Evaluating the Long-Term Effect of Shockwave Therapy in Treating Plantar Fasciitis
Shahina Sarker1*, Mohammad Muhibbur Rahman2, Monia Hafiz3, Md Arifur Rahman Chowdhury4, Suriya Shahaly5, Shamim Farhad6, Mehedi ABM7, Sayat Quayum8, Mohammad Moniruzzaman9
1Assistant Professor, Department of Physical Medicine and Rehabilitation, Savar Upuzilla Health Complex, Dhaka, Bangladesh
2Junior Consultant, Department of Physical Medicine & Rehabilitation, Government Employees Hospital, Dhaka, Bangladesh
3Consultant, Department of Physical Medicine and Rehabilitation, Farazy Hospital Ltd., Dhaka, Bangladesh
4Assistant Professor, Department of Physical Medicine and Rehabilitation, Rangpur Medical College, Rangpur, Bangladesh
5Assistant professor, Ahsania Mission Medical College, Dhaka, Bangladesh
6Medical Officer, Department of Physical Medicine and Rehabilitation, Govt. Employee Hospital, Dhaka, Bangladesh
7Medical Officer, Directorate General of Health Services, Dhaka, Bangladesh
8Assistant Professor, Department of Internal Medicine, International Medical College and Hospital, Dhaka, Bangladesh
9Professor and Head, Department of Physical Medicine & Rehabilitation, Dhaka Medical College, Dhaka, Bangladesh
*Corresponding Author: Shahina Sarker, Assistant Professor, Department of Physical Medicine and Rehabilitation, Savar Upuzilla Health Complex, Dhaka, Bangladesh.
Received: 20 October 2025; Accepted: 31 October 2025; Published: 05 December 2025
Article Information
Citation: Shahina Sarker, Mohammad Muhibbur Rahman, Monia Hafiz, Md Arifur Rahman Chowdhury, Suriya Shahaly, Shamim Farhad, Mehedi ABM, Sayat Quayum, Mohammad Moniruzzaman. Evaluating the Long-Term Effect of Shockwave Therapy in Treating Plantar Fasciitis. Journal of Orthopedics and Sports Medicine. 7 (2025): 532-537.
View / Download Pdf Share at FacebookAbstract
Background: Plantar fasciitis affects over two million people annually, with women nearly twice as susceptible. Conventional treatments often provide only temporary relief, whereas Extracorporeal Shock Wave Therapy (ESWT) has long-term effects in reducing pain and improving function as a non-invasive option.
Aim: To evaluate the long-term effect of ESWT in reducing pain and improving functional outcomes among patients with plantar fasciitis.
Methods: This quasi-experimental study was conducted in the Department of Physical Medicine and Rehabilitation, Dhaka Medical College, from July 2019 to June 2020. Forty-six patients were enrolled by purposive sampling, and 39 completed the study. All participants received ESWT along with NSAIDs, stretching exercises, massage, heel pads, and activity modification. ESWT was applied three times weekly for three weeks. Pain and function were assessed using the Visual Analogue Scale (VAS) and Foot Function Index (FFI) at baseline and at 1, 2, 4, 12, 24, and 48 weeks. Data were analyzed using repeated-measures ANOVA in SPSS version 25 with a 5% significance level.
Results: Among 39 participants (mean age 45.66 ± 7.39 years, BMI 24.29 ± 3.11 kg/m²), 53.8% were male, and 59.0% had left-sided involvement. The mean VAS pain score decreased significantly from 8.82 ± 0.88 to 1.66 ± 0.77, and FFI score from 59.65 ± 5.43 to 10.10 ± 3.23 at 48 weeks (p < 0.001).
Conclusion: ESWT is a safe, effective, and durable treatment for plantar fasciitis, producing significant pain relief and functional improvement up to 48 weeks. It may be considered a first-line therapy, especially for patients unresponsive to conventional management.
Keywords
<p>Plantar fasciitis; Extracorporeal shockwave therapy; Foot diseases; Pain measurement</p>
Article Details
1. Introduction
Plantar fasciitis (PF) is a widespread soft tissue ailment in adults, caused by an inflammatory response and deterioration of the plantar fascia origin due to recurrent micro-trauma [1,2]. Over 2 million individuals seek treatment for heel pain annually [3]. The unadjusted incidence rate of plantar fasciitis was 10.5 per 1000 person-years [4].
