Obesity and diabetes are the strongest predictors of post-acute COVID-19 in Coptic clergy and monks
Michael Y. Henein1,2*, Rafik Shenouda1, Magdi Matter3, Ibadete Bytyçi1,4
1Institute of Public Health and Clinical Medicine, Umea University, Umea, Sweden
2Molecular and Clinic Research Institute, St George University, London, and Brunel University, UK
3St Takla Heart Centre, Alexandria, Egypt
4Clinic of Cardiology, University Clinical Centre of Kosovo, Kosovo
*Corresponding author: Michael Y. Henein, Institute of Public Health and Clinical Medicine, Umea University, Umea, Sweden.
Received: 15 March 2022; Accepted: 22 March 2022; Published: 12 April 2022
Article Information
Citation: Michael Y. Henein, Rafik Shenouda, Magdi Matter, Ibadete Bytyçi. Obesity and diabetes are the strongest predictors of post-acute COVID-19 in Coptic clergy and monks. Archives of Clinical and Biomedical Research 6 (2022): 364-377.
View / Download Pdf Share at FacebookAbstract
Background and Aims: In contrast to priests, the life style of monks is almost similar, irrespective of their order and specifics of religious practices. The aim of this study was to assess the cardiac risk factors in Coptic priests and monks and their impact on post- acute COVID-19.
Methods: Of 1519 clergy, participating in the COVID-19-Clergy study, serving in Europe and Egypt, 257 had the infection and were included in this analysis. Clergy were divided into priests (n=204) and monks (n=53). Participants’ demographic indices, cardiovascular risk factors, management details and post-acute COVID-19 duration were assessed. The impact of geographic differences of life style were also analysed.
Results: Priests were more obese (p=0.001), had more type 2 diabetes (DM) (p=0.001), arterial hypertension (AH) (p<0.001), dyslipidemia (p=0.001) and lower prevalence of infection (p<0.001) compared to monks. Their symptoms’ duration was more prolonged (p<0.001), had frequent post-acute COVID (p<0.001) and had greater need for hospital treatment (p=0.04). In a sub-analysis, priests serving in Europe had higher prevalence of AH, DM, obesity, CHD, dyslipidemia, longer symptoms duration and more frequent post-acute COVID compared to monks from Europe (p<0.05 for all). Similarly, those risk factors were higher in priests serving in Northern Egypt compared to local monks (p<0.05 for all). Symptoms’ duration correlated directly with severity of obesity (rpb = 0.54, p=0.001) and frequency of diabetes (rpb = 0.58, p<0.001). In multivariate analysis, DM 2.56 [(1.189 to 5.524); p=0.01] and morbid obesity OR 2.11 [(1.109 to 4.923); p=0.02] predicted post-acute COVID-19 in the Coptic clergy, particularly priests, while age and moderate obesity were the main predictors in monks (p<0.05 for all).
Keywords
<p>COVID-19; Coptic clergy; cardiovascular risk factors; monks; priests</p>
Article Details
1. Introduction
The Covid-19 pandemic continues to have strong impact on the population worldwide, especially on individuals with pre-existing comorbidities [1]. Of those affected, about 80% develop mild to moderate disease and among the remaining with severe disease, 5% develop critical illness [2]. Persistent symptoms and clinical instability, described as long or post-acute COVID-19, is common in adults hospitalized with severe COVID-19 and is recently becoming a major health issue worldwide [3]. Some demographic indices have been shown to be associated with long COVID-19 including female gender and old age [4]. Also, assessment of demographics and ethnicity on the natural history of the disease during the first infection wave reported significant impact of blacks, Asian and ethnic minorities (BAME) [5, 6]. Along the same line, we have previously reported high COVID-19 prevalence among Coptic clergy and explained it on the basis of their particular life style and frequent regular community services, which require close contact with their parishioners. We have also highlighted the important role of obesity in explaining this high disease prevalence [7, 8]. Furthermore, most sufferers developing COVID-19 complications had significant co-morbidities and the cumulative cardiac risk factors was the most powerful predictor of COVID-19 related mortality and the need for mechanical ventilation [9, 10]. The aim of this study was to assess the cardiac risk factors among clergy and monks and their impact on post-acute COVID-19 and the need for hospital treatment.
