Diaphragm Ultrasound: A Valuable Predictor of the Outcome of Extubation. An Observational Pilot Study in Covid-19 Related ARDS
Veronica Gagliardi1*, Angelo Butturini2, Gioconda Ferraro2, Giuseppe Gagliardi1,2
1University of Padua, Italy
2Department of Anesthesia and Intensive Care, Ospedale Santa Maria della Misericordia, AULSS 5 Polesana, Rovigo, Italy
*Corresponding author: Veronica Gagliardi, University of Padua, Italy.
Received: 12 August 2022; Accepted: 22 August 2022; Published: 09 September 2022
Article Information
Citation:
Veronica Gagliardi, Angelo Butturini, Gioconda Ferraro, Giuseppe Gagliardi. Diaphragm Ultrasound: A Valuable Predictor of the Outcome of Extubation. An Observational Pilot Study in Covid-19 Related ARDS. Archives of Clinical and Biomedical Research 6 (2022): 771-780.
View / Download Pdf Share at FacebookAbstract
Introduction: Because both early and delayed weaning are associated with increased mortality, longer stay in the ICU and higher economic costs, performing extubation once the patient can cope with the respiratory load is completely recommended. Ultrasound Sonography (US) is an available bedside tool that allows a rapid assessment and visualization of the different structures involved in spontaneous breath. M-mode ultrasonography can be useful for the assessment of diaphragm kinetics, providing valuable information about diaphragm disfunction.
Aim of the Study: The aim of this study is to find a correlation between the value of the acceleration of the diaphragm detected with the US M-mode and the outcome of the weaning. Materials and Methods: We have enrolled 19 patients admitted in our ICU. Each patient underwent the trial with the ultrasound M-mode to assess the acceleration of the diaphragm during the contraction. We have analyzed the results relating them to the outcome of the weaning.
Results: While 11 of our patients have had a successful weaning, 8 have failed it, and we can see that the outcome is associated to the values of acceleration.
Discussion: Our study has demonstrated that an assessment of the diaphragm function using US could represent a usable and effective technique as the acceleration is related to the force generated by the diaphragm contraction.
Conclusions: In conclusion, the acceleration could be a useful parameter to consider when it comes to the prediction of the outcome of the weaning process.
Keywords
<p>Diaphragm; ICU; Rapid Shallow Breathing Index; Ultrasound Sonography</p>
Article Details
1. Introduction
Even though mechanical ventilation is an established widespread supportive treatment for respiratory failure, it is not risk-free: when prolonged, it increases the risk of pneumonia, barotrauma, tracheal injuries, and musculoskeletal deconditioning [1]. Conversely, premature removal of mechanical ventilation entails a high risk of weaning failure, and prompting reintubation exposes the patient to unnecessary hemodynamic and respiratory stress [2,3]. Both early and delayed weaning are associated with increased mortality, longer stay in the ICU and higher economic costs: performing extubation once the patient is able to cope with the respiratory load is completely recommended [1,4]. Prolonged mechanical ventilation can lead to ventilator-induced diaphragmatic dysfunction, in a context where the diaphragm is also vulnerable to damage from hypotension, hypoxia and sepsis [4]. Disuse atrophy of the diaphragm plays a pivotal role in weaning failure and from the examination of diaphragm biopsies we can infer that the changes of the structure occur early after intubation [5]. To sum up, diaphragm dysfunction is defined as the inability of the diaphragm to generate reasonable levels of maximal force and it is an under-detected pathological condition in critically ill patients which could impair weaning from mechanical ventilation. Weaning failure, defined as the requirement of invasive or noninvasive mechanical ventilation within 48 hours after extubation, is extremely common: about 20% of mechanically ventilated patients require reintubation [6]. Although the implementation of spontaneous breathing trials is recommended by current guidelines, this practice is ineffective alone in predicting weaning failure and