Comparison of Outcome between Modified French Osteotomy and Three-Dimensional Osteotomy for the Management of Gunstock Deformity
Dr. Debashish Dey1*, Prof. Dr. Krishna Priya Das2, Dr. Md. Nazrul Islam1, Dr. Md. Golam Shaikh Ferdous1, Dr. Aminur Rasul1, Dr. Sabrina khan1
1DGHS, Deputed to Bangladesh Medical University, Dhaka, Bangladesh
2Department of Orthopaedic, Bangladesh Medical University, Dhaka, Bangladesh
*Corresponding Author: Dr. Debashish Dey, DGHS, Deputed to Bangladesh Medical University, Dhaka, Bangladesh.
Received: 27 August 2025; Accepted: 05 September 2025; Published: 12 September 2025
Article Information
Citation: Debashish Dey, Krishna Priya Das, Md. Nazrul Islam, Md. Golam Shaikh Ferdous, Aminur Rasul, Sabrina khan. Comparison of Outcome between Modified French Osteotomy and Three-Dimensional Osteotomy for the Management of Gunstock Deformity. Journal of Orthopedics and Sports Medicine. 7 (2025): 442-448.
View / Download Pdf Share at FacebookAbstract
Background: Gunstock deformity is a triplanar deformity around the elbow. Modified French osteotomy is profoundly used for the correction of deformity. However, as it doesn’t correct all three deformity components, hence, Three-Dimensional (3D) osteotomy was developed. Still, debate persists about the superiority of this technique.
Aim of the study: To compare the clinical outcomes between modified French osteotomy and three-dimensional osteotomy for management of gunstock deformity.
Methods: This prospective comparative study was conducted in the Department of Orthopaedics, BSMMU, Dhaka and New Life Hospital, Dhaka from October 2022 to September 2024 where 40 patients were allocated into two groups. Three-Dimensional osteotomy (Group A) and Modified French osteotomy (Group B). Assessments were done preoperatively and at one, three, six, and twelve months postoperatively. Clinical outcome was evaluated by assessing Carrying Angle, Range of Motion of Elbow, Mayo Elbow Performance Score (MEPS) and Radiological union. Data analysis was done by using ‘Statistical Package for Social Science’ version 26 and for all analyses p-value <0.05 was considered significant.
Result: The mean age of our study population was 11.28± 2.44 years with male predominance (65%). 55% of the cases had the involvement of left limb. 92.5% and 7.5% of the patients had a previous history of supracondylar and lateral condyle fracture of the humerus. The mean duration of initial injury to the surgery was 43.80 ±17.99 months. There was no significant difference between the groups in regard to demographic and clinical profile. At final follow up carrying angle, post-operative internal rotation correction, elbow flexion and MEPS score were significantly better in Group A than Group B (p<0.05). 75% had excellent and 25% had good outcomes in group A, but in group B, 40% had excellent results, 50% had good, and 10% had fair outcomes. Conclusion: Three-dimensional osteotomy corrects all the three forms of the deformities and automatically gives the stability, so it permits early mobilization and ensure better outcome than modified French osteotomy for the treatment of gunstock deformity.
