Hip Resurfacing Arthroplasty Failure. Conversion to Total Hip is it a Favorable Solution with Satisfactory Outcomes?
Abdel-Hamid A Atallah1, Yaser El-Sayed Hassan Wahd1, Mohamed A Abdel-AAl2*
1Assistant Professor orthopaedic surgery, Faculty of medicine for girls, Al-Azhar University, Cairo, Egypt
2Consultant orthopedic surgeon – El bakey General Hospital, Ministry of Health, Cairo, Egypt
*Corresponding Author: Mohamed A Abdel-AAl, Consultant orthopedic surgeon – El bakey General Hospital, Ministry of Health, Cairo, Egypt
Received: 27 February 2022; Accepted: 03 March 2022; Published: 21 March 2022
Article Information
Citation: Abdel-Hamid A Atallah, Yaser El-Sayed Hassan Wahd, Mohamed A Abdel-AAl. Hip Resurfacing Arthroplasty Failure. Conversion to Total Hip is it a Favorable Solution with Satisfactory Outcomes? Journal of Orthopedics and Sports Medicine 4 (2022): 162-177.
View / Download Pdf Share at FacebookAbstract
Background: Hip resurfacing arthroplasty (HRA) had been utilized since the 1950s. The concept favoured for selected young active patients with degenerative hip disease owing to its proposed advantages. Revision rate in most national registries nearly 3.5%. Conversion to total hip replacement may be the correct option for old patients and those whose activity levels changed and the need for hip resurfacing no longer required.
Purpose: The aim of this study is to assess the mid-term outcomes of converting failed hip resurfacing arthroplasty to total hip arthroplasty.
Study design: Prospective case series study.
Level of evidence: Therapeutic IV.
Patients and methods: The study enrolled thirty–five patients (twenty- five males) with failed hip resurfacing arthroplasty converted to total hip arthroplasty Mean age 52.3 years and mean time to revision 35.2 months. Revision included: femoral neck fractures (14 cases), femoral neck thinning (4 cases), component loosening (6 cases) component dislocation (3cases) persistent groin pain and clicking (3 cases) and wear of components (5 cases). Both components revised in Twenty-five patients while the remaining ten underwent revision of femoral component only.
Results: Mean Preoperative hip scores (Oxford, WOMAC, Harris and UCLA hip scores) were 19.4, 78.3, 33,8 and 4.1 respectively improved at last follow-up to 39.8, 11.1, 92.3 and 8.1 respectively representing statistically significant improvements over pre-operative scores (p < 0.0001 for each score) No cases of neurological, vascular, deep infection or implant failure. There were 3 cases (8.6%) with complications included surgical site infection with serous drainage for more than seven days (one case), heterotopic ossification (one case) and residual groin pain in one case. All patient
Keywords
<p>Hip resurfacing arthroplasty; Total hip arthroplasty; Femoral neck fractures; Component loosening</p>
Article Details
Abbreviations
WOMAC: Western Ontario Macmaster; UCLA: University of California at Los Anglos; THA: Total hip Arthroplasty; HRA: Hip resurfacing arthroplasty
1. Introduction
Hip resurfacing arthroplasty has attained great popularity over the last decade as an alternative to conventional, stemmed total hip arthroplasty (THA) particularly in young patients [1]. The proposed advantages of that concept over total hip arthroplasty include proximal femoral bone preservation, physiologic loading of the proximal femur and thus less stress shielding, avoidance of potential embolization risk due to lack of femoral reaming or cementation, decreased thigh pain associated with the femoral stem in conventional THA, [2-4] and improved proprioception of the hip joint with the ability of the patient to resume higher demand activities [5, 6]. In addition; if conversion to total hip necessary; it would be relatively straightforward and less technically demanding. The previous advantages in addition to good clinical results of surface arthroplasty have led to an increasing number of joint replacements in younger active patients [7, 8]. However; this age group faces an increased risk of early implant failure owing to their high activity level [3, 9]. With the increasing number of primary THA procedures being performed and the decreasing age of patients undergoing the procedure, there is an inevitable associated increase in revision burden for arthroplasty surgeons. While early results of hip resurfacing have been promising, a group of complications have been reported which require revision.