consequent reintubation [2]. The identification of the suitable conditions for weaning should be evaluated daily, assessing the improvement of the respiratory failure, of the ability to protect the airway and to start an inspiratory effort, of the fluid balance and the acid-base equilibrium, and of the level of consciousness [3]. In the last few years multiple indices and parameters have been proposed as predictors of weaning outcome, but none of them has shown more than a modest prognostic accuracy [2]: performing the weaning in the optimal moment is still a current challenge [3]. Considering the expiratory physiology research, the evaluation of esophageal pressure using esophageal manometry helps to extimate the trans-diaphragmatic pressure, the gold standard to evaluate the diaphragm force: when this is less than 11 cmH2O diaphragm dysfunction occurs [8]. Many other weaning parameters have been used to predict weaning failure, including rapid shallow breathing index (RSBI), which is the ratio of respiratory rate to tidal volume: RSBI <105 correlates with weaning success, whereas a score >105 correlates with weaning failure [1], minute ventilation (VE), maximum inspiratory pressure (PImax) [4], and the pressure developed in the occluded airway 100 ms after the onset of an inspiratory effort: P0.1 [7]. In this context, Ultrasound Sonography (US) is an available bedside tool that allows rapid assessment and visualization of the thoracic and abdominal structures. More recently, ultrasonography has been used to assess the diaphragm kinetics. The two-dimensional mode is initially used to obtain the best approach and select the exploration line; the M-mode is then used to display the motion of the anatomical structures along the selected line [9]. By providing a direct visualization of the diaphragm with both morphological and functional information in real time, [10] the use of ultrasonographic assessment of diaphragmatic dysfunction could well represent a valuable predictor of weaning failure [1]. To study the diaphragm function, the patient is placed in supine position with the trunk elevated of 10–15°, the function of each hemidiaphragm can be explored with a low frequency (3.5–5 MHz) ultrasound transducer (convex or phased array probe) placed along the midclavicular line or below the costal margin in the longitudinal plane. Technical difficulties in visualizing the left diaphragm have been described, leading most clinicians to perform right diaphragm measurements [11,12]. The M-mode is then used along the selected line to show movements and measure the excursion or displacement of a point of the hemidiaphragm during the respiratory phases. The ultrasound on M-mode trace appears as a wave shape: from the curve obtained the diaphragmatic excursion, the inspiratory and expiratory times. In addition, the M-mode can distinguish diaphragmatic weakness from paralysis: the first shows a reduced diaphragmatic caudal movement, whereas the second is characterized by a paradoxical motion. As far as the speed of diaphragmatic contraction is concerned, a study performed a diaphragmatic sonography with the M-mode technique, calculating the diaphragm contraction speed as the slope (Scdi) of the curve provided by the diaphragm contraction during the inspiratory phase of the spontaneous breathing trials. The contraction speed represented a bedside, standardized and reproducible tool to predict the outcome of weaning [13]. Diaphragmatic ultrasound may identify patients at risk of weaning failure, it is mandatory to standardize the diagnostic criteria of diaphragm dysfunction and the diagnostic performance to predict weaning outcome [3], also because the technique is operator dependent and needs dedicated training. While studying the diaphragm dynamics with the US, we have detected a new parameter, the acceleration of the diaphragm, obtainable dividing the time of contraction to the speed of it, studied with the M-mode of the US.
2. Aim of the Study
Firstly, we want to study the correlation between the value of the acceleration of the diaphragm detected with the US M-mode and the outcome of the weaning. Secondly, we want to assess if this value could be predictive of success or failure in weaning.
3. Materials and Methods
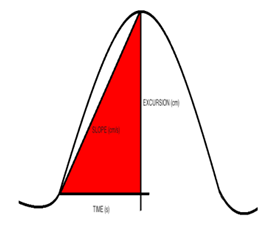
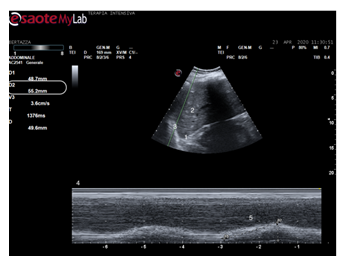
We have enrolled 19 patients admitted in the ICU between March 2020 and April 2021. We have included only patients admitted in the ICU in the above-mentioned period in which neither the available recommended methods (SBT and RSBI, VE, PImax and P0.1) nor clinical parameters were reliable to predict the outcome of extubation. Their mean age was 66 years old; 3 patients were female, with a mean age of 66 years old, and 16 patients were male, with a mean age of 67 years old (Table 1). Each patient underwent the trial with the ultrasound M-mode to assess the acceleration of the diaphragm. The experimental protocol consists of an ultrasonographic analysis of the diaphragmatic activity, using the MyLab Esaote and the probe Convex 5-2 MHz. The probe has been located on the right middle axillary line, in plane along with the sagittal plan. An inclination of 15-20° has then been applied, to direct the ultrasound beam perpendicularly to the rear third of the homolateral hemidiaphragm. Because of the interindividual variability of the patients’ built, the anatomic landmark for each has been identified either in the seventh, or in the eighth, or in the nineth intercostal space, choosing the one which allowed the best acoustic window to detect the diaphragmatic dome and its excursion both in M-mode and in B-mode. Focusing on the M-mode, the following parameters has been measured (Figure 1):
- Diaphragmatic excursion (displacement, cm)
- Time of inspiration (Tinsp, s)
- Velocity of diaphragm contraction (slope, cm/s).
The outcome of the further extubation has been detected (Table 2). We define a successful weaning as the absence of ventilatory support for 48 hours after extubation, whereas weaning failure is defined as the need for reintubation within 48 h following extubation. Once we have obtained the measure of the time and the speed, we have calculated the value of the acceleration for each patient. Hence, we have analyzed our data and we found a cut-off predictive value.
3.1 Data Analysis
We have measured the space and the time of contraction from the graph obtained by M-mode, and we have applied the form of the uniformly accelerated movement to the curve of each patient:
x = x0 + v0t + 1/2at2
where we consider x0 to be 0 mm, and v0 to be 0 mm/s, and we have obtained the following value, by explicating the acceleration:
a=2*s/t2
We have calculated it for each patient, and we have analyzed the results relating them to the outcome of the weaning.
3.2 Statistical Analysis
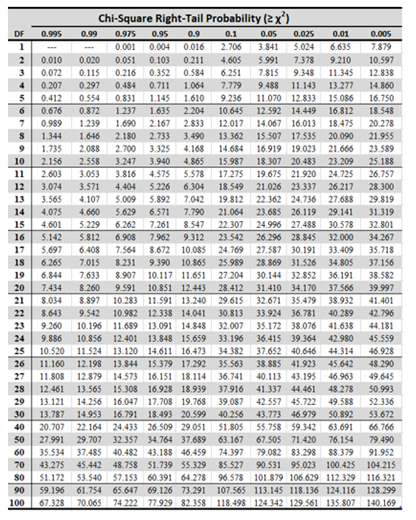
We have applied Mann-Whitney U test for independent measures. We have calculated the rank sum, and we have obtained the Ustat value. Then, we have compared it with the Ucrit value deriving from the table reported in Appendix A (critical values of the Mann-Whitney U test), obtaining our statistically significant result. Then we have used Chi-Square test to find out the difference between the observed and the expected data to analyze if there is a relationship between the entity of the diaphragmatic acceleration and the outcome of extubation.
Appendix A
4. Results
At the end of our analysis, 11 of our patients have had a successful weaning, whereas 8 have failed it. This result does not seem to correlate neither with the sex and the age of the patients (Table 1), nor with the time of intubation, the time of ICU stay or the duration of positivity for SARS-CoV2 (Table 1, 2).
|
Patient n. |
Sex |
Date of birth |
Date of the SARS-CoV2 test positivity |
Date of admission in the emergency department |
Date of admission in the ICU |
|
1 |
M |
01/01/1953 |
17/12/2020 |
17/12/2020 |
25/12/2020 |
|
2 |
M |
22/07/ 1943 |
09/04/2020 |
07/04/2020 |
08/04/2020 |
|
3 |
M |
18/07/1966 |
08/01/2021 |
13/01/2021 |
13/01/2021 |
|
4 |
M |
30/11/1958 |
13/11/2020 |
24/11/2020 |
11/12/2020 |
|
5 |
M |
24/11/1955 |
30/03/2020 |
30/03/2020 |
03/04/2020 |
|
6 |
M |
18/01/1953 |
11/04/2020 |
09/04/2020 |
14/04/2020 |
|
7 |
M |
27/02/1967 |
13/11/2020 |
13/11/2020 |
13/11/2020 |
|
8 |
M |
06/02/1950 |
23/03/2020 |
13/03/2020 |
23/03/2020 |
|
9 |
M |
11/09/1959 |
26/03/2021 |
26/03/2021 |
26/03/2021 |
|
10 |
M |
22/03/1946 |
02/04/2021 |
02/04/2021 |
02/04/2021 |
|
11 |
M |
22/03/1955 |
25/03/2021 |
27/03/2021 |
03/04/2021 |
|
12 |
M |
26/01/1944 |
18/03/2020 |
21/03/2020 |
25/03/2020 |
|
13 |
M |
04/04/1942 |
27/10/2020 |
05/11/2020 |
13/11/2020 |
|
14 |
F |
22/08/1958 |
11/12/2020 |
18/12//2020 |
21/12/2020 |
|
15 |
F |
12/08/1958 |
27/02/2021 |
27/02/2021 |
02/03/2021 |
|
16 |
M |
29/11/1961 |
- |
01/04/2020 |
04/04/2020 |
|
17 |
F |
13/10/1946 |
23/03/2021 |
26/03/2021 |
28/03/2021 |
|
18 |
M |
21/02/1950 |
19/03/2021 |
29/03/2021 |
06/04/2021 |
|
19 |
M |
25/11/1957 |
- |
20/03/2021 |
04/04/2021 |
Table 1: Characteristics of the enrolled patients, including sex, age, date of the SARS-CoV2 test positivity, date of admission in the emergency department and date of admission in the ICU.
On the patients enrolled, we have conducted the analysis with the UltraSound: using the B-mode, we have identified a point belonging to the diaphragm, to study its kinetics using the M-mode. The curve detected in M-mode represents the oscillation of a point of the diaphragm, and, due the tension and elastic forces involved in the system, we can consider it as a uniformly accelerated motion, defined by a constant acceleration. Hence, the above-mentioned curve can be assimilated to a space-time graph showing the motion of a material point, where the x-axis shows the time (t), and the y-axis the distance covered by the material point: the space (s), which is the amplitude of contraction (Figure 1). We have then calculated the acceleration for each patient, using the form a=2*s/t2: the obtained values are reported in Table 3. Our technique and the means through which we have obtained our results for each patient are shown in Figure 2.
|
Patient n. |
Date of the US test |
Ventilation mode during the test |
Date of extubation |
Ventilation mode at the extubation/death |
Time of intubation (days) |
|
1 |
27/01/2021 |
PSV 6+5; FiO2 0,35 |
30/01/2021 |
PSV 8+6, FiO2=0,35 |
38 |
|
2 |
24/04/2020 |
PSV 5+5; FiO2 0,45 |
24/04/2020 |
PSV 5+5, FiO2 =0,45 |
25 |
|
3 |
04/02/2021 |
SIMV/P: Pinsp=10, PEEP=6, FR=12/min FiO2=0,65 |
05/02/2020 |
PSV 8+6, FiO2= 0,5 |
32 |
|
4 |
08/12/2020 |
PSV 10+10, FiO2=0,4 |
08/12/2020 |
PSV 10+5, FiO2=0,4 |
14 |
|
5 |
17/04/2020 |
PSV 8+6, FiO2=0,45 |
19/04/2021 |
PSV 10+5, FiO2=0,4 |
16 |
|
6 |
30/04/2020 |
PSV 8+5, FiO2=0,5 |
03/05/2020 |
PSV 8+8, FiO2=0,4 |
19 |
|
7 |
21/11/2020 |
PSV 10+8, FiO2=0,5 |
21/11/2020 |
PSV 10+8, FiO2=0,5 |
12 |
|
8 |
20/04/2020 |
PSV 5+5, FiO2=0,45 |
20/04/2020 |
C-PAP 5+5, FiO2=0,35 |
27 |
|
9 |
13/04/2021 |
SIMV: (20+10), FiO2=0,6 |
Dead |
PCV: Pinsp=20, RR=22/min, PEEP=10, FiO2=0,5 |
29; dead |
|
10 |
12/04/2201 |
SIMV-P: Pinsp=14, RR= 15, PEEP=8, FiO2=0,5 |
tracheostomy in SB from 21/04/2021 |
PSV 10+5, FiO2=0,4 |
19 |
|
11 |
13/04/2021 |
PCV: FiO2=0,7 Pinsp=26 RR=22/min, PEEP=10 |
Dead |
PCV: Pinsp=26, RR=26/min, PEEP=5, FiO2=1 |
13; dead |
|
12 |
30/04/2020 |
PSV 10+10, FiO2= 0,4 |
Dead |
PSV 15+5, FiO2=0,5 |
46; dead |
|
13 |
26/11/2020 |
PSV 10+8, FiO2=0,4 |
26/11/2020 |
PSV 10+8, i FiO2=0,4 |
13 |
|
14 |
16/01/2021 |
NAVA 2,5, FiO2=0,8 |
Dead |
PCV: Pinsp=27, RR=26/min, PEEP=14, FiO2=0,9 |
37; Dead |
|
15 |
15/03/2021 |
SIMV-P: Pinsp=14, PEEP=10, FiO2=0,5 |
17/03/2021 |
C-PAP 8+8; FiO2=0,4 |
15 |
|
16 |
18/04/2020 |
PSV 18+8, FiO2=0,5 |
19/04/2020 |
PSV 18+8, FiO2=0,5 |
15 |
|
17 |
17/04/2021 |
PCV: Pinsp=28, RR=26/min, PEEP=10, FiO2=0,95 |
Dead |
PCV: Pinsp=30, RR=20/min, PEEP 8, FiO2=0,9 |
21; Dead |
|
18 |
17/04/2021 |
PCV: Pinsp=18 RR=20/min, PEEP=12, FiO2=0,9 |
Dead |
PCV: Pinsp=20, RR=22/min, PEEP=10, FiO2=0,9 |
24; Dead |
|
19 |
17/04/2021 |
PCV: Pinsp=26, RR=26/min, PEEP=10, FiO2=0,9 |
Dead |
PCV: Pinsp=30, RR=20/min, PEEP=8, FiO2=0,9 |
15; Dead |
Table 2: Date of the US test with the applied ventilation mode, date of the extubation with the associated ventilation mode, and time of intubation.
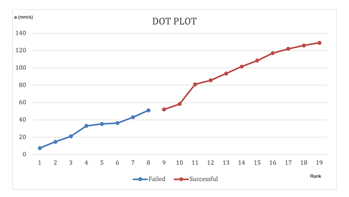
We can see that both positive and negative outcomes are associated to different values of acceleration: in particular, patients with a negative outcome have a value of acceleration from 52 mm/s2 to 128,9 mm/s2, whereas patients who failed the extubation have values included between 7,4 mm/s2 and 51 mm/s2, they are plotted in the graph of Figure 3. The median value of the population who failed extubation is far lower than the median value of the population with a successful extubation:
MedianFailed= 34,1mm/s2 < MedianSuccessful= 101,4 mm/s2.
Furthermore, we can identify an estimated cut-off value, 52 mm/s2. A value of acceleration inferior to 52 mm/s2 may well correlate with a negative outcome of weaning, whereas a value of acceleration superior to 52 mm/s2 may well be predictable of successful weaning.
|
Patient |
Space (S) mm |
Time (t) s |
Acceleration (a) mm/s2 |
Outcome |
|
n. |
||||
|
1 |
15,5 |
0,504 |
122,0 |
Successful |
|
2 |
55,2 |
1,376 |
58,3 |
Successful |
|
3 |
18,4 |
0,352 |
52,0 |
Successful |
|
4 |
27,2 |
0,814 |
81,7 |
Successful |
|
5 |
32,8 |
0,778 |
108,4 |
Successful |
|
6 |
31,8 |
0,736 |
117,0 |
Successful |
|
7 |
40,3 |
0,800 |
125,9 |
Successful |
|
8 |
48,7 |
0,869 |
128,9 |
Successful |
|
9 |
3,7 |
1,000 |
7,4 |
Failed |
|
10 |
20,6 |
1,112 |
33,0 |
Failed |
|
11 |
9,6 |
1,144 |
14,7 |
Failed |
|
12 |
44,9 |
1,024 |
85,6 |
Successful |
|
13 |
21,5 |
1,000 |
43,0 |
Failed |
|
14 |
5,63 |
0,347 |
93,5 |
Successful |
|
15 |
20,6 |
1,080 |
35,3 |
Failed |
|
16 |
31,8 |
0,729 |
101,4 |
Successful |
|
17 |
30,0 |
1,080 |
51,0 |
Failed |
|
18 |
17,6 |
0,984 |
36,3 |
Failed |
|
19 |
10,1 |
0,976 |
21,0 |
Failed |
|
Patient |
Space (S) mm |
Time (t) s |
Acceleration (a) mm/s2 |
Outcome |
|
n. |
||||
|
1 |
15,5 |
0,504 |
122,0 |
Successful |
|
2 |
55,2 |
1,376 |
58,3 |
Successful |
|
3 |
18,4 |
0,352 |
52,0 |
Successful |
|
4 |
27,2 |
0,814 |
81,7 |
Successful |
|
5 |
32,8 |
0,778 |
108,4 |
Successful |
|
6 |
31,8 |
0,736 |
117,0 |
Successful |
|
7 |
40,3 |
0,800 |
125,9 |
Successful |
|
8 |
48,7 |
0,869 |
128,9 |
Successful |
|
9 |
3,7 |
1,000 |
7,4 |
Failed |
|
10 |
20,6 |
1,112 |
33,0 |
Failed |
|
11 |
9,6 |
1,144 |
14,7 |
Failed |
|
12 |
44,9 |
1,024 |
85,6 |
Successful |
|
13 |
21,5 |
1,000 |
43,0 |
Failed |
|
14 |
5,63 |
0,347 |
93,5 |
Successful |
|
15 |
20,6 |
1,080 |
35,3 |
Failed |
|
16 |
31,8 |
0,729 |
101,4 |
Successful |
|
17 |
30,0 |
1,080 |
51,0 |
Failed |
|
18 |
17,6 |
0,984 |
36,3 |
Failed |
|
19 |
10,1 |
0,976 |
21,0 |
Failed |
Table 3: values of diaphragmatic acceleration of each patient, associated with the outcome of weaning.
4.1 Statistical Analysis
We have applied Mann-Whitney U test for independent measures (Wilcoxon rank-sum test). We have calculated the rank sum, and we have obtained the Ustat value.
Null hypothesis H0: the distributions of both populations are equal.
Alternative hypothesis H1: the distributions are not equal.
We assigned each observation to a Rank (Table 4), and we calculated the rank-sum for each population:
|
Failed |
Successful |
RANK |
|
7,4 |
1 |
|
|
14,7 |
2 |
|
|
21,0 |
3 |
|
|
33,0 |
4 |
|
|
35,3 |
5 |
|
|
36,3 |
6 |
|
|
43,0 |
7 |
|
|
51,0 |
8 |
|
|
52,0 |
9 |
|
|
58,3 |
10 |
|
|
81,0 |
11 |
|
|
85,6 |
12 |
|
|
93,5 |
13 |
|
|
101,4 |
14 |
|
|
108,4 |
15 |
|
|
117,0 |
16 |
|
|
122,0 |
17 |
|
|
125,9 |
18 |
|
|
128,9 |
19 |
Table 4: Ranks of Acceleration Values.