Keywords
<p>3D osteotomy; Gunstock deformity; Cubitus varus deformity; French osteotomy</p>
Article Details
1. Introduction
The Gunstock deformity or Cubitus varus deformity involves a triplanar deformity around the elbow. It includes medial angulation in the coronal plane, internal rotation in the axial plane, and extension in the sagittal plane [1,2]. It is the most frequent long-term complication of a childhood supracondylar fracture of the humerus and is reported to occur in 3-59% of cases, with an average incidence of 30% when using different management methods [3-5]. The most common age range for these fractures is 5–7 years in children, and there is no significant variation in occurrence between genders [6]. Supracondylar fractures of the humerus can be divided into extension and flexion types, depending on the direction in which the distal fragment is displaced. Almost 98% of supracondylar humerus fractures are of the extension type and usually occur as a result of falling on an outstretched hand with the elbow fully extended [7]. The most significant causes of cubitus varus deformity are reported to be medial comminution, medial/varus tilt of the distal fragment, and suboptimal coronal reduction [2,4,7]. Whereas osteonecrosis and delayed trochlear growth, accompanied by overgrowth of the normal lateral side of the distal humeral epiphysis, are an uncommon reason for the development of progressive cubitus varus deformity following a supracondylar fracture [5]. Cubitus varus can lead to more musculoskeletal issues beyond just cosmetic concerns. These can include a higher likelihood of lateral condyle fractures, elbow posterolateral rotatory instability, ulnar neuropathy, snapping triceps, progressive ulnar varus, and adult elbow joint malalignment [5,8-10]. Three-dimensional CT scans confirm morphological changes in cubitus varus elbows, showing posterior trochlear overgrowth and increased internal rotation of the distal humerus posterior joint line. The proximal ulna adapts by laterally shifting the trochlear notch, extending the articular surface anteroposteriorly, and moving distally and medially, resulting in greater external rotation and flexion compared to the opposite side [8]. The altered anatomy around the elbow and the osteoarthritic changes associated with cubitus varus can directly impact the position and stability of the ulnar nerve, leading to nerve irritation and the development of ulnar neuropathy [11]. Similarly, snapping of the medial portion of the triceps may occur from the medial displacement of the triceps as well as the internal rotation of the distal humerus [12]. Although cosmetic concerns are a common reason for surgery, potential complications—such as posterolateral rotatory instability, secondary fracture, ulnar neuropathy, snapping triceps, and progressive varus of the ulna—have shifted practice toward proactive surgical correction of cubitus varus. Various corrective techniques exist. In French osteotomy, the angulation correction axis lies proximal to the varus deformity’s center of rotation, causing lateral translation and prominence of the lateral condyle [13]. Three-dimensional osteotomy for correcting cubitus varus deformity allows for the correction of medial and posterior tilt as well as rotation of the distal fragment [7]. Therefore, it is optimal for the patient to undergo osteotomy to correct all three components of the cubitus varus deformity complex simultaneously and restore the anatomical alignment of the elbow joint [14]. The study aimed to compare the clinical, functional, and radiological outcomes between modified French osteotomy and three-dimensional osteotomy in the management of gunstock (cubitus varus) deformity.
2. Methodology and Materials
This prospective comparative study was conducted in the Department of Orthopaedic Surgery at Bangabandhu Sheikh Mujib Medical University (BSMMU), Shahbagh, Dhaka and New Life Hospital, Dhaka over a period from October 2022 to September 2024. The study population comprised patients presenting with gunstock deformity (cubitus varus deformity) who attended the Outpatient Department of Orthopaedic Surgery within the defined study period. Using a simple random sampling technique, a total of 40 patients were enrolled. They were then grouped purposively based on their serial number of admissions, following the odd-even technique, to form two comparison groups.
- • Group A (Three-Dimensional Osteotomy Group): Patients with odd admission numbers.
- • Group B (Modified French Osteotomy Group): Patients with even admission numbers.
2.1 Inclusion criteria:
- • Age up to 20 years
- • Patients with diagnosed case of Gunstock/ Cubitus varus deformity
- • Duration of fracture >1 year
2.2 Exclusion criteria:
- • Patients with associated complications like nerve palsy, Volkmann’s ischemic contracture, and myositis ossificans
- • Marked osteoarthritic change of the elbow joint on radiographs
- • Patients not fit for surgical procedure
2.3 Ethical implications
In this study, keeping compliance with Helsinki Declaration for Medical Research Involving Human Subjects 1964, the nature and purpose of the study were informed in detail to all participants. Voluntary participation was encouraged. There was possibility of physical, psychological risk to the subjects. Informed and understood written consent was taken from every patient before enrollment. Privacy, anonymity and confidentiality of data information identifying any patient were maintained strictly. Each patient had every right to participate or refuse or even withdraw from the study at any point of time. With the permission of academic committee of Department of Orthopaedic surgery, BSMMU, initial work up for thesis was started, then approval of research protocol and ethical clearance by the Institutional Review Board (IRB) of BSMMU, Dhaka was taken. Data taken from the participants was regarded as confidential and kept locked under investigator for purposeful use only. This protocol primarily selected by the academic committee of the department of Orthopaedic Surgery.