2. Methods
2.1. Study design and patients
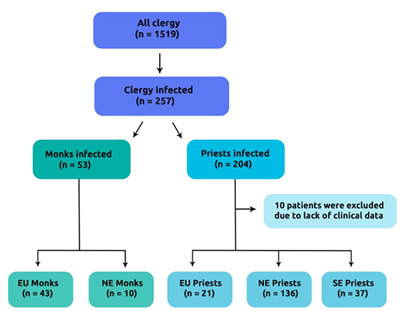
The present study is a retrospective evaluation of a cohort of 1519 Coptic clergy from Egypt and Europe, from March to December 2020. It is a sub-study from the COVID-19- CVD international study, which investigates the impact of COVID-19 on the cardiovascular system and which is approved by the Swedish Ethics Board (Dnr 2020- 02217 Stockholm avdelning 2 medicin) and the International Cardiac Centre-ICC Ethics Board (ICC, 3/2021, Egypt). M.Y.H. (The Principal Investigator) designed and administrated the project which was endorsed by the Head of the Coptic Church in Egypt. Out of 1519 clergy, 257 (16.9%) had the infection, 10 of them were excluded due to lack of clinical data. Based on the difference in pattern of life and place of service, Coptic clergy were divided into priests (n=204) (who lived and served in open communities) and monks (n=53) (who lived and served in closed communities i.e. monasteries). In addition, clergy were subdivided according to their geographic distribution into those living in Egypt or Europe (Flow chart of participants is presented in Figure S1).
2.2. Cardiovascular risk factor assessment
Cardiovascular risk factors such as type 2 Diabetes Mellitus (DM), Arterial Hypertension (AH), Coronary Heart Disease (CHD), dyslipidemia, obesity and family history of cardiovascular disease and stroke were assessed based on medical records information and prior investigations and management data. According to the World Health Organization, conventional international risk factor assessment and cut-off values for body mass index (BMI), underweight was defined as BMI <18.5 kg/m2, normal weight as BMI 18.5-24.9 kg/m2, overweight as BMI of 25 – 29.9 kg/m2 and obese as BMI ≥30 kg/m2. Obesity was further classified into three classes: class I - moderately obese (30- 34.9 kg/m2), class II - severely obese (35-39.9 kg/m2) and class III (≥30 kg/m2) as morbidly obese [11]. Type 2 Diabetes Mellitus (DM) was identified based on pre- recruitment diagnosis leading to participants commenced on conventional oral hypoglycemics and/or insulin therapy. Systemic AH was diagnosed when systolic blood pressure (SBP) was ≥130 mmHg and/or diastolic blood pressure (DBP) was ≥80 mmHg. Dyslipidemia was determined from medical records or if the individual had been commenced on statins. Evidence for coronary artery disease was also evaluated based on medical records information, and prior investigations and management data.
2.2. Clinical events
Clinical Events (CE) details were retrospectively collected and information on participants’ clinical outcome was obtained from medical records, clinical visits, personal communication with general physicians and confidential telephone interviews with patients and relatives. The study primary outcome was frequency of post- acute COVID-19; the secondary outcome was the need for hospitalization. Based on the duration of symptoms, post-acute COVID-19 was defined as symptoms extending beyond 3 weeks, but less than 12 weeks of the acute infection [4].
2.3. Statistical analysis
Discrete data are reported as frequencies (percentages) and continuous variables as means and Standard Deviation (SD) if normally distributed, or median and Interquartile Range (IQR: Q1–Q3) in case of skewed distribution. Continuous data were compared with two- tailed Student t test and discrete data with Chi-square test. The degree of association between cardiac risk factors and symptoms’ duration was determined using the Pearson’s correlation coefficient in the case of continuous variables; chi-square test (categorical and categorical variables) and point biserial correlation were used in the case of categorical and continuous variables. Predictors of post-acute COVID-19 and the need for hospitalization were identified using univariate and multivariate analyses. A significant difference was defined as p value <0.05 (2-tailed). Statistical analysis was performed with SPSS Software Package version (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Demographic and clinical data of priests versus monks
The prevalence of infection was lower in priests compared to monks, despite similar age between groups (p<0.002, p=0.28; respectively). More priests were obese (57.7 vs. 15.1%; p=0.001), had frequent type 2 DM (28.9 vs. 7.54%; p=0.001), systemic AH (34.9 vs. 5.66%; p<0.001), dyslipidemia (31.4 vs. 9.43%; p=0.001) and family history for CHD (11.8 vs. 3.77%; p=0.03) compared to monks. The frequency of CHD tended to be higher in priests (p=0.09) while that of family history for stroke was not different between the two groups (p>0.05; Table 1).