Women exhibited a notably higher adjusted incidence rate ratio of 1.96 for plantar fasciitis compared to men (95% confidence interval, 1.94 to 1.99) [5]. The common risk factors for plantar fasciitis include irregular gait, leg-length inequality (LLI), excessive foot pronation, weakened external and internal foot muscles, increased body mass index (BMI), and thinning of the plantar fat pad [6].
Treatment for plantar fasciitis involves anti-inflammatory interventions, activity adjustments, stretching exercises, customized footwear, and recommendations for taping and patient education. Shockwave therapy and platelet-rich plasma are proposed for cases that do not respond to standard conservative approaches [6-8]. Conventional treatments for plantar fasciitis, such as stretching, orthotics, NSAIDs, and physical therapy, often provide temporary relief, show limited effectiveness in chronic cases, and pose risks like side effects, high costs, and recurrence. Invasive options like surgery carry complication risks, while misdiagnosis and untreated contributing factors can hinder success [9,10].
Extracorporeal shock wave therapy (ESWT) is a noninvasive treatment method derived from extracorporeal shock wave lithotripsy (ESWL) [11]. ESWT has consistently been proven to alleviate pain intensity in individuals with plantar fasciitis. A systematic review and meta-analysis revealed substantial pain reductions, as measured by the Visual Analogue Scale (VAS), for both focal and radial ESWT applications [12]. Furthermore, a randomized controlled trial showed that patients undergoing ESWT experienced a statistically significant decrease in VAS scores compared to those receiving conventional treatments alone [13].
ESWT not only alleviates pain but also enhances functional outcomes. Studies have reported improvements in foot function indices and gait parameters, such as stride length and walking speed, following ESWT treatment [13,14]. The therapy has been found effective in both short-term and long-term follow-ups, with significant improvements in foot function and activity levels [14].
When compared to other conservative treatments, ESWT has been identified as one of the most effective methods for treating plantar fasciitis. It is often used in conjunction with other therapies, such as stretching exercises, to enhance treatment outcomes [15,16]. Notably, the combination of ESWT with calf muscle stretching exercises has shown superior results in pain reduction and functional improvement compared to ESWT alone [15].
2. Materials and Methods
This quasi-experimental study was carried out in the Department of Physical Medicine and Rehabilitation at Dhaka Medical College, Bangladesh, from July 2019 to June 2020, following approval from the institutional ethics committee (MEU-DMC/ECC/2019/307). 46 patients with plantar fasciitis were initially enrolled through purposive sampling, with 39 participants completing the study. Adults aged 40–70 years, of either gender, experiencing unilateral heel pain aggravated by walking or extended standing and reporting a Visual Analogue Scale (VAS) pain score above 4 were included. Exclusion criteria encompassed infections, vascular or neurological disorders, inflammatory conditions, recent injuries, or unstable ankle joints. After obtaining informed consent, all participants underwent an assessment for plantar pain. Pre-treatment evaluations included complete blood counts and plain X-rays of the calcaneus. Participants received Extracorporeal Shock Wave Therapy (ESWT) alongside NSAIDs, stretching, intrinsic foot muscle strengthening exercises, deep friction massage, topical NSAIDs, heel pads, and activity adjustments. ESWT was administered at a frequency of 4 Hz in continuous mode, with 3-bar pressure, and 1000 shocks per session, three times per week for three weeks. Follow-ups were conducted at 1, 2, 4, 12, 24 and 48 weeks, where pain levels were measured using the VAS and foot functionality was evaluated through the Foot Function Index (FFI). The FFI consists of 23 self-administered items categorized into pain, disability, and activity limitation subscales. Data were analyzed using SPSS version 25. Data were analyzed by repeated measure ANOVA test, considering a 0.05 (5%) level of significance and 95% CI.
2.1 Study flow chart

3. Result
The study participants had a mean age of 45.66±7.39 years and a mean BMI of 24.29±3.11 kg/m². Males comprised 53.8% (n=21) of the sample. Left-sided plantar fasciitis was more prevalent, affecting 59.0% (n=23) of the participants. The average duration of symptoms was 4.92±2.56 months, while the mean daily standing time was 6.74±2.92 hours (Table 1)
|
Variables |
Mean ±SD |
|
|
Age (in years) |
45.66±7.39 |
|
|
BMI (kg/m2) |
24.29±3.11 |
|
|
Male, n (%) |
21 |
53.8 |
|
Left-sided injury, n (%) |
23 |
59 |
|
Duration of symptoms (in months) |
4.92±2.56 |
|
|
Standing hours (per day) |
6.74±2.92 |
|
Table 1: Baseline characteristics of the patients.
