Long Term Follow-up of Lumbar Spine Annular Fissures
Faranak Rafiee1*, Shadi Asadollahi2*, Rodrigo Luna2*, Mina Motaghi3, Meisam Hoseinyazdi2, Gary Gong2, David M Yousem2
1Massachusetts General Hospital, Boston MA, USA
2Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins Medical Institution, Baltimore, MD, USA
3Brookdale University Hospital Medical Center, Brooklyn, NY, USA
*Corresponding Author: David M. Yousem, Professor, Neuroradiology Division, Department of Radiology, Associate Dean of Professional Development, Johns Hopkins University School of Medicine, Baltimore, MD 21287, USA.
Received: 06 May 2023; Accepted: 15 May 2023; Published: 18 May 2023
Article Information
Citation:
Faranak Rafiee, Shadi Asadollahi, Rodrigo Luna, Mina Motaghi, Meisam Hoseinyazdi, Gary Gong, David M Yousem. Long Term Follow-up of Lumbar Spine Annular Fissures. Journal of Orthopedics and Sports Medicine. 5 (2023): 241-248.
View / Download Pdf Share at FacebookAbstract
Background and Purpose: Annular fissures are common in the lumbar spine; their natural history is not well-known. They typically are bright on T2W and show linear enhancement. We hypothesized that Lumbar Annular Fissures (LAF) rarely resolve over time and their imaging features are static.
Materials and Methods: From 2011 to 2021, we evaluated patients who had more than one lumbar spine MR. We recorded LAF imaging features on T1W, T2W, and post-contrast sequences and the evolution of those findings over time. We also inspected the evolution of concomitant disc pathology. Finally, we reviewed the radiologic reports to see if LAFs were mentioned.
Results: Of the 441 included patients, 238 (54.0%) had a LAF. Of these, 123/238 (51.7%) had more than one LAF (total 436 LAFs). 433 (99.3%) LAFs were bright on T2W; 3 LAFs enhanced but were not bright on T2W. In follow up, (mean 621 days, SD 951 days), 145/436 (33.3%) LAFs changed in T2W signal intensity; 62.8% showed less hyperintensity on T2W, 7 resolved completely. Of 65 gadolinium-enhanced cases, 53 (81.5%) LAFs enhanced; that enhancement persisted in 85.4%. Bulges or herniations coexisted with LAFs in 388/436 (89.0%). With changes in signal intensity and gadolinium enhancement, the bulge/herniation often evolved. 15.8% of LAFs were reported.
Conclusion: LAFs are prevalent (54.0%) but are under-reported. The vast majority are bright on T2W but that hyperintensity may change over time. Most LAFs enhance and do so persistently. Disk bulges and herniations coexist in 89% of cases and evolve with the LAFs.
Clinical Relevance: The stability of T2 hyperintensity and gadolinium enhancement of LAFs over time implies that the age of the AF cannot be inferred unless it is newly appearing on a current study.
Keywords
Lumbar; Spine; Annular fissures; Disk, Degenerative
Spine articles Spine Research articles Spine review articles Spine PubMed articles Spine PubMed Central articles Spine 2023 articles Spine 2024 articles Spine Scopus articles Spine impact factor journals Spine Scopus journals Spine PubMed journals Spine medical journals Spine free journals Spine best journals Spine top journals Spine free medical journals Spine famous journals Spine Google Scholar indexed journals Lumbar annular fissure articles Lumbar annular fissure Research articles Lumbar annular fissure review articles Lumbar annular fissure PubMed articles Lumbar annular fissure PubMed Central articles Lumbar annular fissure 2023 articles Lumbar annular fissure 2024 articles Lumbar annular fissure Scopus articles Lumbar annular fissure impact factor journals Lumbar annular fissure Scopus journals Lumbar annular fissure PubMed journals Lumbar annular fissure medical journals Lumbar annular fissure free journals Lumbar annular fissure best journals Lumbar annular fissure top journals Lumbar annular fissure free medical journals Lumbar annular fissure famous journals Lumbar annular fissure Google Scholar indexed journals Spine radiology articles Spine radiology Research articles Spine radiology review articles Spine radiology PubMed articles Spine radiology PubMed Central articles Spine radiology 2023 articles Spine radiology 2024 articles Spine radiology Scopus articles Spine radiology impact factor journals Spine radiology Scopus journals Spine radiology PubMed journals Spine radiology medical journals Spine radiology free journals Spine radiology best journals Spine radiology top journals Spine radiology free medical journals Spine radiology famous journals Spine radiology Google Scholar indexed journals Disk fissures articles Disk fissures Research articles Disk fissures review articles Disk fissures PubMed articles Disk fissures PubMed Central articles Disk fissures 2023 articles Disk fissures 2024 articles Disk fissures Scopus articles Disk fissures impact factor journals Disk fissures Scopus journals Disk fissures PubMed journals Disk fissures medical journals Disk fissures free journals Disk fissures best journals Disk fissures top journals Disk fissures free medical journals Disk fissures famous journals Disk fissures Google Scholar indexed journals Surgery articles Surgery Research articles Surgery review articles Surgery PubMed articles Surgery PubMed Central articles Surgery 2023 articles Surgery 2024 articles Surgery Scopus articles Surgery impact factor journals Surgery Scopus journals Surgery PubMed journals Surgery medical journals Surgery free journals Surgery best journals Surgery