2.4 Data collection
After obtaining informed consent, a detailed history and physical examination of each patient were carried out. Plain radiographs of the affected elbow joint (anteroposterior and lateral views) were obtained, and all necessary preoperative investigations were completed. Data were collected using a structured case record form which was used to record information in the preoperative, peroperative, and postoperative phases. The case record form was filled by the interviewers through direct interviews and clinical assessments. Patients underwent either three-dimensional osteotomy or modified French osteotomy, according to their assigned group. Postoperative follow-up was scheduled at one, three, six, and twelve months, during which patients were evaluated both clinically and radiologically, as well as by MEPS scoring. Clinical outcomes were evaluated by measuring the carrying angle and the range of motion of the elbow, while functional outcomes were assessed using the Mayo Elbow Performance Score (MEPS).
2.5 Statistical analysis
The analyses of different variables were done according to standard statistical analysis. Qualitative data were expressed as frequency and percentage and analyzed by chi-square test. Quantitative data were expressed as mean and standard deviation and analyzed by student t-test (parametric) and Mann- Whitney U test (non-parametric). Data were processed and analyzed using software ‘Statistical Package for Social Science’ (SPSS) version 26, IBM®, Armonk, USA. For all analyses, statistical significance was set at p <0.05 and confidence interval set at 95% level.
3. Result
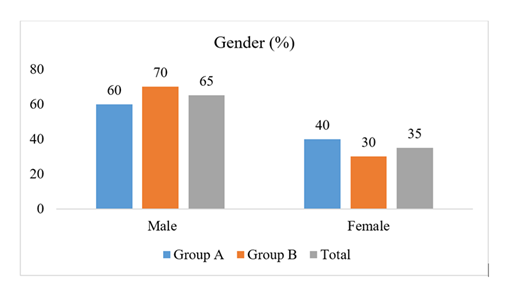
Table 1 showed that the majority in both groups were aged 10–15 years (Group A: 60.0%, Group B: 65.0%), followed by <9 years (25.0% in each group). Mean age was comparable (11.55±2.54 years in Group A vs. 11.00±2.36 years in Group B, p=0.584), with no significant intergroup difference (p=0.887). Figure 1 illustrated the gender distribution. Males predominated in both groups (Group A: 60%, Group B: 70%), while females accounted for 40% and 30%, respectively. Right-hand dominance was most frequent (95.0% in Group A vs. 85.0% in Group B, p=0.404). Limb involvement was almost equally distributed between right and left sides. The most common cause was supracondylar fracture (92.5% overall). Previous treatments included plaster by doctor (57.5%), bone setters (20.0%), and percutaneous pinning (17.5%). Mean injury duration was similar (43.80±17.99 months overall, p=0.284) (Table 2). Group A had significantly earlier union (10.25±1.29 weeks) compared to Group B (12.25±1.71 weeks, p=0.001). The majority in Group A achieved union within 8–10 weeks (65.0%), while in Group B most required 11–12 weeks (50.0%) or longer, with a significant difference in distribution (p=0.024) (Table 3). Table 4 compared radiological angles. Preoperative carrying and internal rotation angles were similar. Postoperatively, Group A had a higher mean carrying angle (11.10±2.13°) than Group B (9.40±2.62°, p = 0.035) and significantly less internal rotation (2.25±1.65° vs. 5.60±1.76°, p=0.001). Postoperatively, Group A achieved significantly greater flexion (132.90±2.32° vs. 130.20±3.25°, p=0.008), while extension improvement was similar between groups (p = 0.432) (Table 5). Preoperative MEPS scores were similar, but postoperative scores were significantly higher in Group A (91.50±5.64) than Group B (86.00±7.18, p=0.015). Excellent final outcomes (>90) were achieved in 75.0% of Group A versus 40.0% of Group B (p=0.045) (Table 6). Table 7 listed postoperative complications. Group A had fewer complications overall, with 90.0% experiencing none compared to 60.0% in Group B. Complications in Group B included pin tract infection (10.0%), nerve injury (10.0%), and under-correction (15.0%). No statistically significant difference was observed (p=0.185).