These include femoral neck fractures [10, 11] and recurrent pain and effusions thought to be related to an aseptic lymphocytic vasculitis associated lesion syndrome [12]. Large destructive lesions (pseudo tumours) have also been reported which lead to soft tissue loss around the hip joint [13].
2. Patients and Methods
The study initiated after receiving approval from the institutional ethics committee for research in accordance with the ethical standards laid down in the 1964 declaration of Helsinki and its later amendments. Also, a written consent had been obtained from the patient for participating in the study.
Between May 2016 and December 2020, Thirty–five patients (Twenty-five males) had been enrolled in this study. Mean age 52.3 years (average 40-67 years).
|
Age |
Males |
Females |
Total |
|
36-45years |
14 |
3 |
17 |
|
46-55years |
5 |
2 |
7 |
|
Above 56years |
6 |
5 |
11 |
|
Total |
25 |
10 |
35 |
Table 1: Age distribution of patients.
Distribution of age shown Table (1) average time to revision was 35.2 months (11-58 months). Indications for revision involved: femoral neck fractures 14 cases (40%) Figure (1), femoral neck thinning 4cases (11.4%), component loosening 6 cases (17.1%) Figure (2), component dislocation 3 cases (8.6%) persistent pain and clicking 3 cases (8.6%) and sever wear of the components of resurfacing prosthesis 5 cases (14.3%). In all cases laboratory investigations had been done to exclude infection. Demographic distribution of patients Table (2).
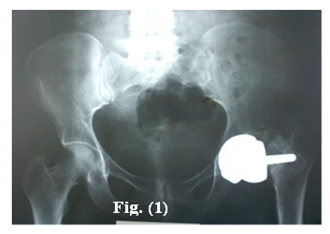
Figure 1: X-ray pelvis: Post-traumatic per prosthetic femoral neck fracture.

Figure 2: Metallosis of the per prosthetic soft tissue observed in three cases and proper debridement had been done.
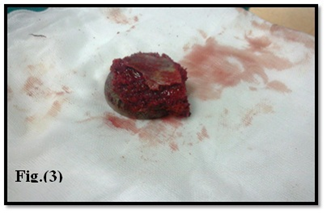
Figure 3: Removal of acetabular component.

Figure 4: Post-operative x-ray showing conversion of surface replacement arthroplasty to total hip arthroplasty with isolated revision of femoral component.
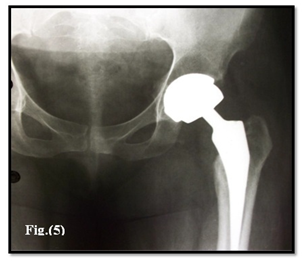
Figure 5: One year postoperative showing stability of the components, no signs of loosening.
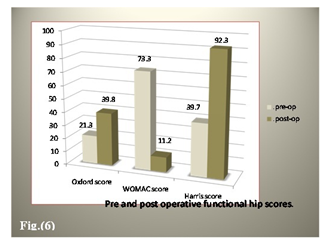
Figure 6: Functional outcome at last follow-up.
|
Males |
Females |
|
|
Number |
25 |
10 |
|
Mean Age |
51 Years |
47.7years |
|
Time to revision |
34.5 months |
26.4 months |
|
Femoral Neck fractures |
9 |
5 |
|
Femoral neck thinning |
2 |
2 |
|
Component loosening |
4 |
2 |
|
Component dislocation |
2 |
1 |
|
Groin pain |
2 |
1 |
|
Component wear |
4 |
1 |
|
Both component revision |
19 |
6 |
|
Femoral component revision |
6 |
4 |
Table 2: Demographic distribution of patients.