top journals Surgery free medical journals Surgery famous journals Surgery Google Scholar indexed journals Fissured disk articles Fissured disk Research articles Fissured disk review articles Fissured disk PubMed articles Fissured disk PubMed Central articles Fissured disk 2023 articles Fissured disk 2024 articles Fissured disk Scopus articles Fissured disk impact factor journals Fissured disk Scopus journals Fissured disk PubMed journals Fissured disk medical journals Fissured disk free journals Fissured disk best journals Fissured disk top journals Fissured disk free medical journals Fissured disk famous journals Fissured disk Google Scholar indexed journals Disk bulge articles Disk bulge Research articles Disk bulge review articles Disk bulge PubMed articles Disk bulge PubMed Central articles Disk bulge 2023 articles Disk bulge 2024 articles Disk bulge Scopus articles Disk bulge impact factor journals Disk bulge Scopus journals Disk bulge PubMed journals Disk bulge medical journals Disk bulge free journals Disk bulge best journals Disk bulge top journals Disk bulge free medical journals Disk bulge famous journals Disk bulge Google Scholar indexed journals Herniation articles Herniation Research articles Herniation review articles Herniation PubMed articles Herniation PubMed Central articles Herniation 2023 articles Herniation 2024 articles Herniation Scopus articles Herniation impact factor journals Herniation Scopus journals Herniation PubMed journals Herniation medical journals Herniation free journals Herniation best journals Herniation top journals Herniation free medical journals Herniation famous journals Herniation Google Scholar indexed journals Gadolinium articles Gadolinium Research articles Gadolinium review articles Gadolinium PubMed articles Gadolinium PubMed Central articles Gadolinium 2023 articles Gadolinium 2024 articles Gadolinium Scopus articles Gadolinium impact factor journals Gadolinium Scopus journals Gadolinium PubMed journals Gadolinium medical journals Gadolinium free journals Gadolinium best journals Gadolinium top journals Gadolinium free medical journals Gadolinium famous journals Gadolinium Google Scholar indexed journals Painful disc stimulation articles Painful disc stimulation Research articles Painful disc stimulation review articles Painful disc stimulation PubMed articles Painful disc stimulation PubMed Central articles Painful disc stimulation 2023 articles Painful disc stimulation 2024 articles Painful disc stimulation Scopus articles Painful disc stimulation impact factor journals Painful disc stimulation Scopus journals Painful disc stimulation PubMed journals Painful disc stimulation medical journals Painful disc stimulation free journals Painful disc stimulation best journals Painful disc stimulation top journals Painful disc stimulation free medical journals Painful disc stimulation famous journals Painful disc stimulation Google Scholar indexed journals Spots articles Spots Research articles Spots review articles Spots PubMed articles Spots PubMed Central articles Spots 2023 articles Spots 2024 articles Spots Scopus articles Spots impact factor journals Spots Scopus journals Spots PubMed journals Spots medical journals Spots free journals Spots best journals Spots top journals Spots free medical journals Spots famous journals Spots Google Scholar indexed journals Transdiscal tear articles Transdiscal tear Research articles Transdiscal tear review articles Transdiscal tear PubMed articles Transdiscal tear PubMed Central articles Transdiscal tear 2023 articles Transdiscal tear 2024 articles Transdiscal tear Scopus articles Transdiscal tear impact factor journals Transdiscal tear Scopus journals Transdiscal tear PubMed journals Transdiscal tear medical journals Transdiscal tear free journals Transdiscal tear best journals Transdiscal tear top journals Transdiscal tear free medical journals Transdiscal tear famous journals Transdiscal tear Google Scholar indexed journals Rim lesions articles Rim lesions Research articles Rim lesions review articles Rim lesions PubMed articles Rim lesions PubMed Central articles Rim lesions 2023 articles Rim lesions 2024 articles Rim lesions Scopus articles Rim lesions impact factor journals Rim lesions Scopus journals Rim lesions PubMed journals Rim lesions medical journals Rim lesions free journals Rim lesions best journals Rim lesions top journals Rim lesions free medical journals Rim lesions famous journals Rim lesions Google Scholar indexed journals Perinuclear tear articles Perinuclear tear Research articles Perinuclear tear review articles Perinuclear tear PubMed articles Perinuclear tear PubMed Central articles Perinuclear tear 2023 articles Perinuclear tear 2024 articles Perinuclear tear Scopus articles Perinuclear tear impact factor journals Perinuclear tear Scopus journals Perinuclear tear PubMed journals Perinuclear tear medical journals Perinuclear tear free journals Perinuclear tear best journals Perinuclear tear top journals Perinuclear tear free medical journals Perinuclear tear famous journals Perinuclear tear Google Scholar indexed journals Radial tears articles Radial tears Research articles Radial tears review articles Radial tears PubMed articles Radial tears PubMed Central articles Radial tears 2023 articles Radial tears 2024 articles Radial tears Scopus articles Radial tears impact factor journals Radial tears Scopus journals Radial tears PubMed journals Radial tears medical journals Radial tears free journals Radial tears best journals Radial tears top journals Radial tears free medical journals Radial tears famous journals Radial tears Google Scholar indexed journals
