
6 |
33.33 |
|
|
Athlete |
3 |
16.67 |
3 |
16.67 |
|
|
Business |
4 |
22.22 |
2 |
11.11 |
|
|
Homemaker |
1 |
5.56 |
0 |
0 |
|
Table 1:Demographic characteristics of the study population (N=36).
|
Variable |
QT Group (n=18) |
PLT Group (n=18) |
p-value |
||
|
n |
% |
n |
% |
||
|
Side involved |
|||||
|
Right |
13 |
72.22 |
10 |
55.56 |
0.298* |
|
Left |
5 |
27.78 |
8 |
44.44 |
|
|
Mechanism of injury |
|||||
|
Road traffic accident |
9 |
50 |
8 |
44.44 |
0.131* |
|
Sports |
6 |
33.33 |
10 |
55.56 |
|
|
Domestic accidents |
3 |
16.67 |
0 |
0 |
|
|
Duration from injury to surgery (months) |
|||||
|
< 6 month |
13 |
72.22 |
15 |
83.33 |
0.713* |
|
6-12 month |
3 |
16.67 |
2 |
11.11 |
|
|
>12 month |
2 |
11.11 |
1 |
5.56 |
|
|
Mean ±SD |
5.39 ±3.60 |
4.78 ±3.19 |
0.743** |
||
Table 2:Injury-related characteristics in ACL reconstruction patients of the study population.
|
Graft diameter (mm) |
QT Group (n=18) |
PLT Group (n=18) |
p-value |
||
|
n |
% |
n |
% |
||
|
7.5 |
0 |
0 |
4 |
22.22 |
0.112* |
|
8 |
7 |
38.89 |
8 |
44.44 |
|
|
8.5 |
6 |
33.33 |
5 |
27.78 |
|
|
9 |
2 |
11.11 |
1 |
5.56 |
|
|
9.5 |
3 |
16.67 |
0 |
0 |
|
|
Mean ± SD |
8.53 ± 0.56 |
8.08 ± 0.43 |
0.027** |
||
Table 3:Intraoperative graft characteristics of the study population.
|
Test |
Grade |
QT Group (n=18) |
PLT Group (n=18) |
p-value* |
||
|
n |
% |
n |
% |
|||
|
Anterior Drawer Test (ADT) |
||||||
|
Pre-operative |
0 |
0 |
0 |
0 |
0 |
0.674* |
|
I |
0 |
0 |
0 |
0 |
||
|
II |
14 |
77.78 |
15 |
83.33 |
||
|
III |
4 |
22.22 |
3 |
16.67 |
||
|
Post-operative |
0 |
16 |
88.89 |
17 |
94.44 |
0.546* |
|
I |
2 |
11.11 |
1 |
5.56 |
||
|
II |
0 |
0 |
0 |
0 |
||
|
III |
0 |
0 |
0 |
0 |
||
|
Lachman Test |
||||||
|
Pre-operative |
0 |
0 |
0 |
0 |
0 |
0.700* |
|
I |
0 |
0 |
0 |
0 |
||
|
II |
13 |
72.22 |
14 |
77.78 |
||
|
III |
5 |
27.78 |
4 |
22.22 |
||
|
Post-operative |
0 |
15 |
83.33 |
16 |
88.89 |
0.63 |
|
I |
3 |
16.67 |
2 |
11.11 |
||
|
II |
0 |
0 |
0 |
0 |
||
|
III |
0 |
0 |
0 |
0 |
||
Table 4:Preoperative and postoperative knee stability by Anterior Drawer and Lachman tests in QT and PLT of the study population.
|
Outcome measure |
QT Group (n=18) |
PLT Group (n=18) |
p-value |
|
Lysholm score |
|||
|
Pre-operative |
55.50 ± 6.94 |
57.56 ± 5.47 |
0.355* |
|
Post-operative |
90.11 ± 3.72 |
91.61 ± 3.17 |
0.171* |
|
IKDC score |
|||
|
Pre-operative |
55.00 ± 5.01 |
57.17 ± 4.34 |
0.214* |
|
Post-operative |
89.22 ± 4.33 |
90.56 ± 4.39 |
0.389* |
|
Knee ROM (°) |
|||
|
Post-operative |
132.50 ± 5.75 |
136.11 ± 3.23 |
0.068* |
Table 5:Functional outcome scores and postoperative range of motion in QT versus PLT groups of the study population.