Table 1: Demographic, clinical and outcome data of priests vs. monks
|
Variable |
Priests |
Monks |
P |
|
(n=204) |
(n = 53) |
value |
|
|
Prevalence (%) |
14.4 ± 10 |
55.1 ± 43 |
0.001 |
|
Age |
49.3 ± 12 |
47.2 ± 15 |
0.28 |
|
BMI (m/kg2) |
31.9 ± 5.9 |
24.9 ± 4.3 |
<0.001 |
|
Underweight (n, %) |
0 (0) |
3 (5.66) |
<0.001 |
|
Normal weight (n, %) |
17 (8.33) |
25 (47.1) |
<0.001 |
|
Overweight (n, %) |
69 (33.8) |
17 (32.1) |
0.22 |
|
Obese (n, %) |
117 (57.7) |
8 (15.1) |
0.001 |
|
Class I (n, %) |
73 (35.8) |
7 (13.2) |
<0.001 |
|
Class II (n, %) |
26 (12.7) |
1 (1.88) |
0.001 |
|
Class III (n, %) |
18 (8.82) |
0 (0) |
<0.001 |
|
AH (n, %) |
71 (34.9) |
3 (5.66) |
<0.001 |
|
DM (n, %) |
59 (28.8) |
4 (7.54) |
0.001 |
|
Dyslipidemia |
63 (31.4) |
5 (9.43) |
0.01 |
|
CHD (n, %) |
21 (10.1) |
4 (6.66) |
0.09 |
|
Family history for CHD (n, %) |
24 (11.8) |
2 (3.77) |
0.03 |
|
Family history for stroke (n, %) |
13 (6.53) |
3 (5.76) |
0.38 |
|
Outcome data |
|||
|
Symptoms’ duration |
17.8 ± 9.8 |
10.8 ± 7.1 |
<0.001 |
|
Post-acute COVID (n, %) |
44 (21.4) |
5 (9.43) |
0.001 |
|
Hospital treatment (n, %) |
34 (16.9) |
22 (11.3) |
0.04 |
|
AH: arterial hypertension; BMI: Body mass index; CHD: Coronary heart disease; DM: diabetes mellitus |
|||
3.2. Geographical impact on life style and infection
The overall prevalence of COVID-19 among priests serving in Europe was higher compared to local monks (p<0.001). They also had higher prevalence of AH, type 2 DM, CHD, dyslipidemia as well as family history for CHD and stroke compared to monks living in closed order in Europe (p<0.05 for all). Among European priests, the frequency of normal weight was less (14.3 vs 44.2%; p<0.001), while overweight was higher (58.3 vs. 30.2%; p=0.001) as was obesity (27.4 vs. 16.3%; p=0.003) compared to local monks. There was no difference in age between priests and monks in Europe (p=0.31). In contrast, the prevalence of type 2 DM and CHD did not differ between priests and monks serving and living in Northern Egypt (p>0.05), while the other risk factors were higher in priests compared to local monks (p<0.05 for all, Table 2).
Table 2: Demographic, clinical and outcome data of Coptic clergy in different regions.