Article Details
Abbreviations:
MR: Magnetic Resonance; LAF: Lumbar Annular Fissure; HNP: Herniated Nucleus Pulposus; NASS: North American Spine Society; ASSR: American Society of Spine Radiology; ASNR: American Society of Neuroradiology; HIZ: High-Intensity Zone; T2W: T2 Weighted Images; SD: Standard Deviation; IQR: Interquartile Range
1. Introduction
The nomenclature of lumbar spine degenerative disk disease has been codified in numerous publications including the “Lumbar disc nomenclature version 2.0 :Recommendations of the combined task forces of the North American Spine Society (NASS), the American Society of Spine Radiology (ASSR) and the American Society of Neuroradiology”(ASNR)” [1-3]. The consensus statement has allowed practitioners to use a common vocabulary when describing the degeneration of disks. One of the terms that is precisely defined is the Annular Fissure (AF). The combined task forces stated that “Annular fissures are separations between the annular fibers or separations of annular fibers from their attachments to the vertebral bone.” Regarding the use of the term “annular tear”, the NASS, ASSR and ASNR opined that…” use of the term ‘tear’ can be misunderstood because the analogy to other tears has a connotation of injury, which is inappropriate in this context. The term ‘fissure’ is the correct term.”
Although LAFs may be described as concentric, radial or transverse the implication is that they are early manifestations of degenerative disk disease. The natural history of LAFs was explored by Sharma et al. [4] in 2009. The authors used a 1-6 point grading scale of the signal intensity of the disk (Grade 1: normal bright signal intensity in the central portion, Grades 2–5 represented loss of signal intensity affecting <25%, 26%–50%, 51%–75%, and 76%–99% of the central aspect of the disks and Grade 6 complete absence of central bright signal intensity). They found that the degeneration grade for those disks with LAFs (mean 3.07) was significantly higher than disks without LAFs (mean 1.43). They also found that, over time, disks with LAFs showed a statistically significant worsening of their grade [4]. Interestingly, Sharma et al did not look at whether LAFs put the patient at higher risk for disk herniation. Nonetheless, the implication is that radiologists should include whether an AF is present or not in their spine MR reports.
Munter et al. [5] in 2002, performed a retrospective review of 29 LAFs of lumbar disks in 18 patients. Over a mean follow up period of 17.2 months (S.D. 12.3 months) the authors found no change in the high intensity zone (focally hyperintense on T2-weighted images) of the LAFs nor changes in the frequent enhancement of the disk fissures. One AF, followed for 64 months, did not change its signal intensity nor enhancement characteristics [5].
We sought to better assess the prevalence, longitudinal imaging characteristics, and significance of LAFs. We hypothesized that 1) LAFs are common, 2) they maintain their high intensity and enhancement ad infinitum, and 3) they do not impact the prevalence of bulges or herniations.
2. Methods
This retrospective study was approved by the Institutional Review Board and was HIPAA compliant. The study was restricted to review of images, reports of studies, and the demographics of the study population; the Electronic Medical Record (EMR) was not approved to be accessed to explore patient symptomatology.
We searched our PACS (Carestream Health, Inc, Rochester NY) data base of all radiologic studies that were obtained at our hospital from 2011 to 2021 in which a patient had more than one lumbar spine MR study. From Carestream we were able to review MRI reports and obtain demographic data without accessing the EMR.
We included only those that had not previously undergone surgery or those disks that had not been violated by neoplasm, infection, or any other inflammatory process.
Imaging was performed on several different 1.5-T and 3.0T MR systems. The imaging parameters varied slightly, depending on the manufacturer of the system. All studies included sagittal fast spin-echo T2-weighted MR imaging (2700-4000/98/3 [range of TR/TE/NEX]) and sagittal T1-weighted MR imaging (600/14/3). Both T1- and T2-weighted imaging had the following parameters: section thickness, 4.0 mm; section gap, 0.4 mm; field of view, 175 to 210 × 280 mm; and matrix, 220 × 512. Enhanced studies employed gadopentetate dimeglumine (0.1 mmol/kg), and contrast-enhanced T1-weighted MR images were obtained with the same parameters as those stated above for unenhanced T1-weighted MR images.
The presence or absence of annular tear(s) was recorded for each examination. The interval between examinations, the configuration of the tear, and the persistence or resolution of imaging findings were noted at each level. The coexistence of the fissured disk with a bulge or herniation was recorded initially and over time. The cases were reviewed by consensus among a neuroradiologist with 20-years’ experience and a musculoskeletal radiologist with 9-years’ experience (disagreements were resolved by a neuroradiologist with 32 years of full-time practice after 2 years of neuroradiology fellowship training).