|
Parameter |
Group A (n=20) |
Group B (n=20) |
Total (n=40) |
P-value |
|
n (%) |
n (%) |
n (%) |
||
|
Age (years) |
||||
|
<9 |
5 (25.0) |
5 (25.0) |
10 (25.0) |
0.887 |
|
42278 |
12 (60.0) |
13 (65.0) |
25 (62.5) |
|
|
>15 |
3 (15.0) |
2 (10.0) |
5 (12.5) |
|
|
Mean± SD |
11.55± 2.54 |
11.00± 2.36 |
11.28± 2.44 |
0.584 |
Table 1: Distribution of patients according to age (N=40).
|
Parameter |
Group A (n=20) |
Group B (n=20) |
Total (n=40) |
P-value |
|
n (%) |
n (%) |
n (%) |
||
|
Hand Dominancy |
||||
|
Right |
19 (95.0) |
17 (85.0) |
36 (90) |
0.404 |
|
Left |
1 (5.0) |
3 (15.0) |
4 (10.0) |
|
|
Involved limb |
||||
|
Right |
10 (50.0) |
8 (40.0) |
18 (45.0) |
0.525 |
|
Left |
10 (50.0) |
12 (60.0) |
22 (55.0) |
|
|
Cause |
||||
|
Supracondylar Fracture |
19 (95.0) |
18 (90.0) |
37 (92.5) |
0.548 |
|
Lateral Condyle Fracture |
1 (5.0) |
2 (10.0) |
3 (7.5) |
|
|
Previous Treatment |
||||
|
Bone setters |
6 (30.0) |
4 (20.0) |
10 (20.0) |
0.746 |
|
Plaster by Doctor |
11 (55.0) |
12 (60.0) |
23 (57.5) |
|
|
Percutaneous pinning |
3 (15.0) |
4 (20.0) |
7 (17.5) |
|
|
Duration of Injury |
||||
|
Duration (months) |
46.10 ± 18.57 |
41.50± 17.56 |
43.80 ±17.99 |
0.284 |
|
≤ 35 month |
8 (40.0) |
10 (50.0) |
18 (45.0) |
0.525 |
|
> 35 month |
12 (60.0) |
10 (50.0) |
22 (55.0) |
|
Table 2: Clinical characteristics of the study population (N=40).
|
Bony Union Time (weeks) |
Group A (n=20) |
Group B (n=20) |
Total (n=40) |
P-value |
|
n (%) |
n (%) |
n (%) |
||
|
45938 |
13 (65.0) |
4 (20.0) |
17 (42.5) |
0.024 |
|
46002 |
6 (30.0) |
10 (50.0) |
16 (40.0) |
|
|
13-14 |
1 (5.0) |
5 (25.0) |
6 (15.0) |
|
|
>14 |
0 (0.0) |
1 (5.0) |
1 (2.5) |
|
|
Mean ± SD (Min-Max) |
10.25 ± 1.29 (8–13) |
12.25± 1.71 (9–16) |
11.25± 1.81 (8–16) |
0.001 |
Table 3: Bony Union Time of the study patients (N=40).
|
Parameter |
Group A, Mean ± SD (Min-Max) |
Group B, Mean ± SD (Min-Max) |
P-value |
|
Carrying angle (°) |
|||
|
Preoperative |
-21.15 ± 3.33 (-27 to -14) |
-19.75 ± 3.45 (-26 to -13) |
0.644 |
|
Postoperative |
11.10 ± 2.13 (5–14) |
9.40 ± 2.62 (3–12) |
0.035 |
|
Internal rotation (°) |
|||
|
Preoperative |
27.15 ± 4.32 (20–36) |
27.60 ± 3.50 (22–34) |
0.745 |
|
Postoperative |
2.25 ± 1.65 (0–5) |
5.60 ± 1.76 (2–9) |
0.001 |
Table 4: Radiological Angles – Carrying Angle and Internal Rotation (N=40).
|
Parameter |
Group A, Mean ± SD (Min-Max) |
Group B, Mean ± SD (Min-Max) |
P-value |
|
Flexion (°) |
|||
|
Preoperative |
125.10 ± 5.39 (116–136) |
126.85 ± 5.14 (117–135) |
0.207 |
|
Postoperative |
132.90 ± 2.32 (129–138) |
130.20 ± 3.25 (124–136) |
0.008 |
|
Extension (°) |
|||
|
Preoperative |
15.50 ± 4.67 (5–22) |
14.55 ± 4.87 (5–22) |
0.384 |
|
Postoperative |
3.20 ± 1.32 (0–6) |
3.45 ± 1.43 (0–6) |
0.432 |
Table 5: Elbow Range of Motion – Flexion and Extension (N=40).
|
Variables |
Group A, Mean ± SD (Min-Max) |
Group B, Mean ± SD (Min-Max) |
P-value |
|
Functional outcome (MEPS Score) |
|||
|
Preoperative |
77.50 ± 7.16 (65–85) |
78.25 ± 6.34 (70–85) |
0.746 |
|
Postoperative |
91.50 ± 5.64 (80–100) |
86.00 ± 7.18 (70–95) |
0.015 |
|
P-value (within group) |
0.001 |
0.001 |
|
|
Final Outcome |
|||
|
Excellent (>90) |
15 (75.0) |
8 (40.0) |
0.045 |
|
Good (75-89) |
5 (25.0) |
10 (50.0) |
|
|
Fair (60-74) |
0 (0.0) |
2 (10.0) |
|
|
Poor (<60) |
0 (0.0) |
0 (0.0) |
|
Table 6: Distribution of patients according to functional and final outcome (N=40).
|
Complication |
Group A (n=20) |
Group B (n=20) |
P-value |
|
n (%) |
n (%) |
||
|
Superficial wound infection |
1(5.0) |
1 (5.0) |
0.185 |
|
Pin tract infection |
0 (0.0) |
2 (10.0) |
|
|
Nerve injury |
0 (0.0) |
2 (10.0 ) |
|
|
Under-correction |
1 (5.0) |
3 (15.0) |
|
|
None |
18 (90.0) |
12 (60.0) |
Table 7: Postoperative complications among participants (N=40).
