Functional Outcome of Biological Graft Versus Fiber Wire in Acromioclavicular Joint Dislocation: A Comparative Study
Dr. Vipin Kumar Raghuwanshi1, Dr. Sandeep Bhinde2*, Dr. Shubham Nagdev3, Dr. Abhishek Dhoke4, Dr. Vinayak Mani Dwivedi5
1Senior Resident, Department of Orthopaedics, Dr. Laxminarayan Panday, Govt Medical College, Ratlam, Madhya Pradesh, India
2Associate Professor, Department of Orthopaedics, RD. Gardi Medical College, Ujjain, Madhya Pradesh, India
3Senior Resident, Department of Orthopaedics, RD. Gardi Medical College, Ujjain, Madhya Pradesh, India
4Senior Resident, Department of Orthopaedics, Shyam Shah Medical College, Rewa, Madhya Pradesh, India
5Senior Resident, Department of Orthopaedics, MGM Medical College, Indore, Madhya Pradesh, India
*Corresponding Author: Dr. Sandeep Bhinde, Associate Professor, Department of Orthopaedics, RD Gardi Medical College, Ujjain, Surasa, Madhya Pradesh, India.
Received: 24 June 2025; Accepted: 01 July 2025; Published: 08 July 2025
Article Information
Citation: Vipin Kumar Raghuwanshi, Sandeep Bhinde, Shubham Nagdev, Abhishek Dhoke, Vinayak Mani Dwivedi. Functional Outcome of Biological Graft Versus Fiber Wire in Acromioclavicular Joint Dislocation: A Comparative Study. Journal of Orthopedics and Sports Medicine. 7 (2025): 328-336.
View / Download Pdf Share at FacebookAbstract
Introduction: Acromioclavicular (AC) joint dislocation is a common shoulder injury, particularly among athletes and individuals engaged in physical labor. The injury often requires surgical intervention to restore joint stability and function. Two popular surgical options are the use of biological grafts and synthetic materials such as Fiber Wire for AC joint reconstruction. This comparative study aims to evaluate the efficacy, safety, and functional outcomes of biological grafts versus fiber wire in the treatment of AC joint dislocations.
Materials and Methods: This study included a sample of 32 patients diagnosed with AC joint dislocation, divided into two groups: those treated with biological grafts and those treated with fiber wire. Patients were randomly assigned to each group and followed for a period of 12 months post-surgery. Clinical evaluations were performed using the Constant-Murley Score. Radiographic assessments were conducted to measure joint stability and alignment. Complications, such as infections and redislocations, were recorded.
Results: The study found that patients treated with biological grafts demonstrated slightly better joint stability and fewer complications compared to those treated with fiber wire. The Constant Murley indicated that the biological graft group achieved superior functional outcomes, with statistically significant differences (p < 0.05).
Conclusion: Both biological grafts and fiber wire provide viable options for AC joint dislocation repair, each with distinct advantages. Biological grafts offer better long-term stability and functional outcomes, making them preferable for patients prioritizing joint integrity and performance. Further research with larger sample sizes and longer follow-up periods is necessary to substantiate these findings and optimize treatment protocols.
Keywords
<p>Acromioclavicular joint (AC joint); Biological graft; Fiber wire; Athletes; Constant-Murley Score; Shoulder</p>
Article Details
1. Introduction
The acromioclavicular (AC) joint, a vital articulation between the clavicle (collarbone) and the acromion process (scapular projection), plays a crucial role in shoulder girdle stability and function. Disruption of this joint, known as acromioclavicular joint dislocation, represents a prevalent injury within the spectrum of shoulder girdle trauma, accounting for 9% to 12% of all such occurrences [1]. The most common etiology is direct trauma to the AC joint or lateral trauma providing an axial load on the joint space. AC dislocations are distinct from "shoulder dislocations," which refer to glenohumeral joint dislocations [2]. These dislocations typically arise from direct blows to the shoulder or falls onto an outstretched arm with the arm positioned inwards (adducted) [3]. ACjoint dislocations are more prevalent in men than women, and they can affect individuals of any age and activity level [4]. AC joints are especially prevalent in the younger population participating in contact sports, representing 15%, 20%, and 41% of shoulder injuries in hockey, skiing, and American football, respectively [5].