2.1 Statistical analysis
Distribution of data was tested using Shapiro-Wilk test. Mean (SD) is reported for normally distributed data and median (IQR) for data that is not normally distributed. Pearson chi-square or Fisher exact test were used for comparing categorical variables between age groups or different lumbar levels. ANOVA test were used for assessing association between age and LAF level. Poisson regression analysis was performed for evaluation of the relationship between the number of LAFs with age and sex of the patients. Logistic regression analysis was used for investigating the relationship between change in signal intensity and change in bulge/herniation. All the statistical analysis was performed using STATA 16 (StataCorp.2019. Stata Statistical Software: release 16. College Station.TX: StataCorp LLC).
3. Results
441 patients’ studies were reviewed in this study based on inclusion criteria. Of those 220 (49.9%) patients were female. The median age (IQR) was 55.5 (40-69) years old. 238 (54.0%) patients were found to have AF and 436 lumbar spine levels had a LAF identified initially (Table 1). These 436 LAFs were the ones that were followed over time from the first scan. The LAFs were predominantly seen at L4-5 and L5-S1 but occurred at all levels (Table 1). Most (51.7%) patients had more than one LAF in the spine (Table 2). We found that only 69/436 (15.8%) of the LAFs were mentioned in the lumbosacral MR reports (Table 1).
|
Spinal Levels of LAFS |
Number of LAFS |
Percentage reported |
|
T12-L1 |
4 |
25 % |
|
L1-2 |
18 |
0 % |
|
L2-3 |
54 |
14.8 % |
|
L3-4 |
83 |
10.8 % |
|
L4-5 |
138 |
18.8 % |
|
L5-S1 |
139 |
18 % |
|
TOTAL LAFs |
436 |
15.8 % |
|
Most LAF (277/436 =63.5%) occurred at L4-5 and L5-S1. |
||
Table 1: Location of LAFs.
|
Number of Levels with an LAF |
Number of patients (Total 238) |
|
4 |
19 |
|
3 |
37 |
|
2 |
67 |
|
1 |
115 |
|
Total: 436 LAFs |
|
|
Most patients (123/238 =51.7%) had more than one LAF. |
|
Table 2: Frequency of Multiple LAFs.
3.1 LAF Frequency and Age
LAF frequency in different age groups by decades and different intervertebral disc levels were assessed. Levels L2-L3, L3-L4, L4-L5 had statistically significant correlation between LAF frequency and patients’ age with P-values of 0.04, <0.001, 0.002 respectively. At these levels, the older you were, the more likely you had an LAF.
3.2 Demographics:
The number of LAFs was not different between men and women. The level of the LAF had no association with either age or sex of the patient. However, the number of LAFs was 2.3% higher for each one-year increase in age (incident rate ratio (IRR)=1.023, p-value<0.001).
3.3 Initial appearance:
Of all, 433/436 (99.3%) LAF were bright on T2W (Figure 1); three were only seen on gadolinium enhanced images. There was no difference in lumbar level and incidence of high intensity on T2W. 65 LAFs were evaluated with a gadolinium enhanced study; 53/65 (81.5%) showed gadolinium enhancement. At initial evaluation 388/436 (89.0%) LAFs had a disk bulge or herniation associated with the LAF. The ratio of bulges to herniations in this group was 2:1 in favor of bulges.
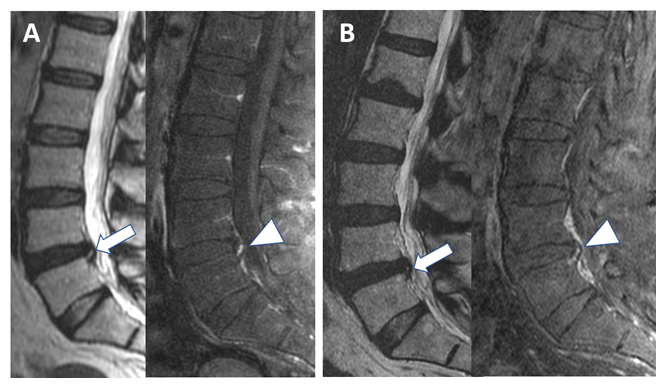
Figure 1: Hyperintensity on T2 and contrast enhancement of an annular fissure at initial and follow-up imaging. Initial (A) Sagittal T2-weighted MR image (left) and fat-suppressed gadolinium-enhanced T1W MR image (right) show abnormal focal hyperintensity on T2 (arrow) and focal contrast enhancement (arrowhead) in the posterior margin of the L4-L5 disc, indicating an annular fissure. (B) Images of the same patient shown in (A) obtained 2827 days later reveal decreased extension and hyperintensity of the focal abnormality on sagittal T2W scan (arrow) but similar contrast enhancement on T1W image (arrowhead) related to annular fissure.