|
Variable |
EU priests |
EU monks |
P |
NE priests |
NE monks |
P |
|
(n=21) |
(n = 43) |
value |
(n=136) |
(n=10) |
value |
|
|
Prevalence (%) |
12.8 ± 5.9 |
86.0 ± 9.8 |
<0.001 |
18.3 ± 14 |
24.4 ± 11 |
0.04 |
|
Age (years) |
51.7 ± 13 |
47.3 ± 15 |
0.31 |
49.6 ± 11 |
46.9 ± 14 |
0.49 |
|
BMI (m/kg2) |
29.1 ± 5.1 |
24.4 ± 4.6 |
0.01 |
32.9 ± 5.7 |
26.6 ± 1.9 |
0.001 |
|
Underweight (n, %) |
0 (0) |
4 (9.30) |
0.02 |
0 (0) |
0 (0) |
0.92 |
|
Normal weight (n, %) |
3 (14.3) |
19 (44.2) |
<0.001 |
8 (6.10) |
2 (20) |
0.01 |
|
Overweight (n, %) |
12 (58.3) |
13 (30.2) |
0.001 |
47 (34.3) |
7 (70) |
<0.001 |
|
Obese (n, %) |
6 (27.4) |
7 (16.3) |
0.003 |
81 (59.9) |
1 (10) |
0.001 |
|
Class I (n, %) |
4 (19.1) |
6 (13.9) |
0.02 |
53 (38.9) |
1 (10) |
<0.001 |
|
Class II (n, %) |
1 (4.76) |
1 (2.32) |
0.06 |
16 (12.1) |
0 (0) |
<0.001 |
|
Class III (n, %) |
1 (4.76) |
0 (0) |
<0.001 |
12 (8.90) |
0 (0) |
0.001 |
|
AH (n, %) |
5 (25.0) |
0 (0) |
<0.001 |
52 (38.3) |
3 (30) |
0.06 |
|
DM (n, %) |
10 (47.6) |
1 (2.32) |
<0.001 |
36 (26.7) |
3 (30) |
0.22 |
|
Dyslipidemia |
5 (25.0) |
0 (0) |
<0.001 |
47 (34.6) |
5 (50) |
0.02 |
|
CHD (n, %) |
4 (18.2) |
1 (2.32) |
0.001 |
15 (11.3) |
1 (10) |
0.41 |
|
Family history for CHD (n, %) |
9 (45.1) |
0 (0) |
<0.001 |
14 (10.7) |
2 (20) |
0.03 |
|
Family history for stroke (n,%) |
3 (16.1) |
3 (5.76) |
0.02 |
13 (6.53) |
3 (33.0) |
0.001 |
|
Outcome data |
||||||
|
Symptoms’ duration |
16.5 ± 9.7 |
10.3 ± 6.8 |
0.01 |
18.1 ± 10 |
12.1 ± 8.4 |
0.03 |
|
Post-acute COVID (n, %) |
5 (25.0) |
4 (9.30) |
0.001 |
27 (19.8) |
1 (10) |
0.01 |
|
Hospital treatment (n, %) |
5 (25.0) |
5 (11.6) |
0.01 |
21 (15.4) |
2 (10) |
0.06 |
|
AH: arterial hypertension; BMI: Body mass index; CHD: Coronary heart disease; DM: diabetes mellitus; EU: European; NE: Northern Egypt |
||||||
3.3. Impact of cardiovascular risk factors on symptoms duration
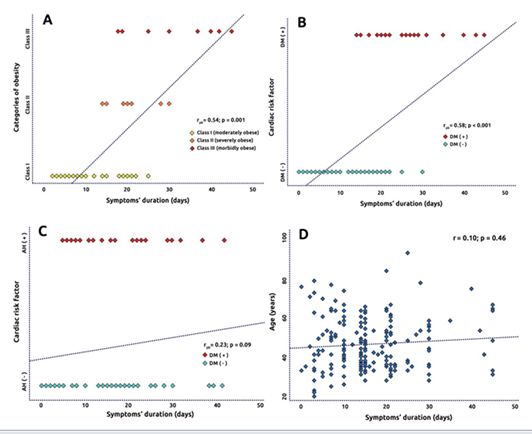
Diabetes strongly correlated with the duration of symptoms (rpb = 0.58, p<0.001). Similarly, symptoms duration increased linearly with severity of obesity from moderate, severe to morbid (rpb = 0.54, p=0.001). In contrast, no relationship was found between age and symptoms duration (r=10, p=0.46), while arterial hypertension tended to have a relationship (rpb = 0.23, p=0.09, Figure 1A, D).
3.4. Predictors of post-acute COVID-19 and the need for hospitalization
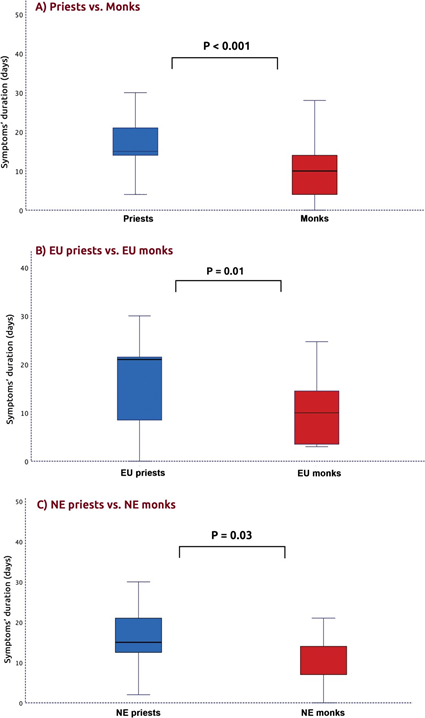
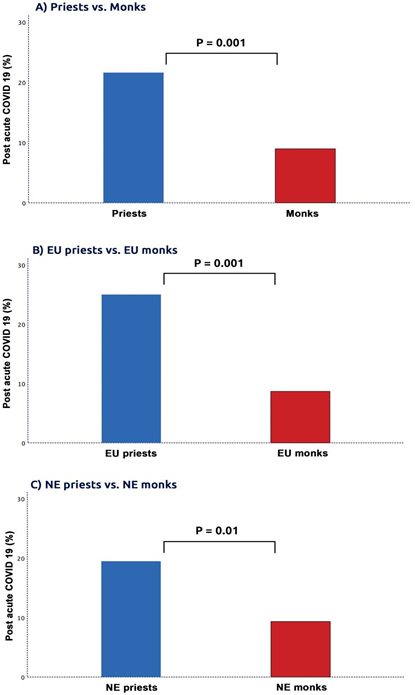
In the group of Coptic priests as a whole, the duration of symptoms was longer (17.8 ± 9.8 vs. 10.8 ± 7.1 days; p<0.001, Figure 2) post-acute COVID-19, more frequent (21.4 vs. 11.3%; Figure 3) and hospital treatment more needed (16.9 vs. 11.3%; p=0.04; Table 1) compared to monks. The Coptic priests from Europe had prolonged symptoms, higher frequency of post-acute COVID-19 and greater need for hospital treatment compared to monks from Europe (p<0.05 for all). Similarly, those clinical events were higher in priests serving in Northern Egypt compared to local monks (p<0.05 for all, Table 2). In univariate analysis, type 2 DM (p = 0.006), CHD (p = 0.04), severe obesity (p = 0.03), and morbid obesity (p=0.01) predicted post-acute COVID-19 in the group of clergy as a whole. In multivariate analysis model, only diabetes, [OR 2.562 (1.189 to 5.524); p = 0.007)] and morbid obesity [OR 2.112 (1.109 to 4.923); p = 0.02)] predicted the frequency of post-acute COVID-19. Testing the impact of the pattern of life and specifics of religious practices related post-acute COVID-19 showed that type 2 DM and morbid obesity were the most powerful independent predictors in priests comparted to age and moderate obesity in monks (Table 3). Almost similarly, type 2 DM (p=0.01), morbid obesity (p=0.03) and AH (p=0.04) independently predicted the COVID-19-related hospitalization in clergy. Morbid obesity and type 2 DM were the most powerful independent predictors of hospitalization in priests while type 2 DM and AH in monks (Table S1).