Radiographic evaluation through plain imaging Studies included standard anteroposterior and lateral x-rays of the pelvis and affected hip respectively. Computed tomography (CT) scans was obtained to assess proposed component size, bone quality and possible acetabular defects confirming their 3-dimensional extent and actual size. Twenty-five patients (71.4%) had revision of both components while the remaining ten patients (28.6%) underwent revision of the femoral component only Table 3.
|
Revised Component |
FNF |
FN thinning |
loosening |
Dislocation |
pain |
wear |
Total |
|
Both components |
10 |
2 |
4 |
2 |
3 |
4 |
25 |
|
Femoral component |
4 |
2 |
2 |
1 |
- |
1 |
10 |
|
Total |
14 |
4 |
6 |
3 |
3 |
5 |
35 |
FN=Femoral neck; FNF= Femoral neck fracture
Table 3: Distribution of revised component relative to revision indication.
Templating was done for all cases to detect near size of implanted component, detecting any bone defect and possibilities of bone grafting. For patients who had revision of both components, acetabular cup 2-4 mm larger than the extracted one was utilized and coupling metal on ultra-high molecular weight polyethylene used in nineteen cases while ceramic on ceramic couple used in six cases. For cases of femoral component revision a matching modular large cobalt chrome metal head was fixed to an uncemented stem. Average femoral component size used for females was 43 (38-50) compared to 49 (46-54) in the male patients. In cases where both components were revised, the average size of the explanted acetabular component was 50.7 mm (46 - 58 mm) compared to 54.6 mm (52-60) post revision.
Low molecular weight heparin (Enoxaparine) given twelve hours before surgery in a dose of 40 mg S C and started again 12 hours postoperative and then given daily until the patient was discharged from the hospital and continued for 35 days. Pre-operative I.V antibiotic (1gm 3rd generation cephalosporin) was administered to all patients. Preparation of two units of whole fresh blood to be ready for use according to intra-operative blood loss and preoperative patient haemoglobin level.
3. Surgical Procedure
All cases were operated upon by single surgeon. Operative technique was tailored case by case. Epidural anaesthesia used in 20 cases, spinal anaesthesia in 9 patients and general anaesthesia utilized in 6 patients. Posterior approach utilized in 20 cases, posterolateral approach used in five cases while modified Harding approach used in 10 cases. After skin incision; culture swabs of components, surrounding soft tissue and samples of any effusions were taken for microbiological examination. Massive metallosis of the periprosthetic soft tissue observed in five cases and proper debridement had been done Figure (3). Intraoperatively, small amount of effusion observed in 3 cases which was blackish in colour while in another 4 cases black staining of the pseudo capsule and periarticular soft tissues suggesting deposition of metallosis.
The mean operative time of the patients was 55.4± 6.0 minutes. Mean blood loss was 400 ±10.6 ml.
In cases where both components were revised the femoral neck osteotomy was performed (after dislocation of the joint) directly below the femoral head component and the healthy bone from the femoral head and neck was used as an autograft for the acetabular or femoral reconstruction. The acetabular component was removed by use of a fulcrum consisting of trial acetabular liner and curved osteotomies or cob elevator to allow relatively easy removal of the shell with minimal bone destruction. Any bone defect was dealt with either morsellised autograft or femoral head allograft. Femoral canal preparation done as for primary hip arthroplasty. Once the stem was firmly seated, a large diameter cobalt chrome head with a modular neck applied and reduction performed. Suction drain inserted deep to fascia lata followed by proper closure of the wound Figure (4).
Table 4: Distribution of functional outcome according to indications.
4. Postoperative Care
Parentral antibiotic administered (1 gram 3rd generation cephalosporin) and continued for 3 days. Patients revised without bone grafting were encouraged to move by 2nd day postoperative. Patient was trained to bear as much weight as he can with the aid of a walker for 3 weeks then using a cane for another 3 weeks then full weight bearing without any aid. Those revised with bone grafting encouraged for partial weight bearing for the first six weeks. First dressing done after 48-72 hours according to the amount of blood drained. Average hospital stay was 5 days (4-10 days).