3.4 Follow-up Appearance:
The range of follow-up duration was 5 days to 6270 days (mean 621 days, SD 951 days). Of 436 levels with an AF, 145 (33.3%) had a change in T2 signal but all remained hyperintense; 54 LAFs became brighter and 91 became darker and 7 (1.6%) resolved completely (Figure 2). The fissure enlarged in 66 (15.1%) LAFs, got smaller in 50 (11.5%), and showed no change in size in 320 (73.4%). 327 (84.3%) of the 388 LAFs with a disk bulge or herniation had no change in the bulge or herniation. However, in 80 LAFs either the bulge/herniation got smaller or resolved (50%) or got larger or appeared (50%). Gadolinium enhanced follow up scans were available for 48 LAFS; in 41/48 (85.4%) the enhancement persisted. In the 7 in which the enhancement resolved (Figure 3), 6/7 showed a decrease in T2W intensity concurrently (only 4 of the 41 with persistent enhancement also had a decrease in T2W hyperintensity). The difference between these 2 groups (with and without resolution of enhancement) for T2W reduction in intensity was statistically significant (p<0.001).
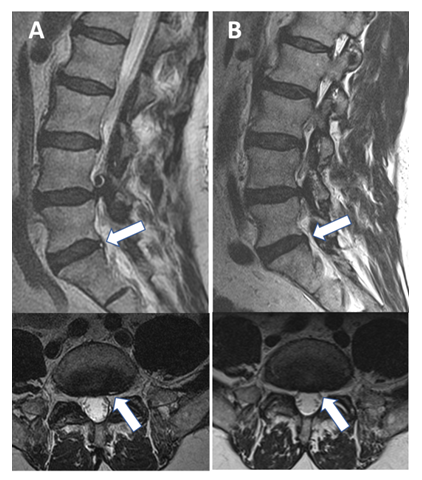
Figure 2: Hyperintensity on T2-weighted turbo spin echo sequence of annular fissure at initial and follow-up imaging. Initial (A) Sagittal and axial T2W (top and bottom) images showing annular fissure at the L5-S1 level to the left of midline (arrow) that appears hyperintense on T2W ; (B) Follow-up of the same patient 2492 days later reveals absent AF signal intensity on sagittal T2W images with no discernible high intensity zone on the axial scan (arrow).
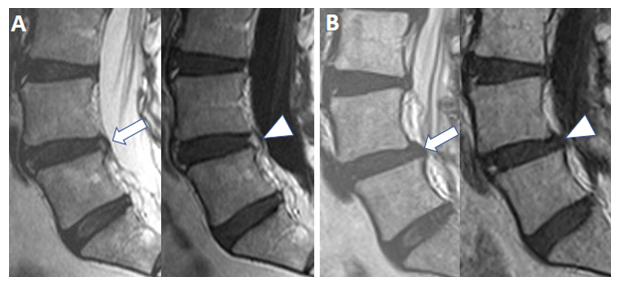
Figure 3: Interval complete resolution of hyperintensity on T2-weighted and enhancement by on gadolinium-enhanced T1W TSE MR image of an annular fissure on follow-up imaging. Initial (A) Sagittal T2W (left) and gadolinium-enhanced Sagittal T1W (right) images reveal T2W hyperintense annular fissure (arrow) with enhancement (arrowhead) at the L4-L5 level. (B) Follow-up imaging performed 2038 days later shows complete resolution of the hyperintensity on T2W (arrow) and enhancement on T1W TSE (arrowhead) of the previously seen annular fissure.
3.5 LAFs and Bulge/Herniation
For levels with LAF, a change in LAF signal intensity was significantly associated with a change in bulge/herniation in patients (p-value<0.001). Patients with LAF who had a change in signal intensity had 3.7 times higher risk of having change in bulge/herniation over time (p-value<0.001). If the LAF became darker, the risk of having a bulge change was 4.5 times higher than when there was no change in LAF (0.012), and the risk for change in bulge/herniation was 7.3 times higher in levels that had a decrease in LAF signal intensity (p-value<0.001). The risk of the bulge becoming smaller over time was 21.2 times more in levels that showed the LAF becoming darker in T2W signal intensity compared to levels with no change in signal intensity (p<0.001) and this risk was 7.7 times higher for levels when the T2W signal intensity became brighter compared to levels with no change (p = 0.032). The risk of the bulge becoming larger in time was 16.5 times higher in levels where the signal intensity became darker compared to levels with no change in signal intensity (p<0.001) and this risk was 15.3 times higher for levels where the signal intensity of the LAF became brighter on T2W images. (p<0.001)
4. Discussion
April and Bogduk [6] first defined the high-intensity zone (HIZ) in the spinal discs as one of the features they believed correlated with painful disc stimulation. They described HIZs as spots of intensely high signal in posterior annulus depicted on T2-weighted images [6,7]. Years later, in their histological study Peng et al. [8], demonstrated that the HIZ is an area of vascularized granulation tissue growing into the posterior disc “tear”. Subsequently, NASS, ASSR, and ASNR recommended referring to these lesions as LAFs rather than tears, since the term “tear” can be falsely misconstrued as arising secondary to trauma or acute injury.
Postmortem studies have classified LAFs into three types: radial, transverse, and concentric [8]. According to the definition of the AF, the orientation of the separation between annular fibers determines the type of the tear. When the rent in annular fibers extends from the nucleus peripherally, the resultant tear is considered as radial. The delamination parallel to the peripheral disc contour results in a concentric fissure. Finally, the transverse fissure is defined as a horizontally oriented radial fissure [1]. In all types of LAFs, mucoid/fluid material or vascularized granulation tissue filling the tear results in the high signal intensity in T2-weighted and the enhancement in post-contrast T1-weighted images [8-10].
The latest post-mortem study by Vernon-Roberts et al. [11] introduced three further classes of “tear” in addition to the previously mentioned types: Perinuclear Tear (PNT), Transdiscal Tear (TDT) and Rim Lesions (RL). Radial tears are frequently the axial arm extension of the PNTs. The authors implied that the concentric tears are the first tears to emerge and can exist as early as age 15. Conversely, the TDTs are rare before age of 50 and are associated with excessive mobility at the level of the involved disc, evidenced by frequent coexistence of same-level marginal osteophytes. RLs are described as peripheral horizontal tears in close contact with the adjacent vertebral endplates. The progressive increase in RL incidence with age tends to be the result of the increase in the number of the involved discs along with the number of RLs present in each disc [11,12].
Multiple modalities have been applied for the depiction of intervertebral disc disease. Discography has shown superiority in detection of the annular tears associated with low back pain [13,14]. Although an invasive procedure, CT discography is deemed the reference standard for meticulous imaging of the LAFs and correlation with symptoms [15]. Kakitsubata et al. [16] compared the conventional MRI with MR discography in cadavers and came to the conclusion that MR discography is more sensitive in detecting the clinically significant radial tears. Although a normal MRI does not exclude annulus pathology, this modality is the mainstay of intervertebral disc imaging [17]. In an interesting recent study, Torén et al. [15] investigated the intervertebral disc behavior on conventional MR images before and after applying spinal loading and compared the results to the subsequent discography. The spinal loading induced different regional T2 signal alterations depending on the fissure width and whether it extends to the outer annulus or not. Furthermore, spinal loading resulted in decreased T2 signal intensity in patients with pain-negative discograms, while no signal change was detected in the group with pain-positive discograms. Such loading behavior of the intervertebral discs promises future MRI progress in correlating LAFs with clinical symptoms in a non-invasive manner.
Most LAFs are asymptomatic and discovered incidentally [18]. They have been frequently reported in the asymptomatic population and cadavers [19,20]. In a systematic review, Brinjikji et al. [21] showed that many image-based spinal degenerative changes are part of normal aging process and are not associated with pain. Furthermore, there is no conclusive evidence that the treatment of asymptomatic LAFs provides benefits [18]. Yet increasing our knowledge about the natural course of these lesions helps in choosing the right approach to both symptomatic and asymptomatic LAFs.
Our study is the largest number of LAFs (n = 436) followed for the longest duration (mean 621 days). We noted that 99.3% of LAFs were bright on T2W; only 3 showed enhancement without a HIZ on T2W. At the same time 41/48 LAFs enhanced. The literature has debated whether T2W or post-contrast T1W scans were best for identifying LAFs. Our study suggests the T2W scans are superior and this is useful since relatively few disks are ever evaluated with gadolinium enhanced sequences [only 48/436 (11%) were evaluated by contrast-enhanced MR]. Our study also noted that only 7/436 (1.6%) of LAFs completely resolved on T2W, however their signal intensity on T2W varied in intensity over time in 33% of cases, often getting darker, but still seen as a HIZ. Gadolinium enhancement on the other hand resolved in 7/48 (14.6%). Therefore, to say that LAFs are “static lesions” is problematic; they are persistent in 99.3% of cases but they may change in signal intensity and enhancement and size [116/436 (26.6%)].
Interestingly, we noted that when the LAF changed in signal intensity or enhancement the bulge/herniation that was associated with the LAF (in 89.0% of cases) also changed either in size or characteristic. This also implies that the LAF is not a static lesion but may be a harbinger of overall discal pathology evolution. Because of that, we feel it is worthwhile reporting on LAFs in lumbar spine MR reports; only a small percentage (15.8%) of LAFs were mentioned in the official radiology dictations of the studies in our project.
To the best of our knowledge, there are relatively few longitudinal studies investigating the natural course specifically of LAFs. In 2002, Munter et al. [5] studied the serial imaging of 29 LAFs in 18 patients and concluded that all the enhancing LAFs show persistent enhancement. On the other hand, high signal intensity on T2W images was present in 96% of the cases and persisted in 88% of them. Their overall conclusion was: 1) Contrast enhanced T1W images are more sensitive in detecting the LAFs, 2) MR imaging findings of LAFs can be stable for long periods. Our study agrees with the latter but T2W scans were more sensitive for LAF in our larger series [5]. The longitudinal study by Sharma et al only looked at 46 patients and did not address the imaging features of LAFs but found a strong association between LAFs and disk degeneration [4].