Table 3: Predictors of COVID-19 prolonged
|
Variable |
Univariate predictors OR (95% CI) All clergy |
P value |
Multivariate predictors OR (95% CI) |
P value |
|
Age |
1.013 (0.437 to 2.095) |
0.22 |
||
|
Diabetes |
2.735 (1.337 to 5.595) |
0.006 |
2.562 (1.189 to 5.524) |
0.01 |
|
AH |
1.165 (0.819 to 3.348) |
0.16 |
||
|
Dyslipidemia |
1.318 (0.427 to 4.073) |
0.61 |
||
|
CHD |
1.441 (0.709 to 2.298) |
0.04 |
1.198 (0.556 to 2.511) |
0.18 |
|
Moderately obese |
1.280 (0.927 to 2.373) |
0.08 |
||
|
Severely obese |
2.005 (1.025 to 3.806) |
0.03 |
||
|
Morbidly obese |
2.516 (1.209 to 4.149) |
0.01 |
2.112 (1.109 to 4.923) |
0.02 |
|
Priests |
||||
|
Age |
0.978 (0.445 to 1.096) |
0.44 |
||
|
Diabetes |
2.143 (0.045 to 4.196) |
0.04 |
1.901 (1.113 to 3.889) |
0.03 |
|
AH |
1.122 (0.530 to 2.537) |
0.61 |
||
|
Dyslipidemia |
0.703 (0.419 to 1.619) |
0.79 |
||
|
CHD |
0.751 (0.222 to 2.544) |
0.67 |
||
|
Moderately obese |
0.920 (0.698 to 2.104) |
0.13 |
||
|
Severely obese |
1.512 (1.088 to 3.709) |
0.04 |
||
|
Morbidly obese |
1.838 (1.105 to 3.541) |
0.01 |
2.044 (1.219 to 4.041) |
0.02 |
|
Monks |
||||
|
Age |
1.161(1.007 to 1.399) |
0.02 |
1.501(1.077 to 2.019) |
0.04 |
|
Diabetes |
1.711 (1.097 to 3.601) |
0.04 |
||
|
AH |
1.122 (0.530 to 2.537) |
0.61 |
||
|
Dyslipidemia |
1.031 (1.007 to 4.019) |
0.11 |
||
|
CHD |
1.018 (0.807 to 3.019) |
0.57 |
||
|
Overweight |
2.047 (1.108 to 3.397) |
0.04 |
1.126 (1.082 to 4.017) |
0.09 |
|
Moderately obese |
1.808 (1.015 to 3.541) |
0.03 |
1.113 (0.811 to 3017) |
0.04 |
|
AH: arterial hypertension; BMI: Body mass index; CHD: Coronary heart disease; DM: diabetes mellitus |
||||
4. Discussion
Findings: The prevalence of infection was lower in priests but cardiovascular risk factors were more prevalent compared to monks. However, priests had more prolonged symptoms and greater need for hospitalization than geographically similar aged monks. Type 2 diabetes and morbid obesity were the two main independent cardiovascular risk factors that predicted long COVID-19 in priests whereas moderate obesity and old age were the respective predictors in monks. The same risk factors predicted priests’ hospitalization compared to DM and hypertension in monks.
Data interpretation: Our findings demonstrate the profound importance of obesity in impacting individual’s susceptibility to catch COVID-19 and to develop prolonged symptoms, irrespective of the body system the infection impacted, that frequently required hospital treatment. We have previously shown that obesity is very common among Coptic priests and is the sole factor that contributed to the COVID-19 infection [7]. The current findings, despite included two additional groups of clergy ‘monks’ who live a quite different style of life i.e in remote and isolated monasteries, support the former report [7, 12]. In fact, large population studies have also shown that obesity is the main predictor of COVID-19 related complications including the need for ventilation, in order to maintain a physiological oxygen level in the circulation [13, 14]. Classifying obesity into three categories, moderate, severe and morbid has further highlighted its clinical impact. Morbid obesity proved to be the worse risk factor related to prolonged COVID-19, and to have an exponential relationship with the duration of illness and symptoms [15, 16]. Our findings also show that diabetes is the second important risk factor that predicted prolonged COVID, irrespective of where clergy lived, in open or closed community [17, 18]. These findings support what other population studies have shown [19, 20] that obesity and diabetes are the two worse risk factors in patients suffering from COVID-19.
Obesity and diabetes are two well established cardiovascular risk factors that are closely related and the two share their suppressing impact on the human immune system, hence the potential explanation of the long COVID in patients carrying both risks [21- 23]. The lower infection rate with COVID seems to be significant in priests serving in open community compared with monks living in closed communities, irrespective of their geographical location. This finding is of particular interest, since it reflects and translates the fast infection spread rate in closed community, where monks share meals, work activities and worship disciplines in confined places, compared to open community where priests are not exposed to similar life style risk, but they mix more with parishioners who might be less infected/carriers. Finally, our results suggest the likelihood of environmental circumstances as a potential risk factor for catching COVID infection, as is the case with Egyptian and European monks, compared to personally inflected risk factors, particularly diabetes and obesity, as predictors of long COVID in the case of priests.