4. Discussion
The mean age of our study population was 11.28± 2.44 years with range of 8- 17 years, and there was no significant difference in population distribution between the two groups. Similar findings have been reported by Takagi et al. [15] and Madhuchandra et al. [16], where the authors have reported the average age of 11.1 years and 9.2 years, respectively. In this study, 65% of patients were male and 35% female, with no significant difference between groups. Similar findings have been reported in literature, with male prevalence ranging from 55.55% to 86.67% [5,17-20]. The higher male incidence is likely due to greater outdoor activity and higher risk of falls and elbow fractures. 55% of the study population had left limb involvement and there was no significant difference between the groups. Our results were comparable to the study done by Madhuchandra et al. [16] and Kumar et al. [20] where the studies have shown involvement of left limb in 52.8% and 57.14% respectively. The cause of cubitus varus deformity has been linked to post traumatic causes around the elbow usually a supracondylar fracture of humerus. The prevalence of developing cubitus varus deformity following supracondylar fracture of humerus ranges from 9- 58% in other study [3]. In our study 92.5% of the patients had a previous history of supracondylar fracture of the humerus, whereas 7.5% had a history of lateral condyle fracture. However, there was no significant difference between the groups (p= 0.548). These results were comparable to the study done by Kumar et al. [20]. We found that 20% of the patients had a history of treatment for the previous fracture by traditional bone settlers, whereas 57.5% were managed with plaster and 17.5% were managed with percutaneous pinning. However, the groups had no significant difference (p= 0.746). Das et al. [5] reported that 10% of patients were treated by traditional bone setters, 75% with plaster, and 15% surgically. Cubitus varus often results from medial comminution or inadequate coronal plane correction of supracondylar fractures. In developing countries, limited surgical access, lack of fluoroscopy, and reliance on traditional healers contribute to its higher prevalence [21]. The mean duration from initial injury to the index surgery was 43.80 ±17.99 months with a range of 28–96 months. There was no significant difference between the groups. The results were comparable to Kumar et al. [20], who reported a mean injury-to-surgery interval of 3.60 ± 2.01 years. In this study, 55% of patients presented after 35 months of injury, similar to Das et al. [5] (45%). The delayed presentation may be due to limited medical facilities in rural areas and the gradual progression of the deformity, with guardians often seeking care only when cosmetic concerns become pronounced. The mean duration for bony union at osteotomy site was 10.25 ± 1.29 weeks in 3D osteotomy, whereas it was 12.25± 1.71 weeks in modified French osteotomy. Bony union was observed significantly earlier following 3D osteotomy than the modified French osteotomy (p=0.024, 0.001). The results were similar to that of Ghieth et al. [22] and Li et al. [23]. Postoperatively the carrying angle improved significantly (from varus to valgus) to 11.10°± 2.13° (5-14°) following 3D osteotomy and 9.40°± 2.62° (3-12°) following modified French osteotomy. Significant improvement in carrying angle was observed following 3D osteotomy than modified French osteotomy (p=0.035). Das et al. [5] and Li et al. [23] showed postoperative carrying angle of 9.50°±1.77° and 10.6° ±4.5°, respectively following 3D osteotomy [5,23]. Similarly, Madhuchandra et al. [16], Orbach et al. [18], and Ahmad [24] showed similar carrying angle following modified French Osteotomy. The mean preoperative internal rotation was 27.15° ± 4.32° (20-36°) in the 3D group, whereas it was 27.60°± 3.50° (22-34°) in the French group. Postoperatively, the Internal rotation deformity was corrected to 2.25°± 1.65° (0-5°) in the 3D group and 5.60°± 1.76° (2-9°) in the French group. There was a significant improvement in the correction of internal rotation in 3D group than French group (p=0.001). These results were similar to that of Das et al. [5]. The greater internal rotation correction with 3D osteotomy is because French osteotomy was originally designed for single-plane (coronal) correction. While its modification allows limited rotational correction, 3D osteotomy addresses all three planes of cubitus varus deformity, overcoming the limitations of the French technique. The mean preoperative flexion at elbow joint was 125.10° ± 5.39° (116-136°) in the 3D group, whereas it was 126.85°± 5.14° (117 to 135°) in the French group (p=0.207). Postoperatively, the flexion improved to 132.90°± 2.32° (129-138°) in the 3D group and 130.20°± 3.25° (124-136°) in the French group. There was a significant improvement in flexion in 3D group than French group (p=0.008). Das et al. [5] reported similar findings in term of 3D osteotomy. Ahmad [24] and North et al. [13] reported similar findings in term of modified French osteotomy. The significant improvement in flexion might be due to the precision of correction of the deformity following 3D osteotomy which improves the elbow kinematics that could recover the elbow range of motion [25]. The mean preoperative extension at elbow joint was 15.50°± 4.67° (5- 22°) in the 3D group, whereas it was 14.55°± 4.87°, (5- 22°) in the French group (p=0.384). Postoperatively, the extension was corrected to 3.20°± 1.32° (0-6°) in the 3D group and 3.45°± 1.43° (0-6°) in the French group. There was a no significant difference between the groups (p=0.432). The results were similar to that of Omori et al. [17] and North et al. [13]. The mean preoperative MEPS score was 77.50± 7.16 (65- 85) in the 3D group, whereas it was 78.25± 6.34 (70- 85) in the French group. Postoperatively, the MEPS score improved significantly to 91.50± 5.64 (80-100) in the 3D group and 86.00± 7.18 (70-95) in the French group (p=0.001). The MEPS score was significantly better following 3D osteotomy than modified French osteotomy (p=0.015). Similar to Li et al. [23], the superior results of 3D osteotomy may be attributed to its more effective correction of triplanar deformities, leading to improved elbow biomechanics and function. According to our study, 3D osteotomy resulted in 75% excellent and 25% good outcomes, while modified French osteotomy showed 40% excellent, 50% good, and 10% fair outcomes, with a significant difference between groups (p=0.045). In contrast, Li et al. [23] reported higher success, with 95% excellent and 5% good outcomes for 3D osteotomy and 100% excellent outcomes for modified French osteotomy, likely due to the use of patient-specific 3D-printed template guides, which improved accuracy, early union, and rehabilitation. In this study, both groups had 5% superficial wound infection, while the modified French group had 10% pin tract infection and 10% nerve injury. Undercorrection occurred in 5% of 3D osteotomy cases and 15% of modified French cases, with no significant group difference (p=0.185). Comparable findings were reported by Das et al. [5], Madhuchandra et al. [16], and Kumar et al. [20] with varying rates of nerve injury, infection, and undercorrection.
5. Limitations of the Study
Every research has its confines. Though optimal attention was given by the investigator, there were some restrains which we couldn’t address.
- • This study was conducted at a single hospital setup, so the study population may not represent the whole community which is needed for study.
- • There is a chance of selection bias due to purposive sampling.
- • Long term outcome couldn’t be assessed due to short follow up duration.
6. Conclusion
Correction of Gunstock deformity by three-dimensional osteotomy ensures correction of all the three form of deformity and gives stability which ensures early mobilization and better outcome in comparison to modified French osteotomy. Also, three-dimensional osteotomy provided early radiological union in comparison to modified French osteotomy.
7. Recommendation
- • Multicenter study to represent the appropriate study population
- • Larger sample size and randomization for precise analysis.
- • Long period of follow-up, to look at long term outcomes and quality of life.
Funding:
No funding sources
Conflict of interest:
None declared
Ethical approval:
The study was approved by the Institutional Ethics Committee.
References
- Yamamoto I, Ishii S, Usui M, et al. Cubitus varus deformity following supracondylar fracture of the humerus: a method for measuring rotational deformity. Clin Orthop Relat Res 201 (1985): 179-185.
- Solfelt DA, Hill BW, Anderson CP, et al. Supracondylar osteotomy for the treatment of cubitus varus in children: a systematic review. Bone Joint J 96 (2014): 691-700.
- Jain AK, Dhammi IK, Arora A, et al. Cubitus varus: problem and solution. Arch Orthop Trauma Surg 120 (2000): 420-425.
- Dudhekar U. Prospective study of cubitus varus deformity, its etiopathology, clinical study and treatment. Int J Res Med Sci 5 (2017): 201.
- Das KP, Datta NK, Khan MZ, et al. Outcome of three-dimensional osteotomy for cubitus varus deformity. Int J Res Orthop 7 (2021): 444.