In 2017, Sharma et al. [22] then looked at serial imaging of LAFs and disks on either side of a “stressed” bone in athletic young adults where the patient had bony edema in the pedicle or endplate with anterolisthesis. At baseline the stressed levels had a higher rate of annular and radial fissures. However, in follow-up (mean 19.8 months) the authors noted no increase of LAFs at the stressed levels compared to “control” disks in 42 patients (mean age 16). The nucleus pulposus however showed decreased disk signal and height over time, but not necessarily the annulus.
Elfering et al. [23] performed a longitudinal assessment of 41 asymptomatic (initially) patients over a 5-year followup. At baseline 8 patients had a LAF. Of these 8, three had resolution of the LAF at 5 years, and 3 subjects had new LAFs develop. Although 18 subjects had episodes of low back pain in the 5-year period, the painful episodes were not associated with development or resolution of the LAFs. As far as imaging features of disk degeneration over time, these authors found that baseline disk herniation (OR 12.63), evening or night work (OR 23.01) and lack of sports activity (OR 2.71) predisposed subjects to progressive deterioration [23]. Borenstein et al. [24] conducted a similar 7 year follow up of 50 asymptomatic individuals who had initial baseline MR scans, scans at the onset of episodes of pain and scans at the end of the 7 year period. They too found that MR studies of disk disease at baseline could not predict the development of episodic low back pain (which occurred in 42% of the subjects). Boos et al followed 46 patients over a five year period and noted no MR findings that predicted patient progression to symptomatic back pain [25]. Progression of MR findings of degenerative disk disease occurred in the majority of Borenstein’s patients with only 8 subjects having a normal study on follow-up but 17/41 (41.4%) showed disk degeneration progression in Boos’ cohort. Neither study specifically looked at LAFs. However, the presence of disk herniations and moderate severity degenerative disk disease correlated best with a patient’s symptoms at the time of an event [24].
What are the implications of our study? We believe that because the HIZ of the LAF persists in 99.3% of cases, one cannot “date” the age of the LAF. It may be days to months to years old. If one identifies changes in the T2W signal intensity or enhancement of the LAF, one may observe concurrent changes in the disk from a small bulge to a larger bulge, from a bulge to a herniation, and a small herniation to a larger herniation and vice versa. The LAF is not necessarily a static lesion in intensity or enhancement. We also suggest that T2W HIZs are more reliable than gadolinium enhanced scans for the detection of LAF since we saw LAFs that did not enhance initially and others that lost their enhancement over time.
This data review is from a single institution but there is no reason to think that our results would deviate from the general population given the large size of the cohort. Many of the studies did not include gadolinium enhanced sequences since our baseline degenerative spine studies do not routinely include enhanced sequences except for post-operative cases which were excluded from the cohort. Nonetheless we have follow-up enhanced data from 48 LAFs. The study required review of thousands of studies to identify the number LAFs reported herein, largely because LAFs were infrequently reported in the radiology reports. We reviewed the cases by consensus among two experienced radiologists with the most experienced radiologist (32 years after fellowship training) breaking any ties. We did not measure inter or intraobserver variability given the large sample size (436 LAFs).
We would like to address the limitation regarding LAFs and clinical correlation. The purpose of this manuscript, as stated in the title and introduction, was to show the longitudinal evolution of LAFs. The reasons we did not attempt to address the clinical symptomatology associated with the LAFs were manifold:
- Based on the purpose of the study, looking at the evolution of LAFs, our institutional IRB gave approval to review images and reports in the PACS, not to access the electronic medical record to explore patient symptomatology.
- The study was a retrospective study so we could not inquire about the patient’s complaints at the time of the examination and some studies were several years old.
- Assigning symptoms to LAFs when the literature is not definitive as to the significance of LAFs as a source of pain (see discussion above) would be misleading.
- 7% of patients had multiple LAFs. Ascribing an increase, decrease or elimination of “back pain” to a specific level of AF whether one is enhancing or not, or enlarging or not, or bright or not would be illogical in this setting, i.e. we did not do discography to identify which was the symptomatic disk.
- It would be impossible with an 88% rate of concurrent disk bulges and herniations to ascribe pain to the LAF and not other disk or facet or ligamentous or osteophytic causes.
5.Conclusion
Lumbar LAFs are prevalent findings on MR studies and are usually discovered on T2W sequences more reliably than gadolinium enhanced ones. While they rarely resolve (0.7%) they may evolve on MR studies and when they change their intensity or enhancement it may signal a dynamic evolution of disk bulges and/or herniations. They are under-reported and their correlation with patient symptomatology, while not addressed in this paper, would be worthwhile to investigate on serial clinical and imaging studies.
