Minimally Invasive Plate Osteosynthesis versus Intramedullary Nailing for Fixation of Humeral Shaft Fractures in Adults
Mohamed Samir Kassem1, Elsayed Morsi2,* , Khaled Loutfy El-Adwar3, Bahaa A Motawea1
1Assistant professor of orthopedic surgery, Faculty of Medicine, Alexandria University, Egypt
2Professor of orthopedic surgery, Faculty of Medicine, Menoufia University, Egypt
3Professor of orthopedic surgery, Faculty of Medicine, Alexandria University, Egypt
*Corresponding Author: Elsayed Morsi, professor of orthopedic surgery, Faculty of Medicine, Menoufia University, Egypt
Received: 09 January 2021; Accepted: 18 January 2021; Published: 21 January 2021
Article Information
Citation: Mohamed Samir Kassem, Elsayed Morsi, Khaled Loutfy El-Adwar, Bahaa A Motawea. Minimally Invasive Plate Osteosynthesis versus Intramedullary Nailing for Fixation of Humeral Shaft Fractures in Adults. Journal of Orthopaedics and Sports Medicine 3 (2021): 019-027.
View / Download Pdf Share at FacebookAbstract
Introduction: The two methods of treatment of humeral shaft fractures, namely minimally invasive plate osteosynthesis (MIPO), and antegrade intramedullary nailing (IMN) are reported as satisfactory procedures.
Objective: To compare the clinical and radiological results of MIPO and IMN techniques in surgical treatment of mid humeral shaft fractures.
Patients and methods: From March 2017 to July 2018, a prospective study on 60 patients with closed unilateral mid- humeral shaft fractures were surgically treated with MIPO or IMN. The intraoperative outcomes including operation time, bleeding volume, and the postoperative outcomes (clinically and radiologically) were recorded. The Constant-Murley scores were used for assessment of function of shoulder joint and Mayo score was used for measurement of elbow joint function. Complications in both groups have been reported. The follow-up duration ranged from 6 to 12 months with a mean duration of 6.7 months.
Results: For group 1 having MIPO technique, the average operative time was 90.3 min (range 50–110), while mean blood loss was 167 ml (range 120–200). In group II patients (interlocking humeral nail), the average time of operation was 100.1 min (range 65–120), and mean blood loss was 118 ml (range 90–150). The mean Constant-Murley shoulder score was 86.95±15.7 in MIPO group and 88.75±13.7in IMN group. The mean Mayo Elbow Performance score in MIPO and IMN groups was 96.5 ± 5.87 and 95.8 ± 6.77, respectively. Radiologic bony union was achieved in 29 out of 30 patients in MIPO group and in 28 out of 30 in IMN group. All the wounds in both groups healed primarily. There was no iatrogenic radial nerve palsies in both groups. Shoulder impingement was found in 2 patients in IMN group. There was no statistically significant difference between two groups in all indexes mentioned above.
Keywords
<p>Fracture humerus; MIPO; IMN; Complications</p>
Article Details
1. Introduction
Fractures of the humeral shaft are relatively common injuries [1]. Best estimates from the literature suggest that humeral shaft fractures represent approximately 3 percent of all fractures and 14% of all fractures of the humerus [1]. Humeral shaft fractures led to significant burden on society due to its bimodal distribution with a peak in young working males due to high energy trauma (road traffic accidents, falling from a height, blow to the arm and gunshot wounds), and a larger peak in older females usually by simple falls [2].
Most humeral shaft fractures can be successfully treated by nonoperative methods with acceptable healing in more than 90% of patients [2]. These conservative methods include U-shaped slab, hanging plaster cast, body bandage, prefabricated functional braces, and a simple sling [1, 2]. The indications for operative treatment include unacceptable alignment after closed reduction, multiple injuries, and radial nerve palsy after manipulation, bilateral humeral fractures, segmental fractures, and open fractures [3-6]. There are several methods of fixation available, namely, plate fixation, intramedullary nailing with Rush rods or Ender nails, locked intramedullary nailing, and external fixation [7-9]. The choice of method is based on the condition of the soft tissues, fracture location and configuration, bone quality, canal diameter, facilities and resources available, and the skills and experience of the surgical team [10, 11].