The cornerstone of effective treatment hinges on accurately classifying the injury severity. The widely employed Rockwood classification system categorizes acromioclavicular dislocations into six distinct types (I-VI) based on the degree of ligamentous disruption [6]. Rockwood types I and II, characterized by minimal ligamentous damage, are managed conservatively through conservative techniques like using an ice pack, immobilization with a sling for several weeks, and physical therapy, taking anti-inflammatory over-the-counter drugs. Whereas in the Rockwood types III to VI, encompassing more severe ligamentous injuries with significant joint instability, oftennecessitate surgical intervention [7].
Surgical management for acromioclavicular joint dislocations encompasses a diverse array of techniques, broadly classified into four categories: Fixation with Hardware—This approach involves utilizing screws, Kirschner wires (K-wires), or a combination of both to directly secure the AC and/or coracoclavicular (CC) ligaments [8], or suture button or anchor fixation [9]. Also, in cases involving substantial ligamentous avulsion, reconstruction may be performed using autografts (tissue harvested from the patient) or allografts (donor tissue) to recreate the disrupted ligaments [10].
Evaluating the success of any treatment strategy for acromioclavicular joint dislocations necessitates using validated outcome measures. The Constant-Murley score (CMS) is a widely utilized and reliable tool for comprehensively assessing patient function and recovery following this injury. This study employed the CMS score as the primary outcome measure to assess patient function and recovery following each surgical approach. It evaluates four domains: pain, activities of daily living, range of motion, and strength.
Despite the existence of various surgical techniques, the optimal approach for managing acromioclavicular joint dislocations, particularly for Rockwood type III injuries, remains a subject of ongoing debate. While some surgeons advocate for conservative management for this type, others favor a surgical approach to achieve enhanced stability and potentially improve long-term outcomes [13].
This study aimed to contribute to the ongoing debate regarding the optimal surgical management of Rockwood type III acromioclavicular joint dislocations by comparing two prevalent surgical techniques: biological graft fixation and suture button fixation. By comparing the CMS scores between these two groups, the study sought to determine which technique yields superior patient outcomes regarding pain reduction, daily living function, range of motion, and strength. Secondary outcome measures were also evaluated, including radiographic assessment of joint stability, patient satisfaction scores, and complication rates associated with each surgical method. This study offered high-quality data to discuss the most effective surgical approach for managing Rockwood type III acromioclavicular joint dislocations.
2. Methods and Materials
The proposed study was conducted after approval by the research guide and institutional ethics committee and is anticipated to be completed within one year. The study was conducted at the Department of Orthopaedics at R D Gardi Medical College, Ujjain.
2.1 Selection Criteria:
a. Inclusion Criteria
- • Adult patients with Rockwood types III, IV, V, and VI of acromioclavicular joint dislocation.
- • Age >18 years and <65 years.
- • Patients who have given consent
- • Acromioclavicular joint dislocation duration: <3 months.
b. Exclusion Criteria
- • Patients with Rockwood type I or II acromioclavicular joint dislocation
- • Age <18 years and >65 years.
- • Patients with comorbidities.
- • Patient who refuses surgical treatment.
- • Acromioclavicular joint dislocation duration >3 months.
2.2 Methodology:
The study was conducted at R D Gardi Medical College, Ujjain, upon approval by the ethical committee within the Department of Orthopaedics on patients with complaints of pain in the shoulder region by using a self-administered knowledge questionnaire after obtaining permission from concerned authorities in the department to conduct the main study.
2.3 Sample size calculation
All statistical analyses were conducted using suitable statistical software. Quantitative data was analyzed using frequency distribution, measures of central tendency and dispersion, and graphical representation. Qualitative data was analyzed using frequency distribution, percentage calculations, and diagrammatic representations. A comparison of quantitative variables was done using both parametric and non-parametric tests.
2.4 Surgical technique
Surgery was performed under general anesthesia.
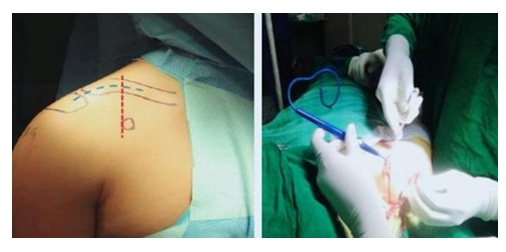
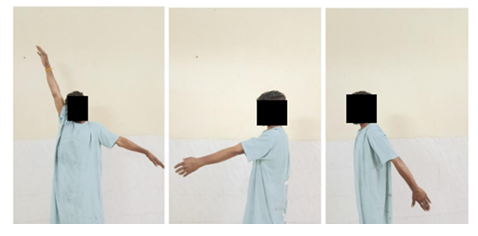
2.4.1 Position: Beech Chair Position (Figure 1-6)
Wound closure and cleaning and dressing done.
Surgical procedure is same in reconstruction with biological graft. In it tendon graft is used in place of fiber wire to reconstruct acromioclavicular joint.
2.4.2 Steps for graft harvest and preparation:
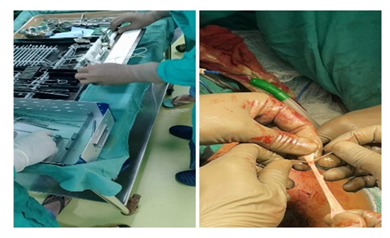
- Graft Harvest – A small incision is made near hamstring insertion (Figure 7,8).
Tendon is taken with the help of tendon stripper.
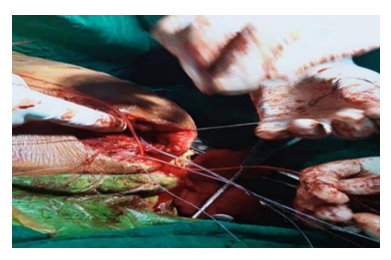
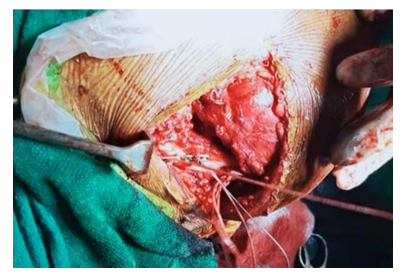
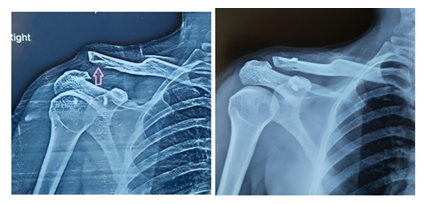
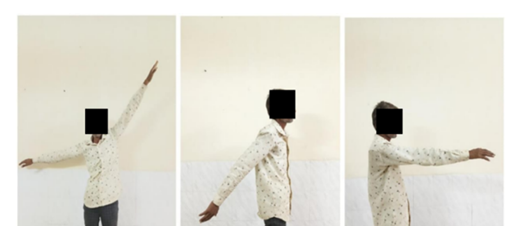
2.4.3 A case of biological reconstruction (Figure 9-13):
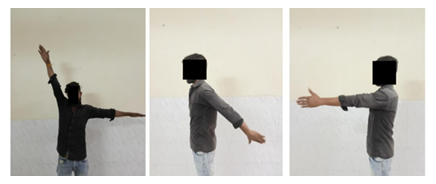
2.4.4 A case of fiber wire reconstruction (Figure 14-18):
3. Results
Present study, most frequently occurring age is 25 years. The standard deviation of 7.749 years reflects moderate variability in the ages within the sample. The ages range from a minimum of 21 years to a maximum of 48 years (Table 1-4; Figure 19 and 20).
|
Age group |
N |
% |
|
<=30 years |
15 |
46.9% |
|
31 - 40 years |
10 |
31.3% |
|
>41 years |
7 |
21.9% |
|
Total |
32 |
100.0% |
Table 1: Age distribution of the cases.
|
Side affected |
N |
% |
|
Left |
12 |
37.5% |
|
Right |
20 |
62.5% |
|
Total |
32 |
100.0% |
Table 2: Side affected of the cases.
|
Complications |
N |
% |
|
None |
29 |
90.6% |
|
Subluxation |
2 |
6.3% |
|
superficial infection |
1 |
3.1% |
|
Total |
32 |
100.0% |
Table 3: Complications.
|
Group |
p |
|||||
|
Biological graft |
Fibre wire |
|||||
|
Complications |
None |
14 |
87.5% |
15 |
93.8% |
0.596 |
|
Subluxation |
1 |
6.3% |
1 |
6.3% |
||
|
superficial infection |
1 |
6.3% |
0 |
0.0% |
||
Table 4: Cross tabulation between complication and study group.
The data compares the occurrence of complications between the Biological Graft and Fiber Wire treatment groups. Among those with no complications, 87.5% received Biological Graft and 93.8% received Fiber Wire. Subluxation occurred in 6.3% of cases in both groups. Superficial infection was reported in 6.3% of cases in the Biological Graft group and none in the Fibre Wire group. The p-value of 0.596 indicates no statistically significant difference in the distribution of complications between the two treatment groups (Table 5).
|
Group |
N |
Mean pre op CMS |
Std. Deviation |
t |
p |
|
Biological graft |
16 |
35.56 |
5.416 |
-.294 |
.771 |
|
Fiber wire |
16 |
36.13 |
5.402 |
Table 5: Comparison of mean pre-operative CMS according to groups.
The Table 5 compares the mean pre-operative Constant-Murley Scores (CMS) between the Biological Graft and Fiber Wire treatment groups. For the Biological Graft group, the mean pre-op CMS is 35.56 with a standard deviation of 5.416. For the Fiber Wire group, the mean pre-op CMS is 36.13 with a standard deviation of 5.402. The t-value is -0.294, and the p-value is 0.771, indicating that the difference in the mean pre-op CMS between the two groups is not statistically significant. This suggests that there is no significant difference in the pre-operative functional status of patients between the Biological Graft and Fiber Wire groups (Table 6, Figure 21).
|
Group |
N |
Mean post op CMS 6 weeks |
Std. Deviation |
t |
p |
|
Biological graft |
16 |
63.00 |
4.412 |
.523 |
.605 |
|
Fiber wire |
16 |
62.25 |
3.661 |
Table 6: Comparison of mean post-operative CMS at 6 weeks according to groups.
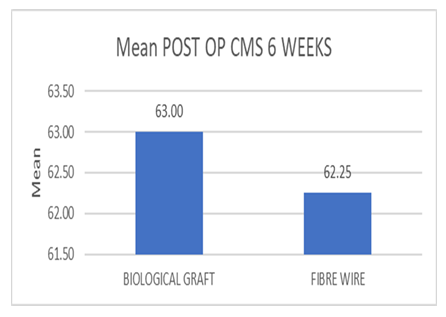
The Table 6 compares the mean post-operative Constant-Murley Scores (CMS) at 6 weeks between the Biological Graft and Fiber Wire treatment groups. For the Biological Graft group, the mean post-op CMS at 6 weeks is 63.00 with a standard deviation of 4.412. For the Fiber Wire group, the mean post-op CMS at 6 weeks is 62.25 with a standard deviation of 3.661. The t-value is 0.523, and the p-value is 0.605, indicating that the difference in the mean post-op CMS at 6 weeks between the two groups is not statistically significant. This suggests that there is no significant difference in the post-operative functional status at 6 weeks between patients treated with Biological Grafts and those treated with Fiber Wire (Figure 22).
|
Group |
N |
Mean post op CMS 6 months |
Std. Deviation |
t |
p |
|
Biological graft |
16 |
91.06 |
6.787 |
2.107 |
.044 |
|
Fibre wire |
16 |
85.94 |
6.971 |
Table 7: Comparison of mean post-operative CMS 6 month according to groups.
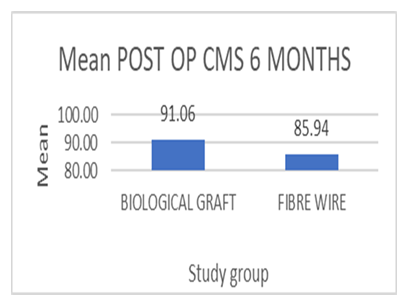
The Table 7 compares the mean post-operative Constant-Murley Scores (CMS)(14) at 6 months between the Biological Graft and Fibre Wire treatment groups. For the Biological Graft group, the mean post-op CMS at 6 months is 91.06 with a standard deviation of 6.787. For the Fibre Wire group, the mean post-op CMS at 6 months is 85.94 with a standard deviation of 6.971. The t-value is 2.107, and the p-value is 0.044, indicating that the difference in the mean post-op CMS at 6 months between the two groups is statistically significant. This suggests that patients treated with Biological Grafts have a significantly better functional status at 6 months post-operation compared to those treated with Fiber Wire (Figure 23).
|
Group |
N |
Mean POST OP CMS12 MONTHS |
Std. Deviation |
t |
p |
|
BIOLOGICAL GRAFT |
16 |
95.25 |
2.543 |
3.258 |
.003 |
|
FIBRE WIRE |
16 |
92.50 |
2.221 |
Table 8: Comparison of mean post-operative CMS 12 month according to groups.
The Table 8 compares the mean post-operative Constant-Murley Scores (CMS) at 12 months between the Biological Graft and Fiber Wire treatment groups. For the Biological Graft group, the mean post-op CMS at 12 months is 95.25 with a standard deviation of 2.543. For the Fiber Wire group, the mean post-op CMS at 12 months is 92.50 with a standard deviation of 2.221. The t-value is 3.258, and the p-value is 0.003, indicating that the difference in the mean post-op CMS at 12 months between the two groups is statistically significant. This suggests that patients treated with Biological Grafts have a significantly better functional status at 12 months post-operation compared to those treated with Fiber Wire.
4. Discussion
Acromioclavicular (AC) dislocation involves the complete loss of articular contact. It is considered chronic when it occurs after conservative management or unsuccessful surgical treatment [11]. This study compares the use of biological graft and fiber wire in the treatment of acromioclavicular joint dislocation.
4.1 Age and Gender:
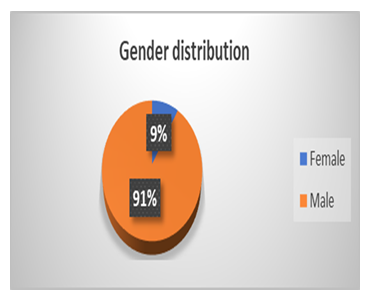
In our study, the mean age of the patients was 25 ± 7.749 years, ranging from 21 to 48 years. A significant proportion, 46.9% (15 cases), were ≤30 years old, 31.3% (10 cases) were aged 31-40 years, and 21.9% (7 cases) were ≥41 years. The sex distribution was predominantly male, constituting 90.6% (29 cases), while females accounted for 9.4% (3 cases). Similar to our study, Jingwei et al. evaluated the clinical outcomes of using suture anchors for acromioclavicular joint dislocation. They reported a mean participant age of 27.7 years (range: 19-55 years), with a predominance of male participants (24 males) compared to female patients (4 females) [15]. In their prospective study,Fauci et al. [11] reported a mean patient age of 35 ± 3.2 years, with a predominance of male patients (male-to-female ratio of 25 to 15). The analytical cross-sectional study conducted by Mardani-Kivi et al.reported that the participants' mean age was 32.6 ± 11.8 years, predominantly male participants (35 males and 4 females). Our study's predominantly male cohort (90.6%) with a mean age of 25 ± 7.749 years aligns with similar findings from Jingwei et al., Fauci et al., and Mardani-Kivi et al., all of whom reported male predominance and comparable age ranges.
Among those 30 years or younger, 43.8% received biological grafts, while 50.0% received Fiber Wire. In the 31- to 40-year age group, 37.5% received biological grafts and 25.0% received Fiber Wire. For individuals over 41 years, 18.8% received biological grafts and 25.0% received fiber wire (p=0.737). Among females, 6.3% received biological grafts, while 12.5% received fiber wire. Among males, 93.8% received biological grafts, and 87.5% received fiber wire (p=0.544).
4.2 Occupation & Addiction:
The patients were 9.4% (3 cases) drivers, 28.1% (9 cases) were farmers, 6.3% (2 cases) were housewives, 37.5% (12 cases) were laborers, 6.3% (2 cases) had private jobs, and 12.5% (4 cases) were students. With respect to addiction, in our study, out of the 32 participants, most of the patients were primarily addicted to alcohol and smoking, accounting for 34.4% (11 cases) and 31.3% (10 cases) of the participants, respectively. Additionally, 15.6% (5 cases) had no addiction, while 18.8% (6 cases) were found to be chewing tobacco.
4.3 Side affected & Mode of trauma:
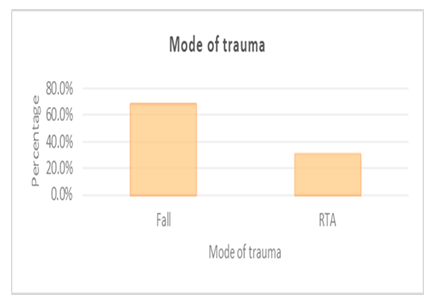
Regarding the affected side, 62.5% (20 cases) were on the right side, while 37.5% (12 cases) were on the left side. The data regarding the mode of trauma among the 32 cases shows that 68.8% (22 cases) were caused by falls, while 31.3% (10 cases) were due to road traffic accidents (RTA).
4.4 Grade of Dislocation:
The grade of dislocationdata shows that Grade 4 and Grade 5 dislocations are the most common, each accounting for 34.4% of the cases. Grade 3 dislocations account for 12.5%, and Grade 6 dislocations make up 18.8% (p-value = 0.98).
4.5 Complications:
90.6% of the cases had no complications; among those with no complications, 87.5% received biological grafts and 93.8% received fiber wire. Subluxation occurred in 6.3% of cases in both groups. Superficial infection was reported in 6.3% of cases in the biological graft group and zero in the FiberWire group. p-value = 0.446 indicates no statistically significant difference in the distribution of complications between the two treatment groups.
4.6 Duration of Surgery:
For the biological graft group, the mean duration of surgery is 91.8 mins ± 19.2 mins. For the Fibre Wire group, the mean duration is 78 mins ±4.8 mins (p-value = 0.007). Indicating the mean duration of surgery is significantly longer for the biological graft group compared to the FiberWire group. Jingwei et al. performed the suture anchor technique to treat AC joint dislocations and reported that the mean duration of surgery was 78 min ± 16.74.
4.7 Duration of Hospital Stay:
For the biological graft group, the mean duration of hospital stay is 6.38 days±3.50 days. For the Fiber Wire group, the mean duration of hospital stay is 5.69 days ± 2.94 days (p-value = 0.552), indicating no statistically significant difference in the mean duration of hospital stay between the two treatment groups.
4.8 Pre-& post-operative CMS scores:
Preoperatively, the biological graft group had the mean pre-op CMS as 35.56 ± 5.416, and the Fiber Wire group had the mean pre-op CMS as 36.13 ± 5.402 (p-value = 0.771 NS). Post-operatively, the mean CMS at 6 weeks for biological graft was noted as 63.00 ± 4.412. For the Fiber Wire group, the mean post-op CMS at 6 weeks was 62.25 ± 3.661 (p-value = 0.605 NS). The mean CMS at 6 months for biological graft was 91.06 ± 6.787. For the Fiber Wire group, the mean CMS at 6 months is 85.94 ± 6.971 (p-value = 0.044). The mean CMS at 12 months for biological graft was 95.25 ± 2.543. For the Fiber Wire group, the mean CMS at 12 months is 92.50 ± 2.221 (p-value = 0.003). Jingwei et al. reported the average CMS score as 96.3 ± 1.73, and out of a total of 26 patients, 8 patients showed full scores. Similarly, Mardani-Kivi et al. reported that the mean Constant score at 12 months was 91±1 in the Ethibond suture group and 92±1 in the semitendinosus autograft group (p>0.05).