Author Contributions:
Faranak Rafiee, David Yousem: Conception or design of the work; Faranak Rafiee, Shadi Asadollahi, Rodrigo Luna, Mina Motaghi , David Yousem, Gary Gong: Acquisition, analysis, or interpretation of data for the work; Faranak Rafiee, Shadi Asadollahi, Rodrigo Luna, Mina Motaghi, David Yousem, Gary Gong: Drafting the work or revising it critically for important intellectual content; Faranak Rafiee, Shadi Asadollahi, Rodrigo Luna, Mina Motaghi , David Yousem, Gary Gong: Final approval of the version to be published; Faranak Rafiee, Shadi Asadollahi, Rodrigo Luna, Mina Motaghi , David Yousem, Gary Gong: Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Meisam Hoseinyazdi: analysis, or interpretation of data for the work and final approval to be published.
Conflict of interests: The authors declare no conflict of interest. Unrelated, Dr. Yousem reports royalties from Elsevier, personal fees from Medicolegal consultant, speaking and consulting fees from MRIOnline.com, outside the submitted work.
Statement of data access and integrity: The authors declare that they had full access to all of the data in this study and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Fardon DF, Williams AL, Dohring EJ, et al. Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society. The American Society of Spine Radiology and the American Society of Neuroradiology Spine J 14 (2014): 2525-2545.
- Fardon DF, Williams AL, Dohring EJ, et al. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society. The American Society of Spine Radiology and the American Society of Neuroradiolog, Spine 39 (2014): E1448-1465.
- Fardon DF, Milette PC. Combined Task Forces of the North American Spine Society ASoSR, et al. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 26 (2001): E93-E113.
- Sharma A, Pilgram T, Wippold FJ. 2nd Association between annular tears and disk degeneration: a longitudinal study. AJNR Am J Neuroradiol 30 (2009): 500-506.
- Munter FM, Wasserman BA, Wu HM, et al. Serial MR Imaging of Annular Tears in Lumbar Intervertebral Disks. AJNR Am J Neuroradiol 23 (2002): 1105-1109.
- Bogduk N, Aprill C, Derby R. Lumbar discogenic pain: state-of-the-art review. Pain Med 14 (2013): 813-836.
- Ellis DL, Ehsanian R, Shin PC, et al. Lumbar Annular High-Intensity Zone as a Precursor to Disc Extrusion. Cureus 13 (2021): e20111.
- Peng B, Hou S, Wu W, et al. The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 15 (2006): 583-587.
- Stadnik TW, Lee RR, Coen HL, et al. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology 206 (1998): 49-55.
- Ross JS, Modic MT, Masaryk TJ. Tears of the anulus fibrosus: assessment with Gd-DTPA-enhanced MR imaging. AJR Am J Roentgenol 154 (1990): 159-162.
- Vernon-Roberts B, Moore RJ, Fraser RD. The natural history of age-related disc degeneration: the pathology and sequelae of tears. Spine (Phila Pa 1976) 32 (2007): 2797-2804.
- Friberg S, Hirsch C. Anatomical and clinical studies on lumbar disc degeneration. Acta Orthop Scand 19 (1949): 222-242.
- Wang H, Li Z, Zhang C, et al. Correlation between high-intensity zone on MRI and discography in patients with low back pain. Medicine (Baltimore) 96 (2017): e7222.
- Yuan Q, Tian W, Cheng XG, et al. Comparison between CT-discography and magnetic resonance imaging in lumbar disc diseases. Zhonghua Yi Xue Za Zhi 86 (2006): 2166-2170.
- Toren L, Lagerstrand K, Waldenberg C, et al. MRI During Spinal Loading Reveals Intervertebral Disc Behavior Corresponding to Discogram Findings of Annular Fissures and Pain Provocation. Spine (Phila Pa 1976) 45 (2020): E1500-E1506
- Kakitsubata Y, Theodorou DJ, Theodorou SJ, et al. Magnetic resonance discography in cadavers: tears of the annulus fibrosus. Clin Orthop Relat Res (2003): 228-240
- Suthar P, Patel R, Mehta C, et al. MRI evaluation of lumbar disc degenerative disease. J Clin Diagn Res 9 (2015): TC04-09
- Tenny S, Gillis CC. Annular Disc Tear. StatPearls. Treasure Island (FL) (2022).
- Yu SW, Haughton VM, Sether LA, et al. Comparison of MR and diskography in detecting radial tears of the anulus: a postmortem study. AJNR Am J Neuroradiol 10 (1989): 1077-1081.
- Yu SW, Haughton VM, Sether LA, et al. Anulus fibrosus in bulging intervertebral disks. Radiology 169 (1988): 761-763.
- Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 36 (2015): 811-816.
- Sharma A, Sargar K, Salter A. Temporal Evolution of Disc in Young Patients with Low Back Pain and Stress Reaction in Lumbar Vertebrae. AJNR Am J Neuroradiol 38 (2017): 1647-1652.
- Elfering A, Semmer N, Birkhofer D, et al. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine (Phila Pa 1976) 27 (2002): 125-134.
- Borenstein DG, O'Mara JW, Jr, Boden SD, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg Am 83 (2001): 1306-1311.
- Boos N, Semmer N, Elfering A, et al. Natural history of individuals with asymptomatic disc abnormalities in magnetic resonance imaging: predictors of low back pain-related medical consultation and work incapacity. Spine (Phila Pa 1976) 25 (2000): 1484-1492.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 