5. Follow –Up Regimen
Patients were followed up clinically and radiologically at 3 weeks for 3 months and every 3 months for one year and periodically every 2 years with average duration of follow-up 26.8 months (28-48 months). Clinical follow-up through was assessed through recording Oxford, Harris, WOMAC and UCLA activity hip scores. Radiological assessment done to determine the over-all alignment of the limb, the respective size, fit and positions of the prosthetic components relative to the bone, the presence of radiolucent lines in zones adjacent to the components, lytic lesions or spot welds at the bone prosthesis interface as well as trabeculae extending to the uncemented stem Figure 5.
FNF=femoral neck fracture
FN=Femoral neck
Table 5: Functional outcome relative to indication of revision and revised component.
6. Results
Thirty-five patients who underwent conversion of failed hip resurfacing arthroplasty to a total hip arthroplasty were included in this prospective case series study. There were 25 males and 10 females. The mean age of the males and females were 56.3 years (range 40-67 years) and 48.8 years (range 41 - 65 years) respectively. The average duration of follow up was 12.7 months (3-31). Evaluation Parameters included Oxford, Harris and Western Ontario McMaster (WOMAC), UCLA activity hip scores, relief of pain, return to previous activities and patient satisfaction.
At last follow-up Oxford, WOMAC, Harris and UCLA hip scores improved from 19.4, 78.3, 33.8 and 4.1 preoperatively to 39.8, 11.1, 92.3, and 8.1 postoperatively p < 0.0001, p < 0.0001 and p < 0.0001 respectively. Figure (6) the greatest improvement was seen in the pain component of the Harris Hip Score with an average improvement of 35 units (79.5%) at the time of last follow up. No cases of neurological, vascular or deep infection occurred. Distribution of outcome according to the indication of revision illustrated in Table 4.
7. Complications
There were 3 complicated cases (8.6%) one case with surgical site infection with serous drainage for more than seven days treated by oral antibiotics and daily sterile dressings until the wound closed completely. Another case had residual groin pain, and the third case had mild heterotopic ossification. The later treated by Indomethacin 25 mg oral capsules three times daily (total 75 mg) continued for 4 weeks. All patients were satisfied with their outcome at their last follow up. The rest of patients have reported resolution of their pain post revision. Also a physiotherapy program was encouraged to improve hip range of motion for all patients.
8. Discussion and Review of Literatures
Revision rates of hip resurfacing arthroplasty (HRA) have been reported to be higher than primary total hip arthroplasty (THA) and in most national registries accounts to be 3.5% over 15 years [5]. As it is feasible to perform revision surgery after failed hip resurfacing arthroplasty, it is important to comprehend the reasons and results of revision. Revision of HRA is associated with a major risk of 5- year re-revision of 11%, which is much higher than 2.8% revision risk of a primary THA [7, 14]. It seems logic as HRA mostly indicated in younger age group who are characterized by higher level of both daily and sport activities. This is in addition to the specific design of the prosthesis. In our study we aim at restoring the daily and sport activities of the patients for which they underwent their HRA surgery. The most common indications for revision are femoral neck fracture (incidence range 0.9-1.1%) owing to osteoporosis or notching of the femoral neck during surgery [5, 3], component loosening, infection and metallosis with adverse local soft tissue reaction [15].
Other risk factors that may propose to HRA failure and the need for revision include: age, Gender and implant factors. Increased age accompanied by poor bone quality which subject the patient to complications as femoral neck fractures, osteoporosis of femoral neck and aseptic loosening. Many studies emphasized that patients above 55 years had increased risk of complications [4, 16, 17]. Female gender is a risk factor for implant failure, with revision rates in females significantly higher compared to males. Many studies have shown that survival rate of HRA may reach 95 to 98 % at 10 years in male patients [18, 19]. The previous study's factors are compatible with our study with some deviation owing to the small number of the series. Implant factors that exaggerate risk Challenges of revision include malposition which is associated with increased incidence of aseptic loosening and increased metal ion release. This is due to increased edge loading of the prosthesis and loss of fluid film lubrication [20, 21]. Also; many studies have emphasized that decreased femoral component size is associated with increased release of metal ions with subsequent increased incidence of failure for every 4 mm decrease in femoral component diameter [22, 23].
