Platelet-Rich Fibrin in Combination with Heat Coagulated Albumin Gel as Treatment for Lateral Epicondylitis, A Retrospective 1-Year Follow-Up Study
Torbjörn Ogéus DC, PgD, MSc, ScA*
Stockholms led- & smärtklinik, 11424, Stockholm, Sweden
*Corresponding Author: Torbjörn Ogéus, Stockholms led- & smärtklinik, 11424, Stockholm, Sweden.
Received: 27 September 2024; Accepted: 04 October 2024; Published: 14 October 2024
Article Information
Citation: Torbjörn Ogéus. Platelet-Rich Fibrin in Combination with Heat Coagulated Albumin Gel as Treatment for Lateral Epicondylitis, A Retrospective 1-Year Follow-Up Study. Journal of Orthopedics and Sports Medicine. 6 (2024): 219-226.
View / Download Pdf Share at FacebookAbstract
Introduction: Lateral epicondylitis (LE), commonly known as tennis elbow, is one of the most frequent causes of elbow pain, primarily affecting the tendons that attach to the lateral epicondyle of the humerus. It is particularly associated with repetitive overuse of the wrist extensor muscles, especially the extensor carpi radialis brevis (ECRB). Despite the condition's name, tennis elbow is not limited to athletes, with a significant prevalence in occupations and activities involving repetitive wrist extension and forearm movements, such as manual laborers, office workers, and musicians. The condition is characterized by localized pain over the lateral epicondyle, which may radiate down the forearm and worsen with wrist extension or gripping actions. Lateral epicondylitis can be debilitating, affecting daily activities and work performance, and its management continues to be a challenge, especially in chronic cases resistant to conventional treatments.
Methods: This is a retrospective database cohort study. The clinic database was searched for patients that had undergone PRF and ALB-PRF treatment for LE between January 2019 and August 2023. 528 patients were included in the study. The analyzed data were 1-year follow-up NRS scores of multiple clinical tests and sonographic pictures before the treatment, 1 month after, 3 months after and 12 months after the treatment.
Results: Statistically significant positive changes on NRS scores (p=0,0001) were presented for all measured clinical outcomes. Sonographic positive changes were also presented; a mean decrease of focal hypoechoic changes of 3 mm (p = 0,0001).
Conclusion: In conclusion, PRF combined with ALB-PRF is an effective treatment for clinically diagnosed lateral epicondylitis. Significantly lowered NRS pain scores in clinical and orthopedic tests as well as significant positive changes in sonographic pictures 3 months after the treatment combined with 1 year-follow up data indicates significant longterm effects.
Keywords
<p>PRF; ALB-PRF; Lateral epicondylitis; Sonography; Regenerative medicine</p>
Article Details
1. Introduction
Lateral epicondylitis (LE), commonly known as tennis elbow, is one of the most frequent causes of elbow pain, primarily affecting the tendons that attach to the lateral epicondyle of the humerus. It is particularly associated with repetitive overuse of the wrist extensor muscles, especially the extensor carpi radialis brevis (ECRB). Despite the condition's name, tennis elbow is not limited to athletes, with a significant prevalence in occupations and activities involving repetitive wrist extension and forearm movements, such as manual laborers, office workers, and musicians. The condition is characterized by localized pain over the lateral epicondyle, which may radiate down the forearm and worsen with wrist extension or gripping actions. Lateral epicondylitis can be debilitating, affecting daily activities and work performance, and its management continues to be a challenge, especially in chronic cases resistant to conventional treatments.
Lateral epicondylitis is typically initiated by microtrauma to the ECRB tendon, leading to degeneration rather than inflammation. Studies have shown that LE is primarily a degenerative condition, where repeated stress causes microtears in the tendon, leading to a failed healing response. This process is known as tendinosis, which involves disorganized collagen fibers, increased vascularity, and mucoid degeneration in the tendon. Histopathological studies have demonstrated the presence of fibroblasts, vascular hyperplasia, and disorganized collagen, with little evidence of inflammatory cells, thus distinguishing lateral epicondylitis from true tendinitis, which involves inflammation [1]. As a result, lateral epicondylitis is best described as an angiofibroblastic tendinosis, a chronic degeneration of the tendon rather than an acute inflammatory process.
The pain associated with lateral epicondylitis is thought to arise from a combination of mechanical overloading of the tendon and changes in the nociceptive pathways within the peripheral and central nervous systems. Repetitive microtrauma can lead to nociceptive sensitization, which may contribute to the persistence of pain even after the initial tendon injury has healed. This chronic pain state can be particularly difficult to manage and is often resistant to standard treatment modalities.
The management of lateral epicondylitis typically begins with conservative approaches, aimed at reducing pain and improving tendon function. First-line treatments include rest, activity modification, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy. Physical therapy plays a crucial role, with eccentric strengthening exercises being the cornerstone of tendon rehabilitation. These exercises promote collagen remodeling, improve tendon strength, and enhance functional outcomes [2]. Bracing and orthotics, such as counterforce braces or wrist splints, may also be used to offload the affected tendon and reduce strain during activities.
Corticosteroid injections are frequently used for short-term pain relief, but their long-term efficacy is questionable. Although they might provide significant pain relief in the short term, several studies have shown that corticosteroids may delay tendon healing and lead to poorer long-term outcomes [3]. Furthermore, repeated corticosteroid injections may weaken the tendon and increase the risk of rupture.
More recently, there has been growing interest in biologic therapies, such as platelet-rich plasma (PRP) and platelet-rich fibrin (PRF), which aim to enhance the body's natural healing mechanisms. These treatments are particularly appealing for chronic cases of lateral epicondylitis that have failed to respond to conservative therapies. Unlike traditional pharmacological or surgical interventions, biologics harness the body's own growth factors to promote tissue regeneration, offering a potentially more effective and less invasive treatment option.
Platelet-rich fibrin (PRF) represents a second-generation platelet concentrate, derived from the patient’s own blood, that has gained increasing attention in the treatment of musculoskeletal injuries, including lateral epicondylitis. PRF is an autologous blood product that is rich in platelets, leukocytes, and fibrin, which collectively release a host of growth factors and cytokines essential for tissue healing and regeneration. Unlike platelet-rich plasma (PRP), which requires anticoagulants during preparation, PRF is prepared without the addition of exogenous agents, resulting in a more natural, fibrin-rich matrix that supports sustained release of growth factors over time [4].
The key growth factors present in PRF include transforming growth factor-beta (TGF-β), platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), and epidermal growth factor (EGF), all of which play vital roles in tissue repair. These growth factors promote collagen synthesis, angiogenesis, and cellular proliferation, which are critical for tendon healing [5]. In addition, PRF contains leukocytes, which contribute to its immunomodulatory properties, potentially reducing chronic inflammation and promoting a more favorable healing environment in degenerative tendon conditions like lateral epicondylitis.
To our knowledge, no conclusive evidence regarding LE treatment recommendations have been published yet.
This study presents 1-year follow-up data from 528 patients who were clinically diagnosed with lateral epicondylitis verified with ultrasound examination and sheds light on the regenerative potential of PRF combined with ALB-PRF in the treatment thereof.
2. Materials and Method
Various types of autologous platelet concentration protocols have been proposed to be used to treat tendon injuries. Some studies have indicated a positive effect on pain and other symptoms however, the effect of injected platelets in the injury might require multiple injections and no standard protocols exist [6]. One way of extending the effect of the injected platelets is to heat a liquid platelet-poor plasma (PPP) layer, the resorption properties of heated albumin (albumin gel) can thereby be extended from 2 weeks to greater than 4 months (ALB-PRF) [7].
PRF’s therapeutic potential in lateral epicondylitis lies in its ability to enhance the natural healing process of tendons, which is often impaired in chronic tendinopathies. The fibrin matrix formed during PRF preparation acts as a scaffold, supporting cell migration and proliferation while gradually releasing growth factors over time. This scaffold provides a favorable microenvironment for tendon healing by facilitating the recruitment of fibroblasts and other reparative cells to the site of injury [8]. These cells play a crucial role in synthesizing new collagen fibers, which are essential for restoring tendon integrity.
In addition to promoting tissue regeneration, PRF may also modulate inflammation in tendinopathies. Chronic tendinopathies are often associated with low-grade, persistent inflammation, which contributes to pain and tissue degeneration. The leukocytes present in PRF release anti-inflammatory cytokines, which can help reduce this chronic inflammation and promote a shift towards tissue repair. Furthermore, PRF has been shown to increase the expression of genes involved in tissue repair and collagen production, further supporting its role in enhancing tendon regeneration [9].
2.1 Preparation of PRF and ALB-PRF
All patients that underwent PRF and ALB-PRF treatment of lateral epicondylitis at the clinic during the reported time frame received the same treatment protocol:
20ml blood was collected from the patients before each of the PRF injections. Two10ml Plastic, round-bottomed vacuum tubes (Liquid PRF tubes) were used to collect the blood, after collection, the tubes were spun on a horizontal swing-out bucket rotors centrifuge system. Two different PRF protocols were utilized in the treatments, the first injection consisted of a combination of Liquid-PRF (L-PRF) and Concentrated-PRF (C-PRF) protocol where two separate centrifugations, the first 300xg for 5 min where one of the tubes were removed and a second centrifugation consisted of a modified C-PRF where the last tube was spun at 2000xg for 4 min. After the second spin the two different protocols where combined in a mixture of L-PRF and a modified C-PRF for the first injection. The second injection consisted of a Heat-Coagulated Albumin Gel -PRF (ALB-PRF) protocol of 2000xg for 8 min followed by a heating and cooling down process before the injection was performed. The two protocols were utilized following international guidelines for PRF preparation published by Miron et al in 2019 [10] (except for the modified C-PRF protocol).
The PRF injection consisted of mixture of L-PRF and a modified C-PRF [11] injection of 2ml, centrifuged at 300xg for 5 min and 2000xg for 4 min. The ALB-PRF injection that was given was 3ml ALB-PRF, 2000xg for 8 min on a horizontal centrifuge, the albumin layer was heated according to the ALB-PRF protocol; 75 degrees for 10 min [12]. In the last step, the heat- coagulated albumin gel was cooled down to room temperature and mixed with the remaining C-PRF to create ALB-PRF. The centrifuge utilized in all PRF treatments was the Bio-PRF horizontal centrifuge (Bio-PRF, USA).
2.2 Administration of PRF and ALB-PRF
The patients underwent two tendon injections, one L-PRF combined with modified C-PRF and one ALB-PRF injection. In the first week one injection of L-PRF combined with modified C-PRF. In the following week one ALB-PRF injection was performed. All tendon injections were performed with ultrasound guidance to ensure needle placement in the injured area in the attachment site for the ECRB muscle in the lateral epicondyle.
5 days after the last injection, all patients received a simple rehabilitation program consisting of light stretching of the extensor musculature of the forearm and excentric strength training for the same muscles with a slow progression of resistance.
2.3 Study design
This is a retrospective database cohort study. The clinic database was searched for patients that had undergone PRF combined with ALB-PRF treatment for lateral epicondylitis between January 2019 and August 2023.
According to the Ethics Commission of Stockholm, Sweden, retrospective database-based studies do not require ethical approval and patient informed consent whenever the data were acquired, saved and treated anonymously. This applies to the present study.
2.4 Subjects
576 patients (289 female and 287 male) underwent PRF combined with ALB-PRF treatment for lateral epicondylitis at the clinic during the above-referred period.
On the first day of treatment, patients were informed about the data collection that routinely takes place in the clinic and were asked to give written consent for data collection. With patient's consent, all patients were asked to report their perceived pain during the clinical tests, before the treatment started, after 1 month, 3 months and after 1 year. Sonographic pictures were taken on all treated joints before the treatment after 1 months and after 3 months.
The patients were included if they were treated with PRF and ALB-PRF treatment of their elbow and the follow-up data was available. The patients were excluded in case all pain assessment data was not available or if they failed to follow the instructions of rehabilitation or missed their follow-up visits.
The inclusion criteria were met by 528 patients (270 female and 258 male) that were treated for lateral epicondylitis with PRF and ALB-PRF.
2.5 Sonographic database
During the treatment protocol, sonographic (ultrasound) pictures of the affected elbow were taken before the treatment, 1 month after, 3 months after the treatment and 12 months after the treatment. The focal area of the lateral epicondyle and specifically the echogenic/hypoechoic (darker) areas were measured digitally in millimeter (mm) and compared on the before and after pictures and later added to the data file for each corresponding patient for easy database access. The most common finding in a patient with LE is focal areas of low echogenicity with a background of intrinsic tendinopathy, in 25% of the cases calcifications are seen [13].
2.6 The instruments
The Numerical Rating Scale (NRS) evaluates perceived pain on a segmented numerical scale with 11 points ranging from 0 to 10 [14] and can be used in combination with orthopedic tests for more exact measurements.
Cozen’s test (often referred to as “tennis elbow test”) is a standardized orthopedic test for measuring lateral epicondylitis clinically. It is performed by resisted wrist extension against pressure applied by the examiner [15].
Maudsley’s test (or Maudsley's middle finger test) is another standardized orthopedic test where the examiner resists extension of the 3rd digit of the hand, stressing the extensor digitorum muscle and tendon [16].
Mill’s test (often referred to as “pain palpation test”) is a clinical test where the clinician palpates the patient’s lateral epicondyle with one hand while pronating the patient’s forearm, fully flexing the wrist, the elbow extended [17].
Finally, the extensor grip test (also referred to as “grip strength”) was used to evaluate the patient’s pain level. In the test the patient is asked to hold the hand of the examiner as they would during a handshake and squeeze the hand [18].
During all the above mentioned orthopedic and clinical tests the patients were instructed to report the corresponding NRS score perceived for data collection.
2.7 Statistical analysis
Mean and standard deviation (SD) or frequencies (percentage) were used to characterize the sample. The normal distribution of the data was tested with the use of T-test and ANOVA tests. Demographic data comparisons between the groups left and right elbow were performed based on data gathered before the treatment series with the use of t-tests for independent samples.
To investigate whether there were significant differences in the mean NRS scores of patient’s multiple comparisons between the pairs of means were performed with t-tests and ANOVA for independent samples.
All statistical tests were performed with Prism 10 for Windows (Microsoft, USA). For all statistical tests, the 0.05 level of probability was set as the criterion for statistical significance.
3. Results
The data of the 528 patients that met the inclusion criteria were analyzed. The patients in the sample were on average 44.44 ± 2.81 years old. There were no significant differences between the patients in the different test groups (left and right elbow) concerning their mean age (p = 0,89). The distribution of male and female patients was not significantly different (p = 0.34) (the demographic data can be seen in Figure 1).
3.1 Cozen’s test scores
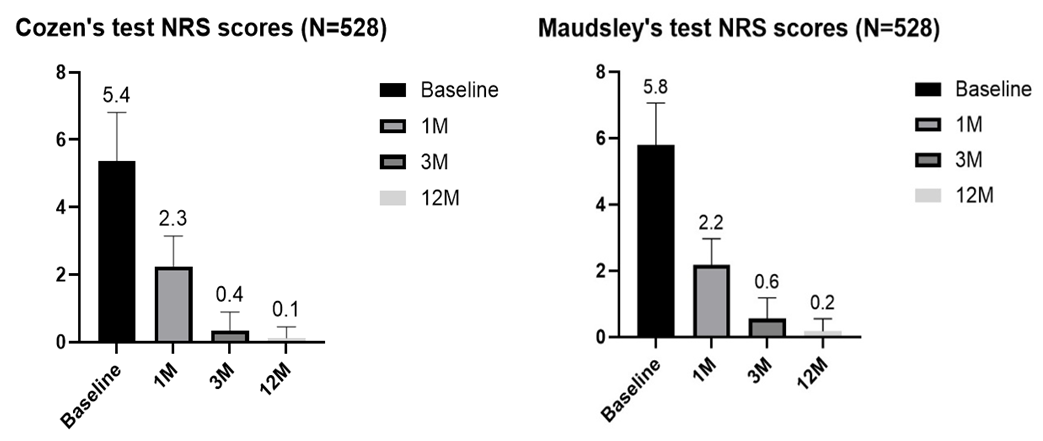
The treated patients (n=528) were analyzed using an ANOVA test and showed a significant improvement in NRS score (p = 0,0002) with a mean change from 5.4 on the baseline measurement, 2.3 on the 1-month follow-up, 0,4 on the 3-month follow-up and 0.1 on the 1-year follow-up (98,1% decrease in total).
3.2 Maudsley’s test scores
The treated patients (n=528) were also analyzed using an ANOVA test and showed a similar positive change in NRS score (p = 0,0001) with a mean change from 5.8 on the baseline measurement, 2.2 on the 1-month follow-up, 0,6 on the 3-month follow-up and 0.2 on the 1-year follow-up (96,5% decrease in total) (changes can be seen in Figure 2).
3.3 Mill’s test scores
The treated patients (n=528) were also analyzed using an ANOVA test and once again showed a similar positive change in NRS score (p = 0,0001) with a mean change from 6.0 on the baseline measurement, 2.5 on the 1-month follow-up, 0.5 on the 3-month follow-up and 0.2 on the 1-year follow-up (96,6% decrease in total) (changes can be seen in Figure 3).
3.4 Extensor grip test scores
The treated patients (n=528) were again analyzed using an ANOVA test and showed a similar positive change in NRS score (p = 0,0001) with a mean change from 5.0 on the baseline measurement, 1.9 on the 1-month follow-up, 0,4 on the 3-month follow-up and 0.1 on the 1-year follow-up (98,0% decrease in total) (changes can be seen in Figure 3).
There were no statistically significant differences between the genders in any of the analyzed tests. A final analysis of the combined NRS data of the different pain tests was performed to determine the total combined changes in all the treated patients. A combined statistically significant (p = 0,0001) improvement of 97,0% was seen (with a mean change of 5.7 to 0.1 at the 12-month follow-up) (changes can be seen in Figure 4).
3.5 Sonographic data
The radiographic data of the 528 patients that met the inclusion criteria were analyzed with a two-tailed unpaired T-test and compared, before- treatment after one months, 3 months and 12 months after the treatment.
The patients showed a statistically significant decrease in hypoechoic areas in the lateral epicondyle that was examined from an average of 3mm wide to an average of near zero visibility according to sonographic picture analysis (p = 0,0001) (changes can be seen in Figure 5).
Examples of the described sonographic changes, such as hypoechoic focal changes and calcifications at the tendon attachment in the lateral epicondyle can be seen in Figure 6.
Figure 6: Sonographic pictures of treated lateral epicondylitis, before and 3 Months after the PRF and ALB-PRF treatment. A) Mean change from 6 mm hypoechoic area to zero B) Mean change from 2 mm hypoechoic area to zero (a minor calcification can be seen in the baseline picture) C) Mean change from 2mm hypoechoic area to zero (a 2mm calcification can be seen on the baseline picture D) Mean change from 5mm hypoechoic area to zero.
4. Discussion
While the use of PRF in lateral epicondylitis is still relatively new, early clinical studies demonstrated promising results. Several trials have shown that PRF might significantly reduce pain and improve functional outcomes in patients with chronic lateral epicondylitis who have failed to respond to conservative treatments. In one prospective study, patients treated with PRF experienced a significant reduction in pain scores and improvement in grip strength compared to those receiving corticosteroid injections [19]. These improvements were sustained over a longer follow-up period, suggesting that PRF may offer more durable benefits than traditional treatments like corticosteroids.
Another randomized controlled trial comparing PRF to platelet-rich plasma (PRP) in lateral epicondylitis found that while both treatments were effective in reducing pain and improving function, PRF offered superior long-term outcomes, with a lower rate of symptom recurrence [20]. This may be due to the sustained release of growth factors from the fibrin matrix in PRF, which promotes more prolonged tissue healing compared to PRP, where growth factors are released more rapidly.
The current study has presented strong evidence for significant pain reduction and positive changes in sonographic examination after a combination of PRF and ALB-PRF treatment. One year follow-up data has confirmed sustained long-term effects.
Arguably lateral epicondylitis often has a natural course of healing and some of the patients in this study might have received similar results over time without treatment. However, multiple studies have shown that LE patients presenting with typical hypoechoic sonographic changes in the attachment site of the ECRB tendon in the lateral epicondyle often have a poor prognosis and oftentimes face a longer period of pain often over many years [21-23].
This study has some limitations in its design, for instance, no control or placebo group could be included due to the study design. The diagnostic criteria for LE lack a golden standard and the data produced in this study are therefore difficult to compare with similar studies on other treatment modalities. However, the sample size in the current study is large, and the follow-up period is longer than most similar studies on other treatment modalities for LE. Besides that, the evidence presented is very strong. The treated elbows were tested in 4 different tests over time and measured with ultrasound, all tests and sonographic pictures showed significant positive changes over time. One observation in the data analyzed was that 25% more patients had problems with their right elbow than the left one. Logically this could be explained by the normal distribution in the population with a dominant right arm and hand. No further analyzes were made regarding this point.
Although some limitations to this study exist, the treatment intervention presented in this article might be recommended in cases of clinically diagnosed LE. The treatment is minimally invasive, has very low risk of infection or rejection [24,25] and has basically no convalescence.
6. Other Interventions
Steroid injections used to be considered the gold standard treatment for LE and other tendinopathies for many years and was often offered as a first line treatment in primary healthcare. However, the positive short-term effects have been shown in multiple studies to be a long-term harm, and corticosteroid injections are often considered inappropriate in the modern healthcare practice [26,27]. According to a meta-analysis of the effects of corticosteroids in the treatment of LE compared to placebo, corticosteroid injections are neither meaningfully palliative nor disease modifying when used to treat ECRB [28].
According to a large study published in April 2024, no evidence for surgery of LE exist and it was described as controversial and the prevailing trend for the treatment of LE is nonsurgical [29].
In summary, compared to other treatment modalities, such as steroid injections or surgery, PRF presents a viable alternative with significant positive short- and long-term effects with very little side effects or risks.
7. Conclusion
In conclusion, PRF combined with ALB-PRF is an effective treatment for clinically diagnosed lateral epicondylitis. Significantly lowered NRS pain scores in clinical and orthopedic tests as well as significant positive changes in sonographic pictures 3 months after the treatment combined with 1 year-follow up data indicates significant long-term effects.
8. Declaration
Ethics Approval: According to the Ethics Commission of Stockholm, Sweden, retrospective database-based studies do not require ethical approval and patient informed consent whenever the data were acquired, saved and treated anonymously. This applies to the present study.
The study was conducted in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate: Not applicable.
Consent for Publication: This manuscript does not contain any individual person’s data. All data exposed in this manuscript was anonymized.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
Acknowledgements: The author was the main and only contributor to the manuscript.
Competing Interests: The author declares that he has no competing interests.
Authors’ contributions: All texts, design, literature review and drafting of this study was done by TO, responsible for the submitted manuscript.
Availability of data and materials: All data generated or analyzed during this study can be provided by the corresponding author upon reasonable request and is available for review by the Editor-in-Chief of this journal.
References
- Kraushaar BS, Nirschl RP. Tendinosis of the elbow (tennis elbow): Clinical features and findings of histological, immunohistochemical, and electron microscopy studies. Journal of Bone and Joint Surgery 81 (1999): 259-278.
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: A systematic review of randomized controlled trials. Lancet 376 (2015): 1751-1767.
- Smidt N, Assendelft WJJ, van der Windt DAWM, et al. Corticosteroid injections for lateral epicondylitis: A systematic review. Pain 96 (2002): 23-40.
- Choukroun J, Diss A, Simonpieri A, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 101 (2001): e56-e60.
- Ehrenfest DMD, Rasmusson L, Albrektsson T. Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends in Biotechnology 28 (2010): 64-73.
- Averell N, Goodwin B, Park S, et al. The concentration of platelets in PRP does not affect pain outcomes in lateral epicondylitis: a systematic review and meta-analysis. Pain Manag 14 (2024): 223-233.
- Fujioka-Kobayashi M, Schaller B, Mourão CFAB, et al. Biological characterization of an injectable platelet-rich fibrin mixture consisting of autologous albumin gel and liquid platelet-rich fibrin (Alb-PRF). Platelets 32 (2021): 74-81.
- Wu PI, et al. Platelet-rich fibrin in musculoskeletal medicine: From bench to bedside. American Journal of Sports Medicine 45 (2017): 1951-196.
- Liao HT, James IB, Marra KG. The role of platelet-rich fibrin in enhancing tissue regeneration: Current clinical applications and future directions. Tissue Engineering Part B: Reviews 25 (2019): 221-232.
- Miron RJ, Pinto NR, Quirynen M, et al. Standardization of relative centrifugal forces in studies related to platelet-rich fibrin. Journal of periodontology 90 (2019): 817-20.
- Fujioka-Kobayashi M, Katagiri H, Kono M, et al. Improved growth factor delivery and cellular activity using concentrated platelet-rich fibrin (C-PRF) when compared with traditional injectable (i-PRF) protocols. Clin Oral Investig 24 (2020): 4373-4383.
- Miron RJ, Pikos MA, Estrin NE, et al. Extended platelet-rich fibrin. Periodontol 2000 94 (2024): 114-130.
- Connell D, Burke F, Coombes P, et al. Sonographic examination of lateral epicondylitis. AJR Am J Roentgenol 176 (2001): 777-82.
- Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, Same or Different? Are Visual Analog Scale Values and Numerical Rating Scale Equally Viable Tools for Assessing Patients after Microdiscectomy? Pain Res Manag 29 (2022): 5337483.
- Karanasios S, Korakakis V, Moutzouri M, et al. Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)-a systematic review. Journal of Hand Therapy (2021).
- Saroja G, Leo A, Aseer P, et al. Diagnostic accuracy of provocative tests in lateral epicondylitis. International Journal of Physiotherapy and Research 2 (2014): 815-823.
- Pienimäki T, Tarvainen T, Siira P, et al. Associations Between Pain, Grip Strength, and Manual Tests in the Treatment Evaluation of Chronic Tennis Elbow. Clin J Pain 18 (2002): 164-170.
- Pitts G, Uhl TL, Day JM. Grip strength is more sensitive to changes in elbow position than isolated wrist extension strength in patients with lateral elbow tendinopathy, Journal of Hand Therapy 34 (2021): 509-511.
- Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. American Journal of Sports Medicine 34 (2006): 1774-1778.
- Wang JH, et al. Comparison of the clinical efficacy of platelet-rich plasma vs platelet-rich fibrin in chronic tendinopathy. Journal of Orthopaedic Surgery and Research 13 (2018): 194.
- Levin D, Nazarian LN, Miller TT, et al. Lateral epicondylitis of the elbow: US findings. Radiology 237 (2005): 230-4.
- Lee MH, Cha JG, Jin W, et al. Utility of sonographic measurement of the common tensor tendon in patients with lateral epicondylitis. AJR Am J Roentgenol 196 (2011): 1363-7.
- Dones VC 3rd, Grimmer K, Thoirs K, et al. The diagnostic validity of musculoskeletal ultrasound in lateral epicondylalgia: a systematic review. BMC Med Imaging 14 (2014): 10.
- Banihashemi M, Zabolinejad N, Salehi M, et al. Platelet-rich plasma use for facial rejuvenation: a clinical trial and review of current literature. Acta Biomed 92 (2021).
- Everts P, Onishi K, Jayaram P, et al. Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci 21 (2020).
- Scott A, Khan KM. Corticosteroids: short-term gain for long-term pain? Lancet 376 (2010): 1714-5.
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 376 (2010): 1751-67.
- Claessen FMAP, Heesters BA, Chan JJ, et al. A Meta-Analysis of the Effect of Corticosteroid Injection for Enthesopathy of the Extensor Carpi Radialis Brevis Origin. J Hand Surg Am 41 (2016): 988-998.e2.
- Ruiz SG, DeVos MJ, Warth RJ, et al. Treatment of Lateral Epicondylitis: Is Surgery Still an Option? Eplasty 24 (2024): e18.







 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 