Figure 1:Distribution of patients according to (AOFAS) Scores in the peroneus longus tendon (PLT) group of the study population.
|
Outcome |
QT Group (n=18) |
PLT Group (n=18) |
p-value |
||
|
n |
% |
n |
% |
||
|
Final outcome (Lysholm) |
|||||
|
Excellent |
14 |
78 |
16 |
89 |
0.513* |
|
Good |
3 |
17 |
2 |
11 |
|
|
Fair |
1 |
6 |
0 |
0 |
|
|
Complications |
|||||
|
Superficial infection |
1 |
6 |
1 |
6 |
0.257* |
|
Anterior knee pain |
3 |
17 |
0 |
0 |
|
|
Paresthesia |
0 |
0 |
1 |
6 |
|
|
Knee stiffness |
1 |
6 |
0 |
0 |
|
|
None |
13 |
72 |
16 |
89 |
|
Table 6:Final clinical outcomes and postoperative complication profiles following QT and PLT ACL reconstruction of the study population.
4. Discussion
Anterior cruciate ligament (ACL) injuries are prevalent among young, active individuals and pose significant risks of long-term functional impairment and joint degeneration. While patellar and hamstring tendon autografts have traditionally dominated ACL reconstruction, recent attention has focused on quadriceps tendon (QT) and peroneus longus tendon (PLT) as viable alternatives due to their distinct biomechanical properties and donor site profiles. Despite historical advancements in ACL management—from early immobilization to modern arthroscopic techniques—comparative clinical data on QT versus PLT remain limited. Evaluating their functional outcomes, knee stability, and recovery profiles is essential to guide patient-specific reconstruction strategies [9]. The mean age of the study population was 28.44±5.70 years (range 20–42), with no significant difference between the two groups. In the present study, the predominance of young patients is consistent with observations by Rhatomy et al. [10], Abdelkader et al. [11], and Hassan and Zein [12], who reported a higher susceptibility to ACL injuries in individuals aged 23–30, likely due to increased physical activity and sports participation. Male patients accounted for 83.3% of cases in both groups, reflecting findings by Galan et al. [13], Keyhani et al. [14], and Waly and Gawish [15]. Higher male involvement may be attributed to participation in high-intensity or contact sports, greater quadriceps mass, and delayed medical attention. The mean BMI was 24.48±3.03kg/m² in the QT group and 24.32±1.77kg/m² in the PLT group, in agreement with prior studies. Elevated BMI increases mechanical stress on the knee, raising injury risk. In both groups, the right knee was predominantly affected, accounting for 72.2% in the QT group and 55.6% in the PLT group. These findings align with previous studies reporting right knee ACL injuries in 55–65% of cases [12-17]. The higher incidence may relate to right-leg dominance, leading to greater functional stress and injury susceptibility. In the present study, the predominant mechanism of ACL injury was road traffic accidents (47.2%), followed by sports-related activities (44.4%) and domestic accidents (8.4%). These findings align with Khajotia et al. [17], and Kumar et al. [18], who similarly reported RTAs as the leading cause, with sports and falls contributing variably across different populations. In our study, 77.8% of patients underwent surgery within six months of injury. The mean interval to surgery was 5.39±3.60 months (QT) and 4.78±3.19 months (PLT), with no significant difference. In contrast, Waly and Gawish [15] and Vijay et al. [19], reported 30–45 days. The quadriceps tendon (QT) graft demonstrated a significantly larger diameter than the peroneus longus tendon (PLT) graft (8.53±0.56mm vs. 8.08±0.43mm), consistent with Waly and Gawish (2022) [15]. The QT graft’s predictable size enables harvesting in variable dimensions, accounting for its superior diameter compared to PLT grafts [20]. At final follow-up, 88.9% of QT group and 94.4% of PLT group patients demonstrated negative anterior drawer tests (ADT), whereas 11.1% and 5.6% showed Grade I translation, respectively. These outcomes align with Lee et al. [21], reporting 74.6% negative ADT in QT grafts, and Trung et al. [22], with 96.7% negative ADT in PLT grafts. Similarly, 83.3% of cases in the QT group and 88.9% of cases in the PLT group had negative Lachman tests at the final follow-up. Previous studies reported similar findings: Lee et al. [21] and Chen et al. [23] observed 70.2% and 88.2% negative tests with QT grafts, while Kumar et al. [18] and Trung et al. [22] reported 88–96% negative tests using PLT grafts in ACLR, At final follow-up, Lysholm scores improved significantly, reaching 90.11±3.72 (80–95) in the QT group and 91.61±3.17 (84–98) in the PLT group, with no significant