Component loosening in our study involved 6 patients (11.4%). In 4 cases both components were loose and revised while in two case only the femoral component affected and isolated femoral revision with retention of the acetabular shell has been done. The technique is less time consuming less technically demanding, minimizes risk of dislocation owing to use of large diameter femoral head and maintenance of residual acetabular bone stock [23, 6]. The only drawback of this procedure concerned with conflicts about the use of metal on metal bearing surface total hip arthroplasty and corrosion-related complications. Recent studies utilized femoral component with dual mobility femoral head though the Food and Drug Administration (FDA) has not approved the use of that [24, 25].
Sandiford NA et al [26], declared that complete revision of both acetabular and femoral components to a THA would minimize the potential sources of cobalt and chromium ions and consequently could produce good short-term clinical outcomes. In the setting of metallosis which explored intraoperatively in 3 cases, proper understanding of the characteristics and anatomic relationships is essential as this soft tissue contamination can distort normal surgical landmarks. Thorough debridement of metal debris and inflammatory soft tissue was performed. Any cystic or lytic osseous lesions were packed with bone graft. Extensive osteolysis may require the use of bone grafting along with supplemental fixation. Patients with these presentations had been revised by ceramic on ceramic bearing couple with functional outcomes similar to those of Willert et al [27].
Advantages of conversion of hip resurfacing to THA include avoidance of implant mismatch awareness, elimination of cobalt or chromium ions source if titanium-alloy femoral and acetabular components or ceramic femoral heads are utilized [13, 17]. However; some shortcomings may limit the prevalence of this strategy namely minimizing bone stock owing to bone loss on removal of hip resurface implants and concern of stability due to use of smaller femoral head in THA compared with that of hip resurfacing implants [28, 8]. The targets to be achieved in this study are relief of pain and returning back of patient daily and sport activities. In last follow-up all patients (except one) returned back to their daily activities and sports. One patient has moderate reduction in range of motion owing to hetertropic ossification. Clinical outcomes of conversion of HRA to total hip arthroplasty had been assessed via some studies. Su et al., [19] declared that clinical outcomes of this conversion was related to the indication of revision and the highest postoperative outcome observed in patients who underwent conversion for femoral neck fracture or implant loosening. The worst outcomes were seen in patients who underwent revision for unexplained pain or metal sensitivity.
In our study the average highest outcome according to Oxford, Harris, WOMAC and UCLA activity hip scores observed in patients revised for femoral neck fractures with values at last visit of 39.5, 98, 8, 7.4 and 9.3 respectively. The worst outcome observed in cases revised for unexplained pain with values of 38. 38.6, 4, 12.3 and 4 respectively. Our study outcome is comparable with many studies as Su et al, [10]. Revision of a single component of HRA, with retention of the remaining components, has been associated with mixed clinical results. In a study comparing 21 patients undergoing conversion of HRA to THA to patients undergoing primary THA, found that in the 18 patients who underwent femoral-sided revision only there was no clinical difference at a mean 46-month follow-up with regard to the mean Harris hip score; WOMAC and UCLA activity score [14]. The results could not be compared with those of our study as we have no comparative cohorts of primary THA (a limitation in our study).
Many studies emphasized that on revising resurfacing hip arthroplasty due to causes related to femoral component, the decision to change the femoral component only or both femoral and acetabular depends largely on the orientation of the acetabular component [2, 22]. In our study we follow similar strategy that if the lateral acetabular opening angle was greater than sixty degrees, we changed both acetabular and femoral components because some vertical orientation of the cup may be compatible with femoral component in resurfacing arthroplasty but this position is difficult to be compatible with fixed angle of the stemmed metal on metal THA prosthesis and lateral sub laxation mostly occur [29]. On the other hand; cases with lateral acetabular opening angle of resurfacing prosthesis near forty degree so during revision the fixed angle of the stemmed metal femoral component usually becomes compatible with the previous metal acetabular cup so in these cases we revised only femoral component. Revision of both acetabular and femoral components of HRA to THA has varying clinical outcomes reported across multiple studies [27]. A registry study of 882 HRA revision emphasized that no difference in re-revision rates and clinical outcome between the acetabular-sided, femoral-sided, or combined acetabular and femoral-sided cohorts [8, 9]. This finding correlated with the results of the prior study by Su et al, [11] Similar findings have been illustrated in our study (Table 5) with no marked differences in clinical outcome between both component revision and isolated femoral component revision regarding Oxford, Harris, WOMAC and UCLA activity hip scores. A small difference in outcome noticed in our study regarding the indication for revision with worst outcome in patients revised for component loosening, unexplained pain and component wear Table (5).