Clinical implications: Our findings, although in a limited sector of the community, are consistent with what population studies have shown that obesity and diabetes are two very important risk factors for COVID-19 infection and long symptoms’ duration. The same two risk factors are similarly important players in the pathophysiology of life- threatening conditions e.g. coronary artery disease and stroke [24] as well as other related conditions. These findings suggest a serious need for prioritizing patients with those risk factors for optimum protection including vaccination, as well as optimum antibiotic cover for viral infection.
Limitations: This study has some limitations. The study design was retrospective with its known limitations including limited data about individual risk factors including duration and severity. However, a study like this can not be designed and run in a prospective way. The relatively small number of participants reflects the difficult nature of the study, design and data collection. Definition of long COVID was made by local physicians, who might differ in their expertise and criteria of diagnosing long COVID. Details about the nature of long COVID in individual patients were not available.
5. Conclusion
In Coptic priests, the cardiovascular risk factors were more prevalent compared to monks. Diabetes and obesity were the two most powerful predictors of post- acute COVID-19. Severity of obesity correlate directly with COVID related symptoms duration.
Declaration of interest
The authors have no conflict of interest to declare.
Funding
This research received no external funding.
Author contributions
M.Y.H.: Conceptualization, study design, methodology and project administration; I.B., R.S., M.B.: data analysis and writing the first draft of manuscript. All authors have read and agreed to the published version of the manuscript.
References
- Guarisco G, Leonetti F. Covid-19 and diabesity: when a pandemia cross another pandemia. Eat Weight Disord 26 (2021): 1283-1286.
- Gong Zhenyu, Gong Xunliang. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network — United States, March–June 2020[J]. Disease Surveillance 35 (2020): 1158-1160.
- N Nikki. Long covid: how to define it and how to manage it. BMJ 370 (2020).
- Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: An overview. Diabetes Metab Syndr 15 (2021): 869-875.
- Pillaye J. Covid-19 and ethnic minorities: the Public Health England report distracts from proactive and timely intervention. BMJ 370 (2020): 3054.
- Keys C, Nanayakkara G, Onyejekwe C, et al. Health Inequalities and Ethnic Vulnerabilities During COVID-19 in the UK: A Reflection on the PHE Reports. Fem Leg Stud (2021):1-12.
- Henein MY, Bytyçi I, Nicoll R, et al. Obesity Strongly Predicts COVID-19-Related Major Clinical Adverse Events in Coptic Clergy. J Clin Med 10 (2021): 2752.
- Petrakis D, Margina D, Tsarouhas K, et al. Obesity - a risk factor for increased COVID-19 prevalence, severity and lethality (Review). Mol Med Rep 22 (2020): 9-19.
- Shi S, Qin M, Shen B, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol 5 (2020): 802-810.
- Henein MY, Bytyçi I, Nicoll R, et al. Combined Cardiac Risk Factors Predict COVID-19 Related Mortality and the Need for Mechanical Ventilation in Coptic Clergy. J Clin Med 10 (2021): 2066.
- Weir CB, Jan A. BMI Classification Percentile And Cut Off Points 2021 (2021): 31082114.
- Bramstedt KA. COVID-19 as a Cause of Death for Catholic Priests in Italy: An Ethical and Occupational Health Crisis. Health Soc. Care Chaplain 8 (2020):180-190.
- Belanger MJ, Hill MA, Angelidi AM, et al. Covid-19 and Disparities in Nutrition and Obesity. N Engl J Med 383 (2020): 69.
- Edwards DA, Ausiello D, Salzman J, et al. Exhaled aerosol increases with COVID-19 infection, age, and obesity. Proc. Natl. Acad. Sci. USA 118 (2021): 2021830118.
- Valente M, Ricco M, Tartamella F, et al. Clinical case definition of COVID-19 and morbid obesity: Is it time to move on? Infect Dis Now 51 (2021): 567-569.
- Wysocki M, Waledziak M, Proczko-Stepaniak M, et al. Lifestyle changes in patients with morbid obesity and type 2 diabetes mellitus during the COVID-19 pandemic. Diabetes Metab 47 (2021):
- Samean L. Covid-19 infections take toll on monks, clergies in Kingdom. The Phnom Penh Pos 2021
- Lee B. Clergy and COVID-19. The regulatory review (2020).
- Krams IA, Luoto S, Rantala MJ, Jõers P, Krama T.Pathogens. Covid-19: Fat, Obesity, Inflammation, Ethnicity, and Sex Differences 9 (2020): 887.
- Sourij H, Aziz F, Bräuer A, et al. COVID-19 in diabetes in Austria study group. COVID-19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission. Diabetes Obes Metab 23 (2021): 589-598.
- Abdi A, Jalilian M, Sarbarzeh PA, et al. Diabetes and COVID-19: A systematic review on the current evidences. Diabetes Res Clin Pract 166 (2020): 108347.
- Kumar A, Arora A, Sharma P, et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr 14 (2020): 535-545.
- Raveendran AV, Misra A. Post COVID-19 Syndrome ("Long COVID") and Diabetes: Challenges in Diagnosis and Management. Diabetes Metab Syndr 15 (2021):102235.
- Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European Society of Cardiology ESC-EORP EUROASPIRE V registry.Eur J Prev Cardiol 26 (2019): 824-835.
Supplementary data
Table S: Predictors of COVID-19 related hospitalization.
|
Variable |
Univariate OR (95% CI) |
P value |
Multivariate OR (95% CI) |
P value |
|
Age |
1.103 (1.061 to 2.038) |
0.01 |
||
|
Diabetes |
1.978 (1.037 to 4.318) |
0.001 |
2.562 (1.189 to 5.524) |
0.01 |
|
AH |
1.738 (1.092 to 3.719) |
0.04 |
2.101 (1.112 to 3.902) |
0.04 |
|
Dyslipidemia |
1.441 (0.709 to 2.298) |
0.07 |
1.198 (0.556 to 2.51) |
0.18 |
|
CHD |
3.018 (1.207 to 6.013) |
0.01 |
||
|
Moderately obese |
1.360 (0.628 to 2.994) |
0.19 |
||
|
Severely obese |
1.270 (1.025 to 4.006) |
0.42 |
||
|
Morbidly obese |
2.516 (1.209 to 4.149) |
0.01 |
2.112 (1.109 to 4.923) |
0.03 |
|
Priests |
||||
|
Age |
1.175 (1.039 to 1.796) |
0.001 |
||
|
Diabetes |
1.607 (0.645 to 3.226) |
0.11 |
1.901 (1.113 to 3.889) |
0.04 |
|
AH |
1.362 (0.530 to 3.148) |
0.47 |
||
|
Dyslipidemia |
2.125 (0.884 to 2.519) |
0.09 |
||
|
CHD |
3.421 (1.022 to 9.944) |
0.03 |
||
|
Moderately obese |
1.144 (0.408 to 2.689) |
0.65 |
||
|
Severely obese |
1.304 (0.408 to 4.101) |
0.31 |
||
|
Morbidly obese |
1.838 (1.105 to 3.541) |
0.01 |
2.044 (1.219 to 4.041) |
0.02 |
|
Monks |
||||
|
Age |
1.061(1.003 to 1.209) |
0.04 |
1.501(1.007 to 4.019) |
0.06 |
|
Diabetes |
2.611 (1.207 to 5.601) |
0.04 |
1.909 (1.097 to 2.519) |
0.03 |
|
AH |
1.202 (1.101 to 2.037) |
0.03 |
2.107 (1.703 to 4.191) |
0.04 |
|
Dyslipidemia |
1.760 (0.227 to 18.19) |
0.64 |
||
|
CHD |
1.018 (0.807 to 3.019) |
0.57 |
||
|
Overweight |
0.347 (0.038 to 2.315) |
0.33 |
||
|
Moderately obese |
3.280 (0.498 to 21.59) |
0.02 |
1.113 (0.811 to 3017) |
0.1 |
|
AH: arterial hypertension; BMI: Body mass index; CHD: Coronary heart disease; DM: diabetes mellitus; |
||||
Article Views: 1568
Journal Statistics




Discover More: Recent Articles