While external fixation is reserved mainly for open fractures or closed injuries with severe soft tissue compromise, plating and intramedullary nailing can both be used for most humeral shaft fractures [10]. Locked intramedullary nailing can be done through relatively small incisions and so incurs less soft-tissue trauma. However, Antegrade Locked intramedullary nailing has some disadvantages like shoulder joint and elbow joint pain and impingement due to insertion site morbidity, nonunion, iatrogenic comminution and neurovascular injury during distal locking screws? insertion [7, 8].
Plate fixation on the other hand, can provide stable fixation with excellent control of rotation, length, and angulation [12]. On the other hand, it is technically demanding, requiring extensive exposure and soft-tissue dissection, risk of infection, blood loss, and iatrogenic radial nerve or other nerve injuries. Elective removal of the plate after union also carries a great risk of nerve insult [13, 14].
As a result, there has been a strong need for a new method of fixation that avoids excessive soft-tissue stripping and devascularization of open techniques while taking the advantage of plate fixation. So the minimally invasive plate osteosynthesis (MIPO) has gained popularity in recent years with satisfactory clinical outcomes. The plate is inserted by a percutaneous approach with separate proximal and distal incisions. This method requires less soft tissue disruption and preserves the fracture hematoma and blood supply to the bone fragments [15, 16].
The aim of this work was to compare the clinical and radiological results of minimally invasive plate osteosynthesis versus intramedullary nailing for fixation of humeral shaft fractures in adults.
2. Patients and Methods
Between March 2017 to July 2018, a prospective study on 60 patients, suffering from closed humeral diaphyseal fractures, presented to El-Hadra University Hospital, Faculty of Medicine, and Alexandria University. The exclusion criteria were intra-articular fractures, non-united fractures, and fractures with radial nerve palsy requiring exploration. These patients were divided into two groups; group 1 (30 patients) was treated with MIPO, and group 2 (30 patients) was treated by locked IMN. The patients were assigned to each group randomly and alternatively as they presented. Approval of our university hospitals institutional review board, and written informed patient consents had been obtained. For group 1; age range was from 19 to 58 years old with a mean of 34.7. There were 18 males and 12 females. Right side was affected in 19 patients; and left in 11.The mechanism of injury was motor vehicle accidents in 25 cases and a fall in five. According to the AO classification: there were 15 type A (simple) fracture, 9 type B (wedge) fracture, and 6 type C (complex) fracture.
For the second group, the average age of patients was 36 years (range: 18 – 55). There were 20 males and 10 females. Right side was injured in 22 patients; and left in 8. The mechanism of injury was motor vehicle accidents in 24 cases and a fall in six. There were 17 type a (simple) fracture, 8 type B (wedge) fracture, and 5 type C (complex) fracture.
All procedures were carried out while the patients were under general anesthesia in supine position with the injured arm on a radiolucent arm board. For the patients having MIPO technique, two incisions were used. A 3 cm proximal incision was made approximately 6 cm distal to the anterior part of the acromion process, and a 3 cm incision was made along the lateral border of the biceps approximately 5 cm proximal to the flexion crease of the elbow. A sub-brachialis, extra-periosteal tunnel was created by passing the plate deep to the brachialis from the distal to the proximal incision with the help of the locked sleeve. To avoid injury to the radial nerve at the lateral aspect of the distal humerus, the plate was passed along the anterior or slightly antero-medial aspect of the humerus. The plate was then fixed to the proximal humerus with one screw or a K-wire. Reduction of the fracture was usually achieved by manipulation under image intensifier. After positioning the plate over the center of the anterior surface of the distal humerus, one screw was inserted distally. The alignment was reassessed with the image intensifier and, if satisfactory, the fixation was completed with at least three screws in each fragment. For the patients having locked IMN technique, deltoid splitting incision was made with exposure of Supraspinatus tendon. Point of entry was identified and Medullary Canal finder was inserted. Under image intensifier, reduction of fracture and guide wire insertion was done. After reaming, interlocking nail humerus with distal threads was used. The distal threads engaged into the distal bone and the proximal locking screw was inserted.