Sandiford, et al, [26] in a review of 25 patients undergoing conversion of surface arthroplasty to THA, found significant postoperative increases in Oxford, Harris, and WOMAC hip scores, with clinical results similar to revision THA. Reports on clinical outcomes following HRA revision for complications associated with metal wear are mixed, with some studies touting midterm clinical success rates as high as 97 %, while other data shows that revision for implant wear is associated with a significantly worse outcome when compared with revision for mechanical etiologies [29, 30]. These reports outcomes support our results regarding worse outcomes of revised cases for implant wear relative to those of femoral neck fractures (14 cases) or femoral neck thinning (4cases) Table (5).
9. Limitations of the Study
Our study presents some limitations, namely small number of patients, follow-up period is somewhat short relatively and lacking of comparative study. The technique itself has some limitations owing to the concerns of metal on metal coupling in hip arthroplasty. Furthermore systematic approach to revision of hip resurfacing arthroplasty to total hip arthroplasty is necessary to ensure optimal clinical results.
10. Conclusions
Our study supported by many literature reviews refer to preference of conversion of faile HRA to THA as it can avoid implant mismatch awareness, eliminate and minimize cobalt or chromium ion source if titanium alloy or ceramic components utilized. However decrease bone stock owing to bone loss on removal of resurface implants and concern of stability due to use of smaller femoral head break the progress of this Syllabus. Further systemic reviews work, randomized controlled studies and research of high level of evidence are needed to facilitate the progress of this technique.
11. Declarations
Ethical approval: This article does not contain any studies with animals.
Informed consent was obtained from all individual participants included in the study according to the rules of the hospital research ethical committee. All procedures performed in our study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Availability of Data and Materials
Not applicable.
Competing Interests
There are no conflicts of interest in the *manuscript, including financial, consultant, institutional and other relationships that might lead to bias or a conflict of interest. Authors had no disclose for any financial ties to the subject of this research
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author Contributions to the Study and Manuscript Preparation include the Following
Conception and design
Mohamed A. Abdel-aal
Acquisition of data analysis and interpretation of data
Abdel-hamid A.Atallah
Drafting the article
All authors.
Critically revising the article
Abdel-hamid A Atallah.
Reviewed submitted version of manuscript
All authors.
Surgical technique of the study
All authors.
Acknowledgements
We would appreciate as authors the whole stuff members of Al-zahraa university hospital Al-Azhar University and stuff members of El-Bakry General hospital Cairo-Egypt Ministry of Health.
References
- Amstutz HC, Le Duff MJ, Campbell PA, et al. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am 92 (2010): 2663-2671
- Anglin C, Masri BA, Tonetti J, et al. Hip resurfacing femoral neck fracture influenced by valgus placement. Clin Orthop Relat Res 465 (2007): 71-79.
- Buergi ML, Walter WL. Hip resurfacing arthroplasty: The Australian experience. J Arthroplasty 22 (2007): 61-65.
- Carrothers AD, Gilbert RE, Jaiswal A, et al. Birmingham hip resurfacing: the prevalence of failure. J Bone Joint Surg (Br) 92 (2010): 1344-1350.
- Australian orthopaedic association national joint replacement registry annual report. Adelaide: AOA (2009): 20-44.
- Mattie E, Matthew F Barra, Thomas G Myers. A Conversion Total Hip Arthroplasty Is Not a Primary Total Hip Arthroplasty. Tech. Orthop 29 (2019): 215.