intergroup difference. These findings are consistent with the study by Waly and Gawish [15], which reported mean Lysholm scores of 89.9±6.8 in the QT group and 90.1±3.8 in the PLT group [15]. Also, there was a significant improvement in the IKDC subjective score at final follow-up, with 89.22±4.33 (80–94) in the QT group and 90.56±4.39 (80–97) in the PLT group, though the difference was not significant. These findings align with those of Runer et al. [16], who reported a mean IKDC score of 93.9 for QT grafts, and Keyhani et al. [24], who observed a mean score of 92.5 for PLT grafts, Although the PLT group had a relatively better Knee ROM than the QT group, the difference was insignificant (136.11 ±3.23° vs 132.50 ±5.75°). This may reflect lower donor-site morbidity, as PLT grafts preserve hamstrings and quadriceps, whereas QT harvesting can impair the extensor mechanism and increase anterior knee pain. The AOFAS score was employed to assess donor site morbidity in patients who underwent PLT grafting, with a mean score of 95.11 ± 3.69 points at the final follow-up. These findings are consistent with previous studies by Rhatomy et al. [10] and Trung et al. [22], which reported final AOFAS scores ranging from 95 to 99 points, The most common complication in the QT group was anterior knee pain, affecting 16.7% (3 patients), with one case (5.6%) of superficial donor site infection, while in the PLT group, one patient (5.6%) had infection and paresthesia. In the present study, 77.8% of patients in the QT group achieved excellent outcomes, 16.6% good, and 5.6% fair, whereas 88.9% of the PLT group attained excellent outcomes and 11.1% good, with no poor outcomes in either group. These findings are consistent with previous reports: Chen et al. [23] observed 59% excellent and 35% good outcomes following ACLR with QT grafts, while Schulz et al. [25] reported 89.1% excellent to good outcomes. For PLT grafts, Hasan and Zein [12] documented 93% excellent, 4% good, and 3% fair outcomes.
5. Limitations of the Study
Despite careful conduct, this study had several limitations. It was a single-center investigation, limiting generalizability to broader populations. Additionally, the absence of blinding, combined with the researcher’s direct involvement in patient evaluation, surgery, and follow-up, may have introduced observer bias. The study lacked age- and sex-matched groups and did not employ randomization. Furthermore, the relatively short follow-up period restricted assessment of long-term functional outcomes and graft durability, warranting caution in extrapolating these findings.
6. Conclusion and Recommendations
ACL reconstruction with Quadriceps tendon and Peroneus longus tendon autograft both provided excellent functional improvement in patients at final follow-up. The functional outcome measures (Lysholm and IKDC scores) were relatively better in the Peroneus Longus tendon group than the Quadriceps group; however, the difference was insignificant. Regarding the peri-operative events, the graft diameter was significantly larger in the Quadriceps tendon group whereas donor site morbidity was lesser in the Peroneus longus tendon group.
It is recommended to conduct multi-center studies with larger sample size and long-term follow-up, employing blinding and randomized controlled trial designs, to further validate these findings and optimize graft selection in ACL reconstruction.
Funding: No funding sources
Conflict of interest: None declared
Ethical approval: The study was approved by the Institutional Ethics Committee.
References
- Khan HA, Ahad H, Sharma P, et al. Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma Monthly20(2015):e18635.
- Ertogrul R, Varol A, Oc Y, et al. Is Peroneus Longus Allograft Good Alternative for Anterior Cruciate Ligament Reconstruction: a Comparison Study. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 88(2021).
- Kim SJ, Kumar P, Oh KS. Anterior cruciate ligament reconstruction: autogenous quadriceps tendon–bone compared with bone–patellar tendon–bone grafts at 2-year follow-up. Arthroscopy: The Journal of Arthroscopic and Related Surgery25(2009):137-44.
- Hurley ET, Calvo-Gurry M, Withers D, et al. Quadriceps tendon autograft in anterior cruciate ligament reconstruction: a systematic review. Arthroscopy: The Journal of Arthroscopic and Related Surgery34(2018):1690-8.
- Johnston PT, McClelland JA, Feller JA, et al. Knee muscle strength after quadriceps tendon autograft anterior cruciate ligament reconstruction: systematic review and meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy29(2021):2918-33.