Postoperatively, the arm was put in a functional arm brace till union and the patient was encouraged to perform exercises of the shoulder and the elbow as tolerated. Follow up were carried out clinically and radiologically till union occur at 1.5, 3, 6 and 12 months. Clinically, Constant-Murley Shoulder Score [17] and Mayo Elbow Performance Score [18] were used. Serial Radiographs were used to assess reduction immediately post-operatively and to assess union.
Fracture union was defined as the presence of bridging callus radio graphically visible on at least three cortices. Statistical analysis was done using Statistical Package for Social Sciences (SPSS/version 15) software the mean follow up period was 6.7 months (range 6 – 12 months).
3. Results
For group 1 having MIPO technique, the average operative time was 90.3 min (range 50–110), mean blood loss was 167 ml (range 120–200). Pain and/or tenderness around the fracture site improved at an average of 4.1 months (range: 3–6) after the operation. The mean Constant-Murley shoulder score was 86.95±15.7 (range 58 to 100), and the mean Mayo Elbow Performance score was 96.5 ± 5.87 (range 80 to 100). Radiologic bony union was achieved in 29 out of 30 patients in 6.1 months post-operatively (range: 3–8) (Figure 1). Nonunion persisted in one patient 12 months post-operatively. He had the fracture united 3 to 4 months after a second operation of bone grafting.
In group II patients (interlocking humeral nail), the average time of operation was 100.1 min (range 65–120), mean blood loss was 118 ml (range 90–150). Pain and/or tenderness around the fracture site improved at an average of 3.9 (range: 3–6) months. The mean Constant-Murley shoulder score was 88.75±13.7 (range 59 to 100), and the mean Mayo Elbow Performance score was 95.8 ± 6.77 (range 85 to 100). Radiologic bony union was achieved in 28 out of 30 patients in 5.4 months (range: 3–7) (Figure 2). Nonunion persisted in 2 patients 12 months post-operatively. They had the fracture united 3 to 3.5 months after a second operation of bone grafting.
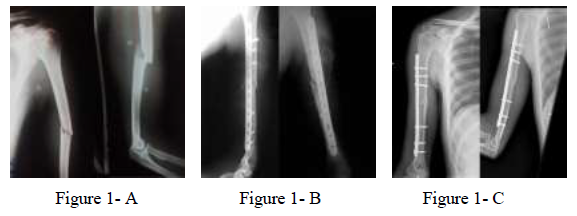
Figure 1: 42 years man with fracture mid shaft humerus. A: pre-operative X-ray showing mid shaft fracture humerus; B: post-operative X-ray with MIPO; C: 3 months post operatively showing complete union.
No statistically significant differences were seen between the results of both groups in terms of functional results and time of union. As regards the number of united cases, no statistically significant differences between the two groups were found. However, there was a statistically significant difference between the two groups in the amount of blood loss, with a significantly smaller blood loss (P < 0.05) being seen in group II patients.
With regard to complications, superficial infection occurred in one patient in each group and was treated with frequent dressing and oral antibiotics. One patient in group 1 and 2 patients in group II required a second operation of bone grafting due to persistent nonunion as mentioned above. No radial nerve palsy was found in any group. Restriction of shoulder abduction due to impingement of the nail was noted in two cases, which were later managed by removal of the nail.
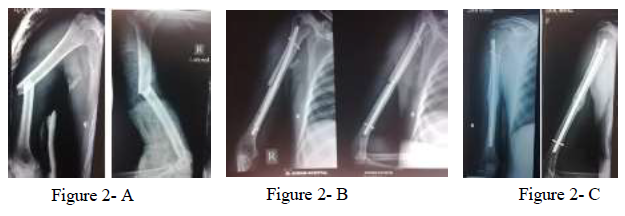
Figure 2: 39 years man with fracture mid shaft humerus. A: pre-operative X-ray showing mid shaft fracture humerus; B: post-operative X-ray with IMN; C: 4 months post operatively showing complete union.
4. Discussion
Humeral shaft fracture is one of the most common fractures in adults, accounting for approximately 3% of all fracture types [1].The choice of conservative treatment or surgical intervention for humeral shaft fractures remains controversial. However, for comminuted fractures, multiple fractures, severely displaced fractures, or fractures associated with vascular and nerve injuries, surgical treatment is still required [19]. With the continuous improvement of technology and implants, recent reports suggest that intramedullary nailing (IMN) or minimally invasive plate osteosynthesis (MIPO) have a good clinical effect in the treatment of humeral shaft fractures [20]. There is no consensus in the literature on which method is better [21-23].
Ozan et al [24] concluded that inflatable intramedullary nails seem to be applicable, safe, and effective for humeral AO/OTA type A midshaft fractures. Besides, Heinemann et al [25] performed a meta-analysis in 2010; they did not find a statistically significant difference between implants in the rate of total complications, non-union, infection, nerve-palsy, or the need for reoperation. On the contrary, Davies et al [19] performed a retrospective study; and suggested that humeral MIPO results in a significantly lower pooled major complication rate than that of IMN. Another prospective case-control work indicated that the MIPO technique in treating the mid-distal humeral shaft fracture is superior to IMN in union time, complication rate, and functional and clinical results [26].
In our study, no difference was found in, while there was significant difference in blood loss which was grater in IMN patients. There was no difference in our work between both groups in functional scores (Constant-Murley shoulder score and Mayo Elbow Performance score.
However, Restriction of shoulder abduction due to impingement of the nail was found in two cases, which were managed by removal of the nail with no functional limitations. Bisaccia (2017) [27] described the same results. Our results showed that nonunion occurred in one patients in group 1 (MIPO) compared to two cases in group 2 (IMN); but the difference is not statistically significant.
However, no significant differences in union rates have been found in most prospective studies with plate fixation shows fewer non-unions than IM nailing.Bhandari et al[28] carried out a meta-analysis of prospective studies which included 155 patients but could not formulate any conclusive preference. As regard complications, no significant differences were found between both groups as regard infection, radial nerve palsy, and nonunion.
5. Conclusions
Both MIPO and IMN methods were effective; however, MIPO method might be better for shoulder function and might reduce the nonunion rate.
Compliance with Ethical Standards
Conflict of interest
The authors report no conflict of interest, financial or otherwise, concerning the material or methods used or the findings specified in this study.
Funding
There was no financial or material support for this study.
Ethical standards
- All patients gave informed consent prior to being included in the study.
- All procedures involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments.
- The study was approved by the Research Ethics Committee.
References
- Sarmiento A, James P. Diaphyseal Humeral Fractures: Treatment options. J Bone Joint Surg (Br) 83 (2001): 1565-1579.
- Ekhoum R, Adami J, Tidermark J, et al. Outcome after closed functional treatment humeral shaft fractures. J Orthop Trauma 20 (2006): 591-596.
- Juan M, Alejandro S, Philipp N. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop (SICOT) 34 (2010):1297-1305.
- McCormack RG, Brien D, Buckely RE. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomized trial. J Bone Joint Surg (Br) 82 (2000): 336-339.
- Dykes DC, Kyle RF, Schnidt AH. Operative Treatment of Humeral Shaft Fractures: Plates versus Nails. Techniques in shoulder and elbow surgery 2 (2001): 194-209.
- Aksu N, Karaca S, Kara A. Minimally invasive plate osteosynthesis (MIPO) in diaphyseal humerus and proximal humerus fractures. Acta Orthop Traumatol Turc 46 (2012):154-160.
- Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br) 84 (2002): 1093-1110.
