Pre-Operative Vitamin D Optimization and Osseointegration in Cementless THR
Anil Kumar Sahu1, Alok Prusty2, Gopabandhu Patra3*
1Professor and H.O.D, Department of Orthopaedic Surgery, Shree Jagannath Medical College & Hospital, Baliguali, Puri, Odisha, India
2Assistant Professor, Department of Orthopaedics, IMS & SUM Hospital, Campus 2, Bhubaneswar, Odisha, India
3Associate Professor, Department of Orthopaedics, SCB Medical College, Cuttack, Odisha, India
*Corresponding Author: Gopabandhu Patra, Associate Professor, Department of Orthopaedics, SCB Medical College, Cuttack, Odisha, India.
Received: 20 September 2025; Accepted: 31 October 2025; Published: 21 November 2025
Article Information
Citation: Anil Kumar Sahu, Alok Prusty, Gopabandhu Patra. Pre-Operative Vitamin D Optimization and Osseointegration in Cementless THR. Journal of Orthopedics and Sports Medicine. 7 (2025): 527-531.
View / Download Pdf Share at FacebookAbstract
Background: Vitamin D is crucial in musculoskeletal health, bone metabolism, and implant integration. Deficiency is common among patients undergoing total hip arthroplasty and may affect functional outcomes and osseointegration. Optimizing preoperative vitamin D could improve recovery and implant success in cementless THR.
Methods: A retrospective multicenter cohort study was carried out across SCB Medical college and IMS & SUM hospital in Odisha, India, from January 2024 to August 2025, including 258 patients undergoing cementless THR. Preoperative vitamin D levels were measured, and supplementation was provided for deficient or insufficient patients. Functional outcomes, radiographic osseointegration, and post-operative complications were assessed at 6 weeