Outcomes of Coracoid Bone Graft Positioning During the Latarjet Procedure with Respect to Surgical Approach
Gary L. Ulrich MD1*, Shariff K. Bishai DO, MS2
1Department of Orthopedic Surgery, University of Kentucky College of Medicine, Lexington, KY, USA
2Associated Orthopedists of Detroit, P.C., Detroit, MI, USA
*Corresponding Author: Gary L. Ulrich, Department of Orthopedic Surgery, University of Kentucky College of Medicine, Lexington, KY, USA.
Received: 14 August 2023; Accepted: 25 August 2023; Published: 04 September 2023
Article Information
Citation:
Gary L. Ulrich, Shariff K. Bishai. Outcomes of Coracoid Bone Graft Positioning During the Latarjet Procedure with Respect to Surgical Approach. Journal of Orthopedics and Sports Medicine 5 (2023): 346-356.
View / Download Pdf Share at FacebookAbstract
The Latarjet procedure represents a successful treatment option for patients with recurrent shoulder instability with glenoid bone loss, and its indications are expanding. One of the most important steps of the Latarjet procedure with respect to outcome is the positioning of the coracoid graft in both the oblique axial and sagittal planes. In the axial plane, a graft placed too medial can result in recurrent instability, whereas a graft placed too lateral can result in development of osteoarthritis. In the sagittal plane, the coracoid graft is ideally positioned in a subequatorial position to best restore stability as a graft positioned too inferior or too superior could result in recurrent instability. In this review, we discuss the outcomes of coracoid graft positioning with respect to surgical approach, including the open, mini-open, arthroscopically assisted, and all-arthroscopic approaches to the Latarjet procedure.
Keywords
<p>Coracoid graft position; Placement; Approach; Open; Arthroscopic</p>
Article Details
Abbreviations:
CT: Computed Tomography
1. Introduction
The Latarjet procedure, eponymously known by Dr. Michel Latarjet’s procedural description in 1954, involves the transfer of the coracoid process from its native position to the anterior-inferior aspect of the glenoid neck [1,2]. Through this coracoid graft transfer, the Latarjet procedure provides stability to the shoulder through three mechanisms, which is known as “triple blocking.” First, the coracoid graft extends the glenoid articular surface in the anterior-posterior dimension, which offers stability and causes a larger distance for the humeral head to travel before dislocation or a large Hill-Sachs lesion engaging with the anterior glenoid rim occurs. Second, the conjoint tendon remains attached to the coracoid process during the transfer; thus, along with the inferior half of the subscapularis, the conjoint tendon acts as a dynamic soft-tissue sling restricting anterior subluxation of the humeral head in the abduction and external rotation shoulder position. Third, the glenohumeral capsule can be repaired to the coracoacromial ligament, which creates a strong adjunct to the inferior glenohumeral ligament, since the native ligament is often irreversibly elongated from the shoulder dislocation injury [3-5]. With this triple blocking mechanism, the Latarjet procedure has had estimated rates of recurrent shoulder instability of 0-18% with >5-year follow-up and 5-26% with >10-year follow-up [6,7].
Traditionally, the Latarjet procedure was only a salvage procedure in cases of significant glenoid bone loss and/or recurrent instability [8]. However, the indications of the Latarjet procedure have expanded as it is now regarded as a primary intervention for recurrent shoulder dislocation with glenoid bone loss in addition to being a treatment option for patients with recurrent shoulder dislocation with no glenoid bone defect and multidirectional instability after failed conservative treatment [2]. Furthermore, the Latarjet procedure has also even been proposed as a primary intervention after a first glenohumeral dislocation in the setting of no glenoid bone deficiency [9]. The surgical approach for a Latarjet procedure has also evolved beyond the traditional open deltopectoral approach, as some surgeons perform the surgery through a mini-open approach, an arthroscopically assisted approach, or an all-arthroscopic approach [3,9,10].
One of most critical steps of the Latarjet procedure is the proper positioning of the coracoid graft on the glenoid neck. If a coracoid graft is placed too lateral and thus overhanging, it can predispose to humeral head defects and arthritic change as well as limit internal rotation via humeral head-coracoid impingement [11,12]. If the graft is placed too medial, it can lead to recurrent instability [13,14]. A systematic review found that coracoid grafts placed medial to the glenoid subchondral bone had an average redislocation rate of 5.89% and an average instability rate of 9.17% compared to an average redislocation rate and instability rate of both 0.51% in coracoid grafts placed flush with the glenoid subchondral bone [15]. Moreover, a coracoid graft positioned too superior or too inferior to the glenoid equator may result in recurrent instability [13,16]. Therefore, substantial complications can result from coracoid graft malposition. In this review, we discuss the literature regarding coracoid graft positioning outcomes from various studies with respect to surgical approach amongst the open, mini-open, arthroscopically assisted, and all-arthroscopic approaches to the Latarjet procedure.
Where to Position the Coracoid Graft?
The ideal position of the coracoid graft is so that it is flush with glenoid subchondral bone in the axial plane. It is important to note that the coracoid graft is placed flush with the subchondral bone, as opposed to the glenoid cartilage itself. When the coracoid graft is placed flush with the glenoid subchondral bone, it allows fibrous cartilage to form on the graft during the healing process and then eventually be confluent with the native glenoid cartilage after healing. The coracoid graft must not be placed too medial to the glenoid subchondral bone, whereas to result in recurrent instability, as well as not too lateral, as to predispose to osteoarthritic changes [11-14]. In the sagittal plane, the coracoid graft should be placed inferior to or just at the glenoid equator, also described as 50% of the glenoid’s height. A coracoid graft positioned too inferior or too superior can result in recurrent instability [16].
While being flush and <1mm within the glenoid subchondral bone and the glenoid equator represents the ideal positioning, some stud have defined acceptable raiesnges. In the axial plane, Allain et al. [12] described the coracoid graft placement to be perfect when the graft was within 5mm of the glenoid subchondral bone rim medially and did not project onto the articular cartilage laterally. In the sagittal plane, Allain et al. [12] described the position to be perfect when the coracoid graft was at or just inferior to the glenoid equator. The glenoid can also be described as a clockface, in which subequatorial area would be 3 o’clock to 6 o’clock in right shoulders. On the other hand, Kany et al. [17] described a target range of -5mm to 3mm in reference to the subchondral glenoid bone rim in the axial plane. There is variability in the accepted tolerance range from author to author, but optimal position one strives for is flush with the subchondral glenoid bone rim in the axial plane and covering the subequatorial glenoid in the sagittal plane.
Traditionally, radiographs were used to assess coracoid graft position postoperatively, which include the anterior-posterior (AP) view, Bernageau’s view (glenoid profile view), and Lamy’s view (scapular Y view) [18]. However, some authors have found discrepancies between radiographs and computed tomography (CT) scans in assessing coracoid graft position. For instance, Doursounian et al. [11] found in their Latarjet procedure study that some of the coracoid grafts that appeared very close to the glenohumeral joint space on radiographs were actually quite distant from the glenohumeral joint on the CT scan.
Clavert et al. [18] analyzed the accuracy of radiographs in evaluating coracoid graft position by performing a cadaveric study comparing Bernageau’s radiographic view to CT scans. In their study, the authors performed a Latarjet procedure on a single cadaveric scapula using two slightly divergent screws for the coracoid transfer fixation. Then radiographs as well as a CT scan were performed to assess for coracoid graft position and screw position. The authors found that a space of ≤1mm could not be visible on Bernageau’s view, whereas the CT images could consistently provide an accurate assessment of bony contact. With regard to screw angle, the CT scan demonstrated a screw-glenoid surface angle of.02° for the inferior screw. The authors concluded 5.2° for the superior screw and 8.1° for the inferior screw. On the other hand, with Bernageau’s view, the mean angle was 1.6° ± 1.15° for the superior screw and 7.6° ± 3.02° that standard radiographs did not result in an accurate assessment of coracoid graft position or screw position. However, they also stated that radiographs do have utility postoperatively in providing a rough estimate of coracoid graft position, non-union or fracture of the coracoid graft, and an excessively medial screw position placing risk on the suprascapular nerve.
A CT scan represents a common and widely accepted method to assess coracoid graft position. Kraus et al. [19] described a reproducible method based off of CT scan analysis, which is commonly used by authors to assess coracoid graft positioning. The method begins by defining the glenoid height, which is obtained with the en face CT view of the glenoid. On this view, the most superior aspect and most inferior aspect of the glenoid are marked. Then a line connecting these two points is made, which represents the total glenoid height. Next, 25% and 50% of the glenoid height are marked (measuring from inferior to superior) and then the corresponding axial CT views at these respective levels are obtained. On each of these axial views, a tangential line is drawn connecting the anterior and posterior subchondral rims of the glenoid. The position of the coracoid graft is then judged as medial, flush, or lateral based off these tangential lines with a tolerance range of <1mm at the 25% and 50% glenoid height levels, respectively (Figure 1).
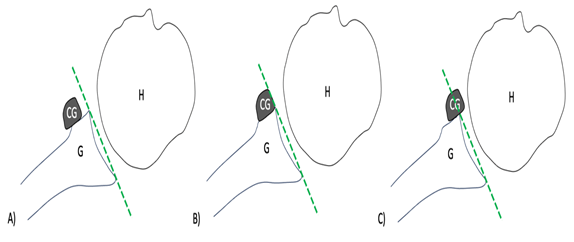
Figure 1: The position of the coracoid graft in relation to the tangential line connecting the anterior and posterior subchondral rims of the glenoid with the coracoid graft being A) medial, B) flush, and C) lateral. G = glenoid, H = humeral head, CG = coracoid graft.
Kraus et al. [19] also described a circumferential assessment, which is performed on the axial CT views at the 25% and 50% glenoid height levels. At each of these levels, a circle is drawn centered on the humeral head that encompasses all of the epiphysis and traverses in the glenohumeral joint midway between the glenoid and the humeral head’s articular surfaces. The coracoid graft can then be judged as lateral or not lateral with this metric. Using the tangential line and circumferential assessment methods at both the 25% and 50% glenoid height levels, the evaluator can classify the coracoid graft as 1) medial to the line (line only), 2) flush with the line (line only), 3) congruent (lateral to the line, but not the circle), and 4) lateral to both (line and circle).
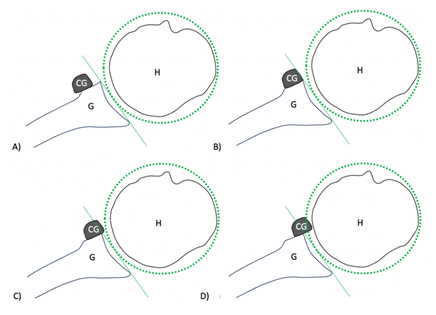
Figure 2: The position of the coracoid graft in relation to the tangential line and circumferential assessment with the coracoid graft being A) medial, B) flush, and C) congruent, and D) lateral. G = glenoid, H = humeral head, CG = coracoid graft.
Utilizing their described methods in 27 consecutive patients undergoing a Latarjet procedure, Kraus et al. [19] found the physicians initial evaluation and re-evalulation agreed 77.8% to 96.3% of the time and the intra-observer variability to range from “substantial” to “almost perfect.” The inter-observer agreement varied between 63.0% to 96.3% and the inter-observer variability ranged from “fair” to “almost perfect.” Kraus et al. [19] concluded that one can utilize their CT scan assessment method to accurately assess coracoid graft position in the axial plane with both satisfactory intra-observer and interobserver variability [20]. While other CT assessments have been described, many studies utilize Kraus et al.’s [19] method to evaluate coracoid graft position in this review.
Coracoid Graft Positioning with Respect to Surgical Approach
The Latarjet procedure can be performed through various approaches, each with their own set of advantages and disadvantages. We list literature reporting coracoid graft positioning outcomes with respect to the open, mini-open, mini-open arthroscopically assisted, and all-arthroscopic approaches to the Latarjet procedure below. The summary of these outcomes is depicted in Table 1.
|
Approach |
Study |
Axial Position |
Sagittal Position |
|
Open Approach |
Allain et al. [12] (n=58) |
“Perfect” = 24/58 (41.4%) Medial = 3/58 (5.2%) Lateral = 31/48 (53.4%) |
Subequatorial = 58/58 (100%) |
|
Doursounian et al. [11] (n=11) |
Flush = 8/11 (72.7%) Medial = 1/11 (9.1%) Lateral = 0/11 (0%) |
Subequatorial = 11/11 (100%) |
|
|
Schmid et al. [21] (n=41) |
Flush = 30/41 (73.2%) Medial = 6/41 (14.6%) Lateral = 5/41 (12.2%) |
N/A |
|
|
Neyton et al. [22] (n=37) |
Flush = 31/37 (83.8%) Medial = 1/37 (2.7%) Lateral = 1/37 (2.7%) |
Subequatorial = 33/37 (89.2%) |
|
|
Mizuno et al. [23] (n=68) |
Flush = 54/68 (79.4%) Medial = 5/68 (7.4%) Lateral = 9/68 (13.2%) |
N/A |
|
|
Minuesa-A. et al. [33] (n=10 cadavers) |
Flush = 10/10 (100%) Medial = 0/10 (0%) Lateral = 0/10 (0%) |
Subequatorial = 9/10 (90%) |
|
|
Zhu et al. [34] (n=44) |
Flush = 44/44 (100%) Medial = 0/44 (0%) Lateral = 0/44 (0%) |
Subequatorial = 44/44 (100%) |
|
|
Russo et al. [36] (n=21) |
Flush = 21/21 (100%) Medial = 0/21 (0%) Lateral = 0/21 (0%) |
Subequatorial = 21/21 (100%) |
|
|
Taverna et al. [40] (n=17) |
Flush = 13/17 (76.4%) |
Subequatorial = 4/17 (23.5%) |
|
|
Kordasiewicz et al. [37] (n=43) |
“Acceptable” = 80.5% |
“Acceptable” = 90.2% 2 to 5 o’clock = 87.8% |
|
|
Neyton et al. [38] (n=79) |
Avg. Distance = -0.9mm at 50% glenoid height Avg. Distance = -1.0mm at 25% glenoid height |
Avg % of graft subequatorial: 71% (95% CI, 67.3% to 74%) |
|
|
Randelli et al. [39] (n=1,053) |
Flush = 78% |
N/A |
|
|
Mini-Open Approach |
Meyer et al. [3] (n=12) |
Congruent = 11/12 (91.7%) Slight Lateral = 1/12 (8.3%) |
N/A |
|
Kraus et al. [19] (n=27) |
Flush = 16/27 (59.3%) Congruent = 6/27 (22.2%) Medial = 2/27 (7.4%) Lateral = 3/27 (11.1%) |
N/A |
|
|
Kraus et al. [25] (n=21) |
N/A |
Avg: 2:00h to 4:26h (R) Range: 1:05h to 5:33h (R) |
|
|
Lateur et al. [26] (n=40) |
Flush = 34/40 (84%) Medial = 2/40 (6%) Lateral = 4/40 (10%) |
N/A |
|
|
Mini-Open Arthroscopically Assisted Approach |
Taverna et al. [9] (n=60) |
Flush = 59/60 (98.3%) Medial = 0/60 (0%) Lateral = 0/60 (0%) *1 graft migrated superiorly at f/u |
Subequatorial = 58/60 (96.7%) Above Equator = 1/60 (1.7%) *1 graft migrated superiorly at f/u |
|
Taverna et al. [40] (n=22) |
Flush = 22/22 (100%) Medial = 0/22 (0%) Lateral = 0/22 (0%) |
Subequatorial = 16/22 (72.7%) Above Equator = 6/22 (27.3%) |
|
|
Nourissat et al. [27] (n=5 cadavers) |
Optimal = 4/5 (80%) Medial = 1/5 (20%) |
Avg: centered on 4 o’clock (R) |
|
|
All-Arthroscopic Approach |
Lafosse et al. [28] (n=180) |
Flush = 144/180 (80%) Medial = 14/180 (8%) Lateral = 22/180 (12%) |
3 to 5 o’clock = 78% Too Superior = 7% Too Inferior = 5% |
|
Casabianca et al. [4] (n=19) |
Flush = 32% Congruent = 38% Medial = 30% Too Medial = 6% Lateral = 0% |
Avg: 1:52h to 4:04h (R) |
|
|
Valencia et al. [29] (n=55) |
Flush = 45/55 (81.8%) Closed Position = 10/55 (18.2%) |
Avg % of graft subequatorial: 71.2 ± 21.8% |
|
|
Kany et al. [17] (n=95) |
Tangential Line: “Target Range” = 65/95 (68.4%) Medial = 7/95 (7.4%) Lateral = 23/95 (24.2%) Circumferential Line: “Target Range” = 77/95 (81.1%) Medial = 11/95 (11.6%) Lateral = 7/95 (7.4%) |
Subequatorial = 87/95 (91.5%) At Equator = 7/95 (7.3%) Above Equator = 1/95 (1.1%) |
|
|
Castricini et al. [30] (n=30) |
Flush = 23/30 (76.6%) Medial = 2/30 (6.7%) Lateral = 1/30 (3.3%) |
3 to 5 o’clock = 23/30 (76.6%) Too Superior = 2/30 (6.6%) Too Inferior = 1/30 (3.3%) |
|
|
Boileau et al. [31] (n=47) |
Flush = 43/47 (91.5%) Medial = 3/47 (6.4%) Lateral = 1/47 (2.1%) |
Subequatorial = 46/47 (97.9%) At Equator = 1/47 (2.1%) |
|
|
Boileau et al. [32] (n=70) |
Flush = 65/70 (92.9%) Medial = 2/70 (2.9%) Lateral = 3/70 (4.3%) |
Subequatorial = 63/70 (90%) Above Equator = 7/70 (10%) |
|
|
Minuesa-A et al. [33] (n=9 cadavers) |
Flush = 9/9 (100%) Medial = 0/9 (0%) Lateral = 0/9 (0%) |
Subequatorial = 4/9 (44.4%) |
|
|
Zhu et al. [34] (n=46) |
Flush = 44/46 (100%) Medial = 0/46 (0%) Lateral = 0/46 (0%) |
Subequatorial = 42/46 (91.3%) |
|
|
Russo et al. [36] (n=25) |
Flush = 24/25 (96%) Medial = 0/25 (0%) Lateral = 1/25 (4%) |
Subequatorial = 20/25 (80%) Above Equator = 5/25 (20%) |
|
|
Kordasiewicz et al. [37] (n=62) |
“Acceptable” = 78.4% |
“Acceptable” = 86.7% 2 to 5 o’clock = 56.7% |
|
|
Neyton et al. [38] (n screw =87) (n button = 42) |
Screw Fixation: Avg. Distance = 1.5mm at 50% glenoid height Avg. Distance = 0.3mm at 25% glenoid height EndoButton Fixation: Avg. Distance = 0mm at 50% glenoid height Avg. Distance = 0.7mm at 25% glenoid height |
Avg % of graft subequatorial: 55% (95% CI, 49% to 61%) Avg % of graft subequatorial: 82% (95% CI, 76% to 87%) |
|
|
Randelli et al. [39] (n=259) |
Flush = 87% |
N/A |
Table 1: The outcomes of coracoid graft position in the axial and sagittal planes categorized by Latarjet approach.
1. Open Approach
The Latarjet procedure is traditionally performed with an open deltopectoral approach, as was initially described by Latarjet and has since been adapted and modified [1,20].
Allain et al. [12] performed 58 open Latarjet procedures and assessed the coracoid graft using radiographs. The authors found that the graft was perfectly positioned in 24/58 (41.4%), too medial in 3/58 (5.2%), and too lateral in 31/48 (53.4%). With regards to cranial-caudal position, the coracoid graft was subequatorial or at the level of the glenoid equator in all 58/58 (100%) patients.
Doursunian et al. [11] reported on 11 open Latarjet procedures in which they assessed the coracoid graft position. Based on CT scan, 8/11 (72.7%) of the coracoid grafts were flush with the anterior-inferior subchondral glenoid rim and there was only 1/11 (9.1%) graft that was medial at 4mm. All 11/11 (100%) of the coracoid grafts were in a subequatorial position.
Schmid et al. [21] were able to assess the coracoid graft position during an open Latarjet procedure in 41 patients from their series. 30/41 (73.2%) were flush, 6/41 (14.6%) were medial, and 5/41 (12.2%) were lateral. Of note, in the 30 cases where the coracoid graft was placed flush, no new development of osteoarthritis was observed and the progression of the preexisting osteoarthritis was significantly less compared to the cases in which the graft was positioned too medial as well as compared to the cases where the graft was placed too lateral (p<0.001).
Neyton et al. [22] performed an open Latarjet procedure on 37 shoulders and reported that the coracoid graft was flush in 31/37 (83.8%), too medial in 1/37 (2.7%), and too lateral in 1/37 (2.7%). The coracoid graft was subequatorial in 33/37 (89.2%) of cases.
Mizuno et al. [23] conducted a retrospective review on 68 open Latarjet procedures and found that the coracoid graft was flush in 54/68 (79.4%) of patients, medial in 5/68 (7.4%) of patients, and lateral in 9/68 (13.2%) of patients.
2. Mini-Open Approach
Young et al. [24] amongst other authors have described a mini-open surgical technique, otherwise known as a limited deltopectoral approach, to perform the Latarjet procedure. In this mini-open surgical technique, the skin is incised 4-5cm from the tip of the coracoid extending towards the axillary fold. If cosmesis is desirable, a mere 3cm incision can be implemented.
Meyer et al. [3] conducted a Latarjet procedure utilizing a new drill guide in 12 patients through a mini-open approach. The authors found that the coracoid graft was congruent in 11/12 (91.7%) with only 1/12 (8.3%) coracoid graft being malpositioned in a slight lateral position according to the authors. Moreover, all coracoid grafts had <1mm discrepancy between the coracoid graft and glenoid rim in all patients.
Kraus et al. [19] also performed the Latarjet procedure through a mini-open approach in 27 patients. In the axial plane, the coracoid graft was flush in 16/27 (60%) of patients, congruent in 6/27 (22%) of patients, medial in 2/27 (7%) of patients, and lateral in 3/27 (11%) of patients. In a different study conducted by Kraus et al. [25], the authors performed a Latarjet procedure on 21 patients through a mini-open approach and found that the average location of the coracoid graft was between 2:00h to 4:26h (range, 1:05h to 5:33h) with respect to a right shoulder.
Finally, Lateur et al. [26] performed 40 Latarjet procedures through a mini-open approach. The authors found that the coracoid graft was flush in 84% of cases, medial in 6% of cases, and lateral in 10% of cases.
3. Mini-Open Arthroscopically Assisted Approach
Taverna et al. [9] described a novel Latarjet surgical technique in which they utilize both arthroscopy and an open approach, which they term “arthroscopically assisted.” In this approach, the authors utilize the open approach to harvest, prepare, and handle the coracoid graft, while using the arthroscopic approach to employ arthroscopic drill guides to accurately position and fixate the coracoid graft. Moreover, their technique has the advantage of avoiding the dangerous portals placed medial to the coracoid posing risk to neurovascular structures.
Taverna et al. [9] performed their technique in 60 patients and found that the coracoid graft was flush in 59/60 (98.3%) of patients, medial in 0/60 (0%) of patients, and lateral in 0/60 (0%) of patients. With regard to the cranial-caudal position, the coracoid graft was optimally at the equator or just subequatorial in 58/60 (96.7%) of patients and above the equator in 1/60 (1.7%) patient. There was 1 coracoid graft (1/60; 1.7%) that had migrated superiorly and was no longer flush at 1 year postoperatively when Taverna et al. recorded their results.
Nourissat et al. [27] also assessed the mini-open arthroscopically assisted approach in 5 cadaveric shoulders. Like Taverna et al. [9], the mini-open approach was utilized to harvest the coracoid graft and the arthroscopic portion of the procedure was used to position the coracoid graft. In all 3 right shoulder specimens, the coracoid graft was located at the 4 o’clock position. On the other hand, in the remaining 2 left shoulder specimens, the coracoid graft was located at the 8 o’clock position. With regards to the glenoid rim, the coracoid graft was in an optimal position in 4/5 (80%) cases, with 1/5 (20%) case being medial by 4mm. The average distance that the coracoid graft was medial to the glenoid rim was 1.4mm (range, 0 to 4mm). No lateral positioning of the coracoid graft occurred.
4. Arthroscopic Approach
Performing the Latarjet procedure through an all-arthroscopic approach was first described by Lafosse et al. [10] in 2007. The arthroscopic approach offers many advantages, which include the capability to assess for concomitant intraarticular pathology, a less invasive approach leading to less scar tissue formation and postoperative stiffness, and a quicker recovery. Moreover, many authors claim the arthroscopic approach allows improved visualization of the glenoid margin to allow a surgeon to accurately place the coracoid graft [32].
Lafosse et al. [28] published a subsequent study in 2010 reporting the outcomes of their described arthroscopic Latarjet technique in 180 patients. The authors found the coracoid graft was flush in 144/180 (80%) of patients, medial in 14/180 (8%) of patients, and was lateral in 22/180 (12%) of patients. The cranial-caudal placement was optimal between 3 to 5 o’clock in 78% of patients, too superior in 7% of patients, and too inferior in 5% of patients.
Casabianca et al. [4] performed an arthroscopic Latarjet procedure in 19 patients and found that in the axial view 32% of the coracoid grafts were flush, 38% were congruent, 30% were medial, 6% were too medial, and 0% were lateral. On the glenoid face, the coracoid grafts were placed from 01:52h (56° ± 14°) to 4:04h (122° ± 12.5°).
Valencia et al. [29] conducted 55 Latarjet procedures through an all-arthroscopic approach taking note of the coracoid graft position with respect to preoperative glenoid bone defect size. The authors found that coracoid grafts were flush in 45/55 (81.8%) of patients and 10/55 (18.2%) were defined as “closed” with respect to the angulation of the graft to the anterior glenoid rim. There were no coracoid grafts with an “open” angle to the glenoid rim. The average distance from the coracoid graft to the glenoid rim was 1.1 ± 2.19mm and 1.31 ± 2.05mm at 50% and 25% of the glenoid height, respectively. On average, 71.2 ± 21.8% of the total height of the coracoid graft was inferior to the glenoid equator and 44/55 (80%) of patients had more than 50% of the coracoid graft below the equator on average. When accounting for the amount of preoperative glenoid bone defect, patients with a glenoid bone defect did not significantly differ from patients without a glenoid bone defect in terms of axial position of the coracoid graft and if the graft was flush to the glenoid rim (p>0.05). However, there was a significant difference in regard to cranial-caudal position of the graft, as patients without a glenoid defect had a significantly less percentage of their coracoid graft below the equator (p=0.04).
Kany et al. [17] performed 105 arthroscopic Latarjet procedures and evaluated 95 of them with regard to coracoid graft position. With regard to cranial-caudal positioning, the coracoid grafts were subequatorial in 87/95 (91.5%) of patients, at the glenoid equator in 7/95 (7.3%) of patients, and above the equator in 1/95 (1%) patient. With the axial tangent circle evaluation, the axial view revealed the mean coracoid graft position was 0mm ± 4mm (range, -10 to 8mm) to the tangential line. Of the Latarjet procedures, 65/95 (68.4%) were positioned optimally within the author’s defined target range of -5mm to 3mm. 23/95 (24.2%) of patients had laterally positioned coracoid grafts, which in themselves had an average overhang of 5 ± 2mm (range, 3 to 8mm). 7/95 (7.4%) of patients had medial coracoid grafts, which in themselves had an average distance of -8 ± 1mm (range, -10 to -6mm) from tangential line. With the axial tangent circle evaluation, the average coracoid graft position was -1 ± 3mm (range, -11 to 6mm) to the tangential circle. 77/95 (81.1%) of the coracoid grafts were positioned within the target range, 7/95 (7.3%) were positioned laterally with a mean position of 4 ± 1mm (range, 3 to 6mm) within themselves, and 11/95 (11.6%) were positioned medial with a mean position of -7 ± 2mm (range, -11 to -6mm) within themselves. Finally, with the coronal tangent circle evaluation, the average coracoid graft position was -2 ± 4mm (range, -11 to 10mm) from the tangential circle. 70/95 (73.7%) of the coracoid grafts were positioned within the target range, 5/95 (5.4%) were positioned laterally with a mean position of 6 ± 3mm (range, 3 to 10mm) within themselves, and 20/95 (21.1%) were positioned medial with a mean position of -7 ± 1mm (range, -11 to -6mm) within themselves.
Castricini et al. [30] studied the learning curve of an arthroscopic Latarjet procedure in 30 patients. The authors found that the coracoid graft was flush and optimally position in the 3 to 5 o’clock position in 23/30 (76.6%) of patients. The coracoid graft was positioned medially in 2/30 (6.7%) of patients and laterally in 1/30 (3.3%) patient. The remaining patients experienced coracoid fractures.
As mentioned, an advantage of the arthroscopic approach is the capability to assess concomitant intraarticular pathology. Boileau et al. [31] utilized this advantage to modify to the standard Latarjet procedure, in which they performed a Latarjet procedure combined with an arthroscopic Bankart repair in 47 patients. A conversion to open surgery was needed in 6 patients early on in the study due to difficulty passing the coracoid graft through the subscapularis and/or fixing the graft to the glenoid neck. However, in all of these 6 open conversions, the procedure was finished arthroscopically by checking the position of the graft and performing the Bankart repair. With regard to the cranial-caudal position, the coracoid grafts were subequatorial in 46/47 (97.9%) of patients, 1/47 (2.1%) patient was at the equatorial glenoid line, and 0/47 (0%) of patients were superior to the glenoid equator. In the axial plane, the coracoid graft was flush in 43/47 (91.5%) of patients, 3/47 (6.4%) of patients were positioned too medial, and 1/47 (2.1%) patient was positioned too lateral.
Boileau et al. [32] conducted a subsequent study on 70 patients undergoing their combined arthroscopic Latarjet and Bankart repair technique. Utilizing radiographs, the authors reported that the coracoid graft was correctly subequatorial in 63/70 (90%) of patients, above the equator by 25% of the coracoid graft height in 7/90 (10%) of patients, and above the equator by 50% of the coracoid graft height in 0/90 (0%) of patients. Furthermore, the coracoid graft was correctly flush to the glenoid in 65/70 (93%) of patients, too medial by >5mm to the glenoid in 2/90 (3%) of patients, and too lateral by >5mm to the glenoid in 3/70 (4%) of patients.
5. Studies Comparing The Approaches
In studies comparing the Latarjet approaches, the literature remains a debate on if one approach leads to better coracoid graft positioning.
Minuesa-Asensio et al. [33] assessed the coracoid graft placement in the Latarjet procedure between the arthroscopic approach and the open approach in 19 cadaveric shoulders. The authors found that all of the coracoid grafts were placed flush with the glenoid in both the open and arthroscopic groups. There was no significant difference in the axial position of the coracoid grafts between the groups (p=0.243); however, there was a tendency to position the coracoid grafts slightly lateral in the open group with a mean distance of 1.1mm lateral to the glenoid rim (range, -0.07 to 1.6mm) compared to the arthroscopic group with an average of -1.67mm (range, -2.8 to 2.24mm). With respect to the cranial-caudal position of the coracoid graft, Minuesa-Asensio et al. [33] reported that 9/10 (90%) of the coracoid grafts were placed in the optimal subequatorial position in the open group, whereas 4/9 (44.4%) were placed in an optimal position in the arthroscopic group (p>0.05). Finally, with regard to the major axes along the glenoid and coracoid graft, Minuesa-Asensio et al. [33] found the coracoid grafts with the arthroscopic group were placed at a significantly increased angle of inclination with an average of 15.1° (range, 9.5° to 21.5°) compared to the open group with an average angle of 3.8° (range, 1° to 8°) (p=0.001).
Zhu et al. [34] performed 44 open and 46 arthroscopic Latarjet procedures and found that coracoid graft was at the level of the subchondral glenoid rim in all patients regardless of an open approach or an arthroscopic approach. There were no medial or laterally placed grafts. However, there was a significant difference with regard to subequatorial position, as the open approach resulted in all 44/44 grafts (100%) placed inferior to the equator, whereas only 42/46 grafts (91.3%) in the arthroscopic approach were placed below the equator (p<0.001).
Marion et al. [35] conducted the Latarjet procedure with an mini-open approach on 22 patients and with an arthroscopic approach on 36 patients. They found the arthroscopic approach resulted in a more lateral coracoid graft (p<0.04), but a better subequatorial position (p=0.02) than the mini-open approach.
Russo et al. [36] conducted 21 open and 25 arthroscopic Latarjet procedures and reported that the arthroscopic approach resulted in 24/25 (96%) flush coracoid grafts with 1 coracoid graft being too proud laterally (4%). In the sagittal plane, the coracoid graft was subequatorial in 20/25 cases (80%) and breached the equatorial line in 5/25 cases (20%). Overall, the arthroscopic approach resulted in 19/25 cases (76%) that were properly positioned flush and subequatorial with the glenoid. On the other hand, the open approach resulted in flush and subequatorial positioning of the coracoid graft in all 21/21 cases (100%) and there was a significant difference between the arthroscopic approach and the open approach in the sagittal plane regarding subequatorial position (p=0.025).
Kordasiewicz et al. [37] postoperatively examined 43 open and 62 arthroscopic Latarjet procedures and discovered that in the axial view the arthroscopic group had 78.4% of coracoid grafts placed in the acceptable position, while the open group had 80.5% placed in the acceptable position (p<0.05). In the sagittal plane, the coracoid graft was in the acceptable position between the 2 and 5 o’clock position in 86.7% of patients in the arthroscopic group versus 90.2% of patients in the open group (p>0.05). However, when the criteria was restricted to between the 2 and 5 o’clock position in the sagittal plane, 56.7% of patients in the arthroscopic group versus 87.8% of patients in the open group were in an acceptable position (p<0.05).
Neyton et al. [38] retrospectively assessed 208 Latarjet procedures with 79 treated with an open approach and 129 treated arthroscopically. The arthroscopic procedures were separated into two groups based on the type of coracoid graft fixation, with 87 patients receiving screw fixation and 42 patients receiving an EndoButton fixation. In the axial plane at 50% of the glenoid height, the average position of the coracoid graft was -0.9mm (95% CI, -1.4 to 0.5mm) in the open group, 1.5mm (95% CI, -0.9 to 2.1mm) in the screw fixation group, and 0mm (95% CI, -0.6 to 0.6mm) in the Endobutton fixation group. The axial positioning at 50% of the glenoid height was significantly different between the open group versus both the arthroscopic groups (p<0.0001). However, there was no significant difference between the two arthroscopic fixation groups (p>0.05). In the axial plane at 25% of the height of the glenoid, the average position of the coracoid graft was -1.0mm (95% CI, -7.0 to 3.8mm) in the open group, 0.3mm (95% CI, -0.2 to 0.9mm) in the screw fixation group, and 0.7mm (95% CI, -0.4 to 0.2mm) in the Endobutton fixation group. Again, the axial positioning was significantly different between the open group versus both the arthroscopic groups (p<0.001). However, there was no significant difference between the two arthroscopic fixation groups (p>0.05). Finally, with regard to cranial-caudal positioning of the coracoid graft, the average position of the coracoid graft with regard to its own height below the glenoid equator was 71% in the open group (95% CI, 67.3% to 74%), 55% in the screw fixation group (95% CI, 49% to 61%), and 82% in the EndoButton fixation group (95% CI, 76% to 87%). The open group’s cranial-caudal coracoid graft’s position was significantly different than both the arthroscopic groups (p<0.001). Moreover, the cranial-caudal coracoid graft position was also significantly different between the two arthroscopic groups themselves (p<0.001).
Randelli et al. [39] conducted a systematic review comparing the Latarjet procedure done with an open approach versus an arthroscopic approach. The authors included 23 articles with a total of 1,317 Latarjet procedures (1,058 open, 259 arthroscopic). The authors found that the coracoid graft was flush in 87% of the procedures in the arthroscopic group versus 78% in the open group (p>0.05).
Taverna et al. [40] conducted their described mini-open arthroscopically assisted Latarjet procedure in 22 patients and compared it to 17 Latarjet procedures with an open approach. The authors found the coracoid graft was placed properly in line with the glenoid rim in all 22/22 (100%) of the arthroscopic-assisted approach patients compared to 13/17 (76.4%) of the open approach patients. The average articular step off in the arthroscopic group was 1.6mm (range, 0 to 7mm) with 64.7% of the procedures having <1mm articular step off. On the other hand, the average articular step off in the open group was 1.6mm (range, 0 to 8mm) with 50% of the procedures having <1mm step off. With regard to cranial-caudal positioning, the coracoid graft was optimally subequatorial in 16/22 (72.7%) of patients in the arthroscopic group compared to only 4/17 (23/5%) of patients in the open group.
Conclusion
The positioning of the coracoid graft during the Latarjet procedure remains one of the most important steps of the surgery. The Latarjet procedure can be performed through either an open, mini-open, mini-open arthroscopically assisted, or all-arthroscopic approach. The coracoid graft positioning postoperatively can be assessed with described methods on a CT scan. All approaches can lead to satisfactory coracoid graft placement with recent studies. No matter what Latarjet approach is employed, one must ensure coracoid graft placement is accurate to achieve optimal patient outcomes.
References
- Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chirurgical 49 (1954): 994-7.
- Shin, SJ, Kim JH, Ahn J. Arthroscopic Latarjet procedure: current concepts and surgical techniques.Clin Shoulder Elb (2023).
- Meyer DC, Moor BK, Gerber C, Ek ET. Accurate coracoid graft placement through use of a drill guide for the Latarjet procedure. J Shoulder Elbow Surg 22 (2013): 701-708.
- Casabianca L, Gerometta A, Massein A, et al. Graft position and fusion rate following arthroscopic Latarjet. Knee Surg Sports Traumatol Arthrosc 24 (2016): 507-512.
- Yamamoto N, Muraki T, An KN, et al. The stabilizing mechanism of the Latarjet procedure: a cadaveric study. J Bone Joint Surg Am 95 (2013):1390-1397.
- Calvo E, Valencia M, Foruria AM, et al. Recurrence of instability after Latarjet procedure: causes, results and treatment algorithm. EFORT Open Rev 7 (2022): 800-807.
- Gilat R, Lavoie-Gagne O, Haunschild ED, et al. Outcomes of the Latarjet procedure with minimum 5-and 10-year follow-up: a systematic review. Shoulder Elbow 12 (2020): 315-329.
- Shah AA, Butler RB, Romanowski J, et al. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 94 (2012): 495-501.
- Taverna E, Longo UG, Guarrella V, et al. A new mini-open technique of arthroscopically assisted Latarjet. BMC Musculoskelet Disord 21 (2020): 1-2.
- Lafosse L, Lejeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy 23 (2007): 1242-e1.
- Doursounian L, Debet-Mejean A, Chetboun A, et al. Bristow-Latarjet procedure with specific instrumentation: study of 34 cases. Int Orthop 33 (2009): 1031-1036.
- Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 80 (1998): 841-852.
- Hovelius L, Körner L, Lundberg B, et al. The coracoid transfer for recurrent dislocation of the shoulder. Technical aspects of the Bristow-Latarjet procedure. J Bone Joint Surg Am 65 (1983): 926-934.
- Huguet D, Pietu G, Bresson C, et al. Anterior instability of the shoulder in athletes: apropos of 51 cases of stabilization using the Latarjet-Patte intervention. Acta Orthop Belg 62 (1996): 200-206.
- Cowling PD, Akhtar MA, Liow RY. What is a Bristow-Latarjet procedure?: A review of the described operative techniques and outcomes. Bone Joint J 98 (2016): 1208-1214.
- Barth J, Neyton L, Métais P, et al. Is the two-dimensional computed tomography scan analysis reliable for coracoid graft positioning in Latarjet procedures?. J Shoulder Elbow Surg 26 (2017): e237-e242.
- Kany J, Flamand O, Grimberg J, et al. Arthroscopic Latarjet procedure: is optimal positioning of the bone block and screws possible? A prospective computed tomography scan analysis. J Shoulder Elbow Surg 25 (2016): 69-77.
- Clavert P, Koch G, Neyton L, et al. Is anterior glenoid bone block position reliably assessed by standard radiography? A cadaver study. Orthop Traumatol Surg Res 102 (2016): S281-S285.
- Kraus TM, Graveleau N, Bohu Y, et al. Coracoid graft positioning in the Latarjet procedure. Knee Surg Sports Traumatol Arthrosc (2016): 496-501.
- Edwards TB, Walch G. The Latarjet procedure for recurrent anterior shoulder instability: rationale and technique. Oper Tech Sports Med 10 (2002): 25-32.
- Schmid SL, Farshad M, Catanzaro S, et al. The Latarjet procedure for the treatment of recurrence of anterior instability of the shoulder after operative repair: a retrospective case series of forty-nine consecutive patients. J Bone Joint Surg Am 94 (2012): e75.
- Neyton L, Young A, Dawidziak B, et al. Surgical treatment of anterior instability in rugby union players: clinical and radiographic results of the Latarjet-Patte procedure with minimum 5-year follow-up. J Shoulder Elbow Surg 21 (2012): 1721-1727.
- Mizuno N, Denard PJ, Raiss P, et al. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 23 (2014): 1691-1699.
- Young AA, Maia R, Berhouet J, et al. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg 20 (2011): S61-S69.
- Kraus TM, Martetschläger F, Graveleau N, et al. CT-based quantitative assessment of the surface size and en-face position of the coracoid block post-Latarjet procedure. Arch Orthop Trauma Surg 133 (2013): 1543-1548.
- Lateur G, Pailhe R, Refaie R, et al. Results of the Latarjet coracoid bone block procedure performed by mini invasive approach. Int Orthop 42 (2018): 2397-2402.
- Nourissat G, Nedellec G, O’Sullivan NA, et al. Mini-open arthroscopically assisted Bristow-Latarjet procedure for the treatment of patients with anterior shoulder instability: a cadaver study. Arthroscopy: Arthoscopy 22 (2006): 1113-1118.
- Lafosse L, Boyle S. Arthroscopic latarjet procedure. J Shoulder Elbow Surg 19 (2010): 2-12.
- Valencia M, Rivas UN, Calvo C, et al. Does preoperative glenoid bony defect determine final coracoid graft positioning in arthroscopic Latarjet?. JSES Int 7 (2023): 393-398.
- Castricini R, De Benedetto M, Orlando N, et al. Arthroscopic Latarjet procedure: analysis of the learning curve. Musculoskelet Surg 97 (2013): 93-98.
- Boileau P, Mercier N, Roussanne Y, et al. Arthroscopic Bankart-Bristow-Latarjet procedure: the development and early results of a safe and reproducible technique. Arthroscopy 26 (2010): 1434-1450.
- Boileau P, Thélu CÉ, Mercier N, et al. Arthroscopic Bristow-Latarjet combined with Bankart repair restores shoulder stability in patients with glenoid bone loss. Clin Orthop Relat Res 472 (2014): 2413-2424.
- Minuesa-Asensio A, García-Esteo F, Merida-Velasco JR, et al. Comparison of coracoid graft position and fixation in the open versus arthroscopic Latarjet techniques: a cadaveric study. Am J Sports Med 48 (2020): 2105-2114.
- Zhu Y, Jiang C, Song G. Arthroscopic versus open Latarjet in the treatment of recurrent anterior shoulder dislocation with marked glenoid bone loss: a prospective comparative study. Am J Sports Med 45 (2017): 1645-1653.
- Marion B, Klouche S, Deranlot J, et al. A prospective comparative study of arthroscopic versus mini-open Latarjet procedure with a minimum 2-year follow-up. Arthroscopy 33 (2017): 269-277.
- Russo A, Grasso A, Arrighi A, et al. Accuracy of coracoid bone graft placement: open versus arthroscopic Latarjet. Joints 5 (2017): 85-88.
- Kordasiewicz B, Kicinski M, Ma?achowski K, et al. Comparative study of open and arthroscopic coracoid transfer for shoulder anterior instability (Latarjet)—computed tomography evaluation at a short term follow-up. Part II. Int Orthop 42 (2018): 1119-1128.
- Neyton L, Barth J, Nourissat G, et al. Arthroscopic Latarjet techniques: graft and fixation positioning assessed with 2-dimensional computed tomography is not equivalent with standard open technique. Arthroscopy 34 (2018): 2032-2040.
- Randelli P, Fossati C, Stoppani C, et al. Open Latarjet versus arthroscopic Latarjet: clinical results and cost analysis. Knee Surg Sports Traumatol Arthrosc 24 (2016): 526-532.
- Taverna E, Guarrella V, Cartolari R, et al. Arthroscopically-assisted Latarjet: an easy and reproducible technique for improving the accuracy of graft and screw placement. Shoulder Elbow 10 (2018): 99-106.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 