- Russo SA, Abzug JM. Supracondylar humerus fractures. In: Pediatric Elbow Fractures: A Clinical Guide to Management. Cham: Springer; (2017): 37-64.
- Sawyer JR, Spence DD. Fractures and dislocations in children. In: Canale ST, Frederick MA, James HB, et al., editors. Campbell’s Operative Orthopaedics. 14th ed. Philadelphia: Elsevier; (2021).
- Ho CA. Cubitus varus—it's more than just a crooked arm! J Pediatr Orthop 37 (2017): S37-S41.
- Abzug JM, Herman MJ, Kozin S. Pediatric elbow fractures. New York: Springer; (2018).
- Skaggs DL, Flynn JM. Supracondylar fractures of the distal humerus. In: Waters PM, Skaggs DL, Flynn JM, editors. Rockwood and Wilkins’ Fractures in Children. 9th ed. Philadelphia: Wolters Kluwer; (2020): 754-844.
- Fujioka H, Nakabayashi Y, Hirata S, et al. Analysis of tardy ulnar nerve palsy associated with cubitus varus deformity after a supracondylar fracture of the humerus: a report of four cases. J Orthop Trauma 9 (1995): 435-440.
- Spinner RJ, O’Driscoll SW, Davids JR, et al. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg 24 (1999): 718-726.
- North D, Held M, Dix-Peek S, et al. French osteotomy for cubitus varus in children: a long-term study over 27 years. J Pediatr Orthop 36 (2016): 19-24.
- Usui M, Ishii S, Miyano S, et al. Three-dimensional corrective osteotomy for treatment of cubitus varus after supracondylar fracture of the humerus in children. J Shoulder Elbow Surg 4 (1995): 17-22.
- Takagi T, Takayama S, Nakamura T, et al. Supracondylar osteotomy of the humerus to correct cubitus varus: do both internal rotation and extension deformities need to be corrected? J Bone Joint Surg Am 92 (2010): 1619-1626.
- Madhuchandra P, Pawankumar KM. Modified French osteotomy for cubitus varus correction—our experience. J Orthop Traumatol Rehabil 16 (2024): 79-84.
- Omori S, Murase T, Oka K, et al. Postoperative accuracy analysis of three-dimensional corrective osteotomy for cubitus varus deformity with a custom-made surgical guide based on computer simulation. J Shoulder Elbow Surg 24 (2015): 242-249.
- Orbach H, Rozen N, Rubin G, et al. Outcomes of French’s corrective osteotomy of the humerus for cubitus varus deformity in children. Isr Med Assoc J 20 (2018): 442-445.
- Kasirajan S, Govindasamy R, Lokayah SK. Functional outcome of modified French osteotomy fixed with recon-locking compression plate in older children. J Clin Orthop Trauma 16 (2021): 202-207.
- Kumar S, Jashanpreet J, Singh R. A clinical study of outcomes of supracondylar osteotomy in correcting cubitus varus deformities. Int J Health Sci (2024): 9972-9987.
- Abzug JM, Herman MJ, Kozin S. Pediatric elbow fractures. New York: Springer; (2018).
- Ghieth MAEA, Sebaai MA, Kotb MI. Three-dimensional corrective osteotomy of cubitus varus by modified step cut osteotomy of supra condylar humerus. Am Res J Orthop Traumatol 5 (2020): 1-8.
- Li J, Wang J, Rai S, et al. 3D-printed model and osteotomy template technique compared with conventional closing-wedge osteotomy in cubitus varus deformity. Sci Rep 12 (2022): 6762.
- Ahmad I, Idrees M. Modified French osteotomy for cubitus varus deformity. Pak J Surg 23 (2007): 1-5.
- Oka K, Miyamura S, Shiode R, et al. Three-dimensional corrective osteotomy for cubitus varus deformity using patient-matched instruments. JSES Int 8 (2024): 646-653.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 