5. Conclusion
This study compares the efficacy of biological graft versus fiber wire in the treatment of acromioclavicular (AC) joint dislocation. Our findings indicate that while both treatment options are effective across different age groups, genders, and occupations, the biological graft group demonstrated a significantly longer mean duration of surgery but better long-term functional outcomes, as evidenced by higher postoperative CMS scores at six and twelve months. Despite the longer surgical time, the biological graft group showed betterresults in terms of shoulder function.
Additionally, the study highlighted that most patients in both treatment groups experienced no complications, with a minimal incidence of subluxation and superficial infections. The comparison of hospital stay duration between the two groups revealed no significant difference, further supporting the overall comparability of the two treatments in terms of patient recovery. Overall, while both biological graft and fiber wire are viable options for AC joint dislocation, the biological graft may offer enhanced long-term functional outcomes, making it a preferable choice.
References
- Liu T, Bao FL, Jiang T, et al. Acromioclavicular Joint Separation: Repair Through Suture Anchors for Coracoclavicular Ligament and Nonabsorbable Suture Fixation for Acromioclavicular Joint. Orthop Surg 12 (2020): 1362-71.
- Wong M, Kiel J. Anatomy, Shoulder and Upper Limb, Acromioclavicular Joint. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2025).
- Hu F, Han S, Liu F, et al. A modified single-endobutton technique combined with a nice knot for treatment of Rockwood type III or V acromioclavicular joint dislocation. BMC Musculoskelet Disord 23 (2022): 15.
- Constant CR, Gerber C, Emery RJH, et al. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg 17 (2008): 355-61.
- Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med 27 (2008): 763-88.
- Wu W, Yuan X. The Graphic Derivation Process of Lagrange Multiplier Method. Open J Soc Sci 11 (2023): 527-32.
- Bosworth BM. Acromioclavicular Dislocation: End-Results of Screw Suspension Treatment. Ann Surg 127 (1948): 98-111.
- Neviaser JS. Acromioclavicular dislocation treated by transference of the coracoacromial ligament. AMA Arch Surg 64 (1952): 292-7.
- Bakalim G, Wilppula E. Surgical or conservative treatment of total dislocation of the acromioclavicular joint. Acta Chir Scand 141 (1975): 43-7.
- Katznelson A, Nerubay J, Oliver S, et al. Dynamic repair of acromioclavicular dislocation. Acta Orthop Scand 46 (1975): 199-204.
- Fauci F, Merolla G, Paladini P, et al. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs. synthetic ligament: a prospective randomized comparative study. J Orthop Traumatol Off J Ital Soc Orthop Traumatol 14 (2013): 283-90.
- Dalos D, Huber G, Wichern Y, et al. Acromioclavicular joint suture button repair leads to coracoclavicular tunnel widening. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 31 (2023): 161-8.
- Meeder PJ, Wentzensen A, Weise K. Surgical repair of complete acromioclavicular separation (Tossy III) by tension wire bending and suture of the ligaments (author’s transl.). Langenbecks Arch Chir 350 (1980): 169-73.
- Constant–Murley Score: systematic review and standardized evaluation in different shoulder pathologies—PMC [Internet] (2025).
- Zhang JW, Li M, He XF, et al. Operative treatment of acromioclavicular joint dislocation: a new technique with suture anchors. Chin J Traumatol Zhonghua Chuang Shang Za Zhi 17 (2014): 187-92.














 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 