- Mustamsir E, Phatama KY. Tensile strength comparison between peroneus longus and hamstring tendons: a biomechanical study. International Journal of Surgery Open9 (2017):41-4.
- Kerimoglu S, Aynaci O, Saracoglu M, et al.Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthopaedica et Traumatologica Turcica42(2008):38-43.
- Agarwal A, Singh S, Singh A, et al. Comparison of functional outcomes of an anterior cruciate ligament (ACL) reconstruction using a peroneus longus graft as an alternative to the hamstring tendon graft. Cureus15(2023).
- D’Ambrosi R, Meena A, Arora ES, et al. Reconstruction of the anterior cruciate ligament: a historical view. Annals of Translational Medicine11(2023):364.
- Rhatomy S, Hartoko L, Setyawan R, et al. Single bundle ACL reconstruction with peroneus longus tendon graft: 2-years follow-up. Journal of Clinical Orthopaedics and Trauma11 (2020):S332-6.
- Abdelkader MA, Mostafa AG. Primary anterior cruciate ligament reconstruction using full-thickness peroneus longus tendon autograft. The Egyptian Orthopaedic Journal58(2023):186-91.
- Hassan AZ, Zein A. Functional knee and ankle outcomes of a peroneus longus tendon autograft for primary reconstruction of the anterior cruciate ligament. The Egyptian Orthopaedic Journal59(2024):125-31.
- Galan H, Escalante M, Della Vedova F, et al. All inside full thickness quadriceps tendon ACL reconstruction: Long term follow up results. Journal of Experimental Orthopaedics7(2020):13.
- Keyhani S, Qoreishi M, Mousavi M, et al. Peroneus longus tendon autograft versus hamstring tendon autograft in anterior cruciate ligament reconstruction: a comparative study with a mean follow-up of two years. Archives of Bone and Joint Surgery10(2022):695.
- Waly AH, Gawish HM. Comparative study between peroneus longus, semitendinosus tendon, and quadriceps tendon graft for anterior cruciate ligament reconstruction. The Egyptian Orthopaedic Journal57(2022):109-21.
- Runer A, Suter A, di Sarsina TR, et al. Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction show comparable clinical, functional, and patient-reported outcome measures, but lower donor-site morbidity compared with hamstring tendon autograft: A matched-pairs study with a mean follow-up of 6.5 years. Journal of ISAKOS8(2023):60-7.
- Khajotia BL, Chauhan S, Sethia R, et al. Functional outcome of arthroscopic reconstruction of anterior cruciate ligament tear using peroneus longus tendon autograft. Int J Res Orthop4(2018):898-903.
- Kumar VK, Narayanan SK, Vishal RB. A study on peroneus longus autograft for anterior cruciate ligament reconstruction. Int J Res Med Sci8(2020):183-8.
- Vijay C, Santosh MS, Avinash C, et al. Is Peroneus longus autograft a better alternative to the Hamstring autograft for anterior cruciate ligament reconstruction?–A randomised control study. Journal of Orthopaedics, Trauma and Rehabilitation29(2022):22104917221088335.
- Todor A, Caterev S, Nistor DV, et al. Free bone plug quadriceps tendon harvest and suspensory button attachment for anterior cruciate ligament reconstruction. Arthroscopy Techniques5(2016):e541-4.
- Lee S, Seong SC, Jo CH, et al.Anterior cruciate ligament reconstruction with use of autologous quadriceps tendon graft. JBJS89(2007):116-26.
- Trung DT, Le Manh S, Thanh LN, et al. Preliminary result of arthroscopic anterior cruciate ligament reconstruction using anterior half of peroneus longus tendon autograft. Open Access Macedonian Journal of Medical Sciences7(2019):4351.
- Chen CH, Chuang TY, Wang KC, et al. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: clinical outcome in 4–7 years. Knee Surgery, Sports Traumatology, Arthroscopy14(2006):1077-85.
- Keyhani S, Qoreishi M, Mousavi M, et al. Peroneus longus tendon autograft versus hamstring tendon autograft in anterior cruciate ligament reconstruction: a comparative study with a mean follow-up of two years. Archives of Bone and Joint Surgery10(2022):695.
- Schulz AP, Lange V, Gille J, et al. Anterior cruciate ligament reconstruction using bone plug-free quadriceps tendon autograft: intermediate-term clinical outcome after 24–36 months. Open Access Journal of Sports Medicine19 (2013):243-9.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 