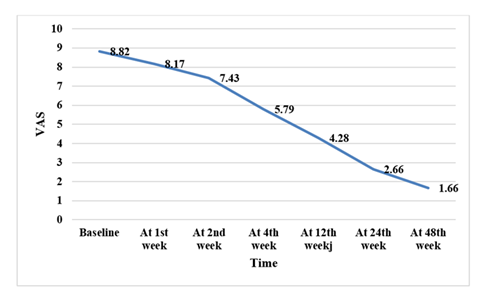
The mean VAS pain score decreased from 8.82±0.88 at baseline to 1.66±0.77 by the 48th week, showing a steady decline over time. The reduction was statistically significant (p < 0.001) (Table 2 and Figure 1).
|
VAS |
Baseline |
1st |
2nd |
4th |
12th |
24th |
48th |
|
week |
week |
week |
week |
week |
week |
||
|
Mean±SD |
8.82±0.88 |
8.17±1.09 |
7.43±1.27 |
5.79±1.00 |
4.28±0.91 |
2.66±0.77 |
1.66±0.77 |
|
p-value |
<0.001a |
||||||
a= Repeated measure ANOVA
Table 2: Comparison of VAS scores at different time points.
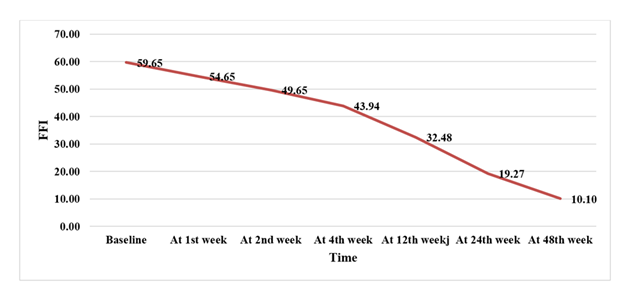
The mean Foot Function Index (FFI) score declined from 59.65±5.43 at baseline to 10.10±3.23 by the 48th week, indicating progressive improvement. The reduction was statistically significant (p < 0.001) (Table 3 and Figure 2).
|
FFI |
Baseline |
1st |
2nd |
4th |
12th |
24th |
48th |
|
week |
week |
week |
week |
week |
week |
||
|
Mean±SD |
59.65±5.43 |
54.65±5.43 |
49.65±5.43 |
43.94±5.15 |
32.48±3.65 |
19.27±4.53 |
10.10±3.23 |
|
p-value |
<0.001a |
||||||
a= Repeated measure ANOVA
Table 3: Comparison of FFI scores at different time points.
4. Discussion
This study evaluated the long-term efficacy of extracorporeal shock wave therapy (ESWT) in reducing pain and improving function in patients with plantar fasciitis. The findings demonstrated sustained improvement up to 48 weeks, supporting ESWT as an effective and durable treatment option for long-term management of plantar fasciitis.
In this study, mean BMI was 24.29±3.11 and the average age was 45.66±7.39 years. Our findings were consistent with previous studies indicating that a higher BMI increases the risk of plantar fasciitis [17,18]. The average standing time was 6.74±2.92 hours, reinforcing the role of mechanical factors and weight-bearing activities in plantar fasciitis [18,19].
Pain reduction, as measured by VAS scores, demonstrated a significant decline over time. Notably, ESWT showed considerable reduction in pain intensity across the studies reviewed. Our findings align with existing literature, as they demonstrate pain reduction similar to the results reported by Leão et al. [20], Gollwitzer et al. [21] and Dastgir [22], who observed significant VAS improvements at 12 and 24 weeks, respectively. Lai et al. [23] reported significantly greater pain relief on the VAS scale with corticosteroid injection (P=0.001 at 4 weeks and P<0.001 at 12 weeks). Previous meta-analyses had also shown a significant decrease in VAS scores for both f-ESWT (-2.818, SE 0.803, 95% CI [-4.393, -1.244], P<0.0001) and r-ESWT (-3.038, SE 0.428, 95% CI [-3.878, -2.199], P<0.0001), indicating their effectiveness in pain relief for plantar fasciitis patients [12]. This supports the potential of shockwave therapy as an effective treatment, offering rapid pain relief that persists over time.