- Barrack RL, Ruh EL, Berend ME, et al. Active patients perceive advantages after surface replacement compared to cementless total hip arthroplasty? Clin Orthop Relat Res 471 (2013): 3803-3813.
- Loughead JM, Starks I, Chesney D, et al. Removal of acetabular bone in resurfacing arthroplasty of the hip: a comparison with hybrid total hip arthroplasty. J Bone Joint Surg Br 88 (2006): 31-34.
- McKee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee-Farrar prosthesis. J Bone Joint Surg. (Br) 48 (1966): 245-259.
- Schmidutz F, Wanke-Jellinek L, Jansson V, et al. Revision of Hip Resurfacing Arthroplasty with a Bone-conserving Short-stem Implant. Reconstructive Review 3 (2013).
- Su EP, Su SL. Surface replacement conversion: results depend on reason for revision. J.Bone Joint 95 (2013): 88-91.
- Thomas P. Gross. Hip resurfacing: is female gender an absolute or relative contraindication? Ann Joint 6 (2021): 23
- Gaillard MD, Gross TP. Metal-on-metal hip resurfacing in patients younger than 50 years: a retrospective analysis: 1285 cases, 12-year survivorship. J Orthop Surg Res 12 (2017): 79.
- Blevins JL, Shen TS, Morgenstern R, et al. Conversion of Hip Resurfacing With Retention of Monoblock Acetabular Shell Using Dual-Mobility Components. J. Arthroplasty 34 (2019): 2037-2044.
- Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg (Br) 86 (2004): 177-184.
- De Haan R, Campbell PA, Su EP, et al. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br 90 (2008): 1158-1163.
- Gross TP, Liu F. Risk factor analysis for early femoral failure in metal-on-metal hip resurfacing arthroplasty: the effect of bone density and body mass index. J. Orthop. Surg Res 7 (2012): 10.
- Murray DW, Gundle R, Gill HS, et al. The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg. (Br) 94 (2012): 1180-1186.
- Prosser GH, Yates PJ, Wood DJ, et al. Outcome of primary resurfacing hip replacement: evaluation of risk factors for early revision. Acta Orthop 81 ((2010): 66-71.
- Jacob A, Haynes Jeffrey B, Stambough Robert L, et al. Conversion of a failed hip resurfacing arthroplasty to total hip arthroplasty: pearls and pitfalls. Curr Rev Musculoskelet Med 9 (2016): 103-111.
- Klein GR. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J Arthroplasty 22 (2007): 171-175.
- Langton DJ1, Jameson SS, Joyce TJ, et al. Poor outcome of revised resurfacing hip arthroplasty. Acta Orthop 81 (2010): 72-76.
- Langton DJ, Jameson SS, Joyce TJ, et al. The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg. (Br) 90 (2008):1143-1151.
- McMinn D, Daniel J. History and modern concepts in surface replacement. Proc Inst Mech Eng H 220 (2006): 239-251.
- Pritchett JW. One-component revision of failed hip resurfacing from adverse reaction to metal wear debris.J Arthroplasty 29 (2014): 219-224.
- Sandiford NA, Muirhead-Allwood SK, Skinner JA. Revision of failed hip resurfacing to total hip arthroplasty rapidly relieves pain and improves function in the early post-operative period. J Orthop Surg Res 5 (2010): 88.
- Wera GD, Robert J Gillespie, Carter Petty MA, et al. Revision of Hip Resurfacing Arthroplasty. Am J Orthop 39 (2010).
- Lavigne M Masse V, Girard J, Roy AG, et al. Return to sport after hip resurfacing or total hip arthroplasty: a randomized study. Rev Chir Orthop Reparatrice Appar Mot 94 (2008): 361-367.
- Vedat BI, Izzet B, Kasim K. Mid-Term Results of the Metal-on-Metal Total Hip Arthroplasty. Medical Journal of Islamic World Academy of Sciences 28 (2020): 49-54.
- Wong JM, Liu YL, Graves S, et al. What is the Re-revision Rate After Revising a Hip Resurfacing Arthroplasty? Analysis from the AOANJRR. Clin Orthop Relat Res 473 (2015): 3458-3464.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 