- Demirel M, Turhan E, Dereboy F, et al. Interlocking nailing of humeral shaft fractures a retrospective study of 114 patients. Indian J Med Sci 59 (2005): 436-442.
- Rawa S, Farooq M, Singh S, et al. Results of antegrade humeral interlocking nailing in adults A Prospective Study. Internet Surg 2 (2010): 24.
- Angelen J, Archdeacon M, Cannada L, et al. Avoiding complications in the treatment of humeral fractures. J Bone Joint Surg (Br) 90 (2008):1580-1589.
- Apivatthakakul T, Patiyasikan S, Luevitoonvechkit S. Danger zone for locking screw placement in minimally invasive plate osteosynthesis (MIPO) of humeral shaft fractures: a cadaveric study. Injury 41 (2010): 169-172.
- Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma 26 (2012): 585-589.
- Livani B, Belangero W, Andrade K, et al. Is MIPO in Humeral Shaft Fractures Really Safe? Postoperative Ultrasonographic Evaluation. Int Orthop 33 (2009): 1719 -1723.
- Shetty M, Kumar M, Sujay K, et al. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Int Orthop 45 (2011): 520-526.
- Zhou Z, Gao Y, Tang M, et al. Minimally invasive percutaneous osteosynthesis for proximal humeral shaft fractures with the PHILOS through the deltopectoral approach. Int Orthop (SICOT) 36 (2012): 2341-2345.
- Ziran B, Kinney R, Smith W, et al. Sub-muscular plating of the humerus: An emerging technique. Injury 6 (2010):1047-1052.
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research 214 (1987): 160-164.
- Turchin Diana C, Dorcas E Beaton, Robin R Richards. Validity of observer-based aggregate scoring systems as descriptors of elbow pain, function, and disability. JBJS 80.2 (1998): 154-162.
- Davies G, Yeo G, Meta M, et al. Case-Match Controlled Comparison of Minimally Invasive Plate Osteosynthesis and Intramedullary Nailing for the Stabilization of Humeral Shaft Fractures. J Orthop Trauma 30 (2016): 612-617.
- Wen H, Zhu S, Li C, et al. Antegrade intramedullary nail versus plate fixation in the treatment of humeral shaft fractures. An update meta-analysis. J Medicine (Baltimore) 98 (2019): 1-10.
- Kulkarni M, Kulkarni V, Kulkarni S. Treatment of Humerus Diaphyseal Fractures with Minimally Invasive Plate Osteosynthesis. J Fract Sprains 1 (2017): 1-7.
- Tetsworth K, Hohmann E, Glatt V. Minimally Invasive Plate Osteosynthesis of Humeral Shaft Fractures: Current State of the Art. JAAOS 26 (20180: 652-661.
- Connors K, Hawken J. Surgical Management of Humeral Shaft Fractures – What is the Best Choice? Ely J Surg 1 (2018):1-4.
- Ozan F, Gürbüz K, Uzun E, et al. The inflatable intramedullary nail for humeral shaft fractures. J Orthop 14 (2017): 137-141.
- Heineman DJ, Poolman RW, Nork SE, et al. Plate fixation or intramedullary fixation of humeral shaft fractures. An updated meta-analysis. Acta Orthopaedica 81 (2010): 216-223.
- Chang H, Yao ZL, Hou YL, et al. Lateral Subcutaneous Locking Compression Plate and Small Incision Reduction for Distal-third Diaphyseal Humerus Fractures. J Orthop Surg 10 (2018): 218-226.
- Bisaccia M, Meccariello L, Rinonapoli G, et al. Comparison of Plate, Nail and External Fixation in the Management of Diaphyseal Fractures of the Humerus. Med Arch 71 (2017): 97-102.
- Bhandari M, Devereaux PJ, McKee MD, et al. Compression plating versus intramedullary nailing of humeral shaft fractures, a meta-analysis. Acta Orthop Belgica 77 (2006): 279-284.
Article Views: 2512
Journal Statistics




Discover More: Recent Articles