Similarly, functional improvement, assessed through FFI scores showed significant reductions over time. The progressive decline in FFI scores reflects enhanced foot function and reduced disability, underscoring the clinical benefits of the ESWT.
The FFI traditional version was assessed in two studies [24,25], and there were significant improvements at one-month post-treatment (P≤0.001) [24], six weeks (P<0.01) [25], and three months (P<0.01) [25]. The FFI revised version (FFI-R) demonstrated significant improvements at six months (P<0.001) [26,27]. The pain subscale (PS-FFI) was studied in two research papers: Bahar-Ozdemir et al. [24] found significant improvements (P<0.05). Concurrently, Rompe et al. [28] reported significant advantages for PFSS with ESWT versus ESWT (P<0.001). The FFI-DS was addressed by two studies: Bahar-Ozdemir et al. [24] reported significant within-group changes (P<0.05). However, Takla et al. [29] reported significant within-group changes (P<0.0001) and significant between-group changes (PBMT+ESWT, ESWT, and PBMT) (P<0.0001). ESWT was also superior to PBMT in enhancing physical function (P<0.0001). The activity subscale (FFI-AS), assessed by Bahar-Ozdemir et al. [24], showed post-treatment gains (P<0.05) with no inter-group differences (P=NS). Tognolo et al. [30] also reported significant gains in the Italian FFI (17-iFFI) for both groups (P<0.0001), with a further advantage for the low-intensity f-ESWT myofascial point group (P=0.0016).
5. Limitations
This study has certain limitations, such as a relatively small sample size, the absence of a placebo-controlled group, and a single-center design, which may restrict the broader applicability of the findings. Furthermore, long-term outcomes and patient-reported quality of life were not evaluated, which could have an impact on the results.
6. Conclusion
ESWT is a safe, effective, and non-invasive therapy for plantar fasciitis, offering sustained pain relief and functional improvement up to 48 weeks. Its long-term efficacy supports its use as a preferred option, though larger multi-center studies with extended follow-up are needed to confirm these results.
Acknowledgements:
None.
Author Contributions:
Shahina Sarker: Critical intellectual input, study concept and design, methodology, writing of the manuscript draft, study supervision, read and approved the final version. Mohammad Muhibbur Rahman: Critical intellectual input, study concept and design, methodology, revision for important intellectual content, read and approved the final version. Monia Hafiz: Critical intellectual input, study concept and design, methodology, read and approved the final version. Md. Arifur Rahman Chowdhury: Critical intellectual input, study concept and design, methodology, read and approved the final version. Suriya Shahaly: Critical intellectual input, study concept and design, methodology, read and approved the final version. Shamim Farhad: Critical intellectual input, writing of the manuscript draft, read and approved the final version. A. B. M. Mehedi: Critical intellectual input, revision for important intellectual content, read and approved the final version. Sayat Quayum & Mohammad Moniruzzaman: Critical intellectual input, revision for important intellectual content, read and approved the final version.
Funding:
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest:
The authors declare no conflict of interest.
References
- Palomo López P, Becerro De Bengoa Vallejo R, Losa-Iglesias ME, et al. Impact of plantar fasciitis on the quality of life of male and female patients. JPR 11 (2018): 875-880.
- Ali Q, Long Y, Ali M. Prevalence, causes, and treatment of plantar fasciitis in young females of a medical college. Bull Fac Phys Ther 29 (2024): 31.
- Luffy L, Grosel J, Thomas R, et al. Plantar fasciitis: A review of treatments. JAAPA 31 (2018): 20-24.
- Nahin RL. Prevalence and pharmaceutical treatment of plantar fasciitis in United States adults. J Pain 19 (2018): 885-896.
- Goweda R, Alfalogy E, Filfilan R, et al. Prevalence and risk factors of plantar fasciitis among patients with heel pain. J High Inst Public Health 45 (2015): 71-75.
- Rabadi D, Seo S, Wong B, et al. Immunopathogenesis, early detection, therapies, and prevention of plantar fasciitis: A concise review. Int Immunopharmacol 110 (2022): 109023.