SFailed=1+2+3+4+5+6+7+8= 36
SSuccessful=9+10+11+12+13+14+15+16+17+18+19= 154
Ustat= S - n(n+1)/2
UstatS= 154 - 11(11+1)/2= 154 - 66= 88
UstatF= 36 - 8(8+1)/2= 36 – 36 = 0
UCrit= 13 (Appendix A) a=0,01
UstatF < UCrit with a=0,01
We reject H0, the difference between the two groups is statistically significant, it is not casual, so the distributions of populations are not equal (Figure 3).
4.2 Chi-Square Test
|
weaning failure |
successful weaning |
Total in the line |
||
|
0 |
11 |
a>52 mm/s2 |
11 |
|
|
8 |
0 |
a<52 mm/s2 |
8 |
|
|
Total in the column |
8 |
11 |
Total = 19 |
Table 5: Observed Values.
|
weaning failure |
successful weaning |
Total in the line |
||
|
5 |
6 |
a>52 mm/s2 |
11 |
|
|
3 |
5 |
a<52 mm/s2 |
8 |
|
|
Total in the column |
8 |
11 |
Total = 19 |
Table 6: Expected Values.
We have then calculated the c2 test, considering values reported in Table 4 and Table 5, and we have obtained:
c2= ∑(Oi – Ei)2/Ei =19
where
Oi = observed value (actual value)
Ei = expected value.
From the table reported in Appendix B, we deduce that we have found a correlation between the value of the acceleration and the outcome of extubation of 99,5%, considering a level of confidence of 0,05.
Appendix B
5. Discussion
Defining the right time for extubation remains a debated issue because of the difficulty in predicting the outcome before the maneuver. Moreover, it results to be even more challenging in patients who were affected by Covid-19 related ARDS (C-ARDS), because of the severity of the lung failure, the total amount, and the dosage of drugs in the ICU, and the aggressive prolonged mechanical ventilation. Therefore, a reliable method to make extubation as safe as possible is currently required. With regard to this subject, our study has demonstrated that an assessment of the diaphragm using US could well represent a usable and effective technique. It has been in fact broadly studied in literature, where the detection and the relationships between various parameters have been examined [4]. US is an available and easily usable bedside technique, cost effective and even though operator-dependent, repeatable, as we have focused on the detection of objective and measurable parameters. In this framework, our study highlights the use of B-mode to identify a point belonging to the diaphragm, and the use of M-mode to study the kinetics. The curve detected in M-mode represents the oscillation of a point of the diaphragm, and, due the tension and elastic forces involved in the system, we can consider it as a uniformly accelerated motion, defined by a constant acceleration. Hence, the above-mentioned curve can be assimilated to a space-time graph showing the motion of a material point, where the x-axis shows the time (t), and the y-axis the distance covered by the material point: the space (s) that is the amplitude of contraction. In particular, the uniform acceleration plays a pivotal role in our study, because it results to be directly proportional to the trans-diaphragmatic pressure, the gold standard parameter considered when it comes to the prediction of success or failure in weaning.
We can demonstrate as follows:
ΔP= resultant pressure acting on diaphragm, consisting of the trans-diaphragmatic pressure (;
a= acceleration of the diaphragmatic contraction.
The resultant force acting on the diaphragm is the force of the diaphragmatic contraction, corresponding to ΔP*Sd, where Sd is the area of the diaphragmatic surface.
Moreover, for Newton's second law of motion, the resultant force results to be md*a, where md is the diaphragm mass.
So we obtain the following system of equations:
F = md*a
F = ΔP*Sd
→ ΔP*Sd= md*a → a = (Sd/md)*ΔP
The pressure and the acceleration results to be directly proportional, and we can consider the physical quantity Sd/md a constant quantity, typical of each system, so it is different from one patient to another, but it is unnecessary to calculate, because our interest is on the fact that the two parameters are strictly related by a constant value that we can call k.
→a = k * ΔP.
Hence, we can demonstrate that the acceleration is related both to the force generated by the diaphragm contraction, and to the transdiaphragmatic pressure, a reliable measure rarely employed to decide the timing of weaning. Therefore, we can also consider our technique related to the measure of transdiaphragmatic pressure, but with the advantage of being non-invasive. To sum up, the outcome of extubation is not related to sex, age, mode of ventilation, or duration of ICU stay and of intubation. On the contrary, the calculated value of the acceleration is strongly correlated to the outcome of the weaning, so it represents a worth parameter which could play a pivotal role in the process of decision-making, detected with a bedside and cost-effective technique.
6. Conclusions
In conclusion, the acceleration, being directly proportional to the trans-diaphragmatic pressure, and to the force generated by diaphragm contraction, could well be a useful parameter to consider when it comes to the outcome of the weaning process. It is a reliable measure, bedside and cost effective. This is an observational pilot study, so more studies including a higher number of patients are needed to corroborate our findings.
Declarations
Ethical Approval and Consent to Participate
Approved by the ethical committee (comitato Etico per la Sperimentazione Clinica delle Province di Verona e Rovigo), Project number: 3658CESC. Written informed consent was obtained from all patients. All methods were carried out in accordance with relevant guidelines and regulations of ethical principles for medical research involving human, stated in the Declaration of Helsinki.
Availability of Data and Materials
All data generated or analysed during this study are included in this published article.
Consent for Publication
Not applicable.
Availability of supporting data
The data that support the findings of this study are openly available.
Competing Interests
I declare that the authors have no competing interests, or other interests that might be perceived to influence the results and/or discussion reported in this paper.
Funding
There is no funding in this study.
Authors' Contributions
G.G. and V.G. conceived the original idea. V.G. developed the theory and performed the computations. V.G. verified the analytical methods. G.G., A.B. and G.F. carried out the experiment. G.G. supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Acknowledgements
All the material is owned by the authors and/or no permissions are required.
References
- Fadila M, Rajasurya V, Regunath H. Ventilator Weaning. 2020 Nov 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2021).
- Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and Lung Ultrasound to Predict Weaning Outcome: Systematic Review and Meta-Analysis. Chest 152 (2021): 1140-1150.
- Qian Z, Yang M, Li L, et al. Ultrasound assessment of diaphragmatic dysfunction as a predictor of weaning outcome from mechanical ventilation: a systematic review and meta-analysis. BMJ Open 8 (2018): e021189.
- Li C, Li X, Han H, et al. Diaphragmatic ultrasonography for predicting ventilator weaning: A meta-analysis. Medicine (Baltimore) 97 (2018): e10968.
- Pham T, Brochard LJ, Slutsky AS. Mechanical Ventilation: State of the Art. Mayo Clin Proc 92 (2017): 1382-1400.
- Baptistella AR, Sarmento FJ, da Silva KR, et al. Predictive factors of weaning from mechanical ventilation and extubation outcome: A systematic review. J Crit Care 48 (2018): 56-62.
- Wawrzeniak IC, Regina Rios Vieira S, Almeida Victorino J. Weaning from Mechanical Ventilation in ARDS: Aspects to Think about for Better Understanding, Evaluation, and Management. Biomed Res Int 2018 (2018): 5423639.
- Vetrugno L, Guadagnin GM, Brussa A, et al. Mechanical ventilation weaning issues can be counted on the fingers of just one hand: part 1. Ultrasound J 12 (2020): 9.
- Matamis D, et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med 39 (2013): 801-810.
- de la Quintana Gordon FB, Nacarino Alcorta B, Fajardo Pérez M. Ultrasound evaluation of diaphragm function and its application in critical patients, mechanical ventilation, and brachial plexus block. Rev Esp Anestesiol Reanim 64 (2017): 513-521.
- Kilaru D, Panebianco N, Baston C. Diaphragm Ultrasound in Weaning From Mechanical Ventilation. Chest 159 (2021): 1166-1172.
- Dres M, Goligher EC, Heunks LMA, et al. Critical illness-associated diaphragm weakness. Intensive Care Med 43 (2017): 1441-1452.
- Carbognin S, Pelacani L, Zannoni F, et al. P246 Diaphragm ultrasonography: a method for weaning patients from mechanical ventilation. 36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium. 15-18 March 2016. Crit Care (2016).



 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 