- Morrissey D, Cotchett M, Said J’Bari A, et al. Management of plantar heel pain: a best practice guide. Br J Sports Med 55 (2021): 1106-1118.
- Rhim HC, Kwon J, Park J, et al. Epidemiology, evaluation, and treatment of plantar fasciitis: a systematic review of reviews. Life 11 (2021): 1287.
- Trojian T, Tucker AK. Plantar fasciitis. Am Fam Physician 99 (2019): 744-750.
- Latt LD, Jaffe DE, Tang Y, et al. Evaluation and treatment of chronic plantar fasciitis. Foot Ankle Orthop 5 (2020): 2473011419896763.
- Auersperg V, Trieb K. Extracorporeal shock wave therapy: an update. EFORT Open Rev 5 (2020): 584-592.
- Lippi L, Folli A, Moalli S, et al. Efficacy and tolerability of extracorporeal shock wave therapy in plantar fasciopathy: a systematic review. Eur J Phys Rehabil Med 60 (2024): 832-846.
- Saleh AM, ELNaggar EMK, El Sayed AS, et al. Effect of extracorporeal shockwave on gait parameters in plantar fascitis. Bull Fac Phys Ther 29 (2024): 64.
- Tezen Ö, Bilir EE, Arslan HB, et al. Effectiveness of extracorporeal shock wave therapy: radial vs focused applications. J Foot Ankle Surg 64 (2025): 36-41.
- Muradova AMY, Kozlov VV. Pain assessment in plantar fasciitis treated by shock wave therapy. SJLSA 16 (2024): 306-316.
- Ovchynnikov OM, Bludova MO, Merkulova TV, et al. Effectiveness of shock wave therapy vs other treatments for plantar fasciitis: a review. Medicni Perspektivi 29 (2024): 20-26.
- Riddle DL, Pulisic M, Sparrow K. Impact of demographic and impairment variables in plantar fasciitis. Foot Ankle Int 25 (2004): 311-317.
- El Molla SS, Fahmy AM, Gamil AM, et al. Evaluation of plantar fasciitis improvement after shock wave therapy by ultrasonography. Egypt Rheumatol Rehabil 48 (2021): 43.
- Riddle DL, Pulisic M, Pidcoe P, et al. Risk factors for plantar fasciitis: a matched case-control study. J Bone Joint Surg Am 85 (2003): 872-877.
- Leão RG, Azuma MM, Ambrosio GHC, et al. Effectiveness of shockwave therapy in plantar fasciitis. Acta Ortop Bras 28 (2020): 7-11.
- Gollwitzer H, Diehl P, Von Korff A, et al. Shock wave therapy for chronic painful heel syndrome. J Foot Ankle Surg 46 (2007): 348-357.
- Dastgir N. Extracorporeal shock wave therapy for plantar fasciitis. J Pak Med Assoc 64 (2014): 675-678.
- Lai TW, Ma HL, Lee MS, et al. ESWT vs corticosteroid injections for chronic plantar fasciitis. J Musculoskelet Neuronal Interact 18 (2018): 47-54.
- Bahar-Ozdemir Y, Atan T. Kinesio taping vs ESWT in plantar fasciitis: randomized trial. Int J Clin Pract 75 (2021): 12.
- Kesikburun S, Uran Şan A, Kesikburun B, et al. Ultrasound-guided prolotherapy vs ESWT in chronic plantar fasciitis. J Foot Ankle Surg 61 (2022): 48-52.
- Uğurlar M, Sönmez MM, Uğurlar ÖY, et al. Four treatment modalities for chronic plantar fasciitis: 36-month follow-up. J Foot Ankle Surg 57 (2018): 913-918.
- Wheeler PC, Dudson C, Calver R. Radial ESWT vs minimal-dose ESWT in chronic plantar fasciopathy. Foot Ankle Surg 28 (2022): 1356-1365.
- Rompe JD, Furia J, Cacchio A, et al. Shock wave treatment vs combined stretching for heel pain. Int J Surg 24 (2015): 135-142.
- Takla MKN, Rezk SSRA. Photobiomodulation + ESWT for plantar fasciitis: randomized trial. Lasers Med Sci 34 (2019): 583-593.
- Tognolo L, Giordani F, Biz C, et al. Myofascial points treatment with f-ESWT for plantar fasciitis. Eur J Phys Rehabil Med 58 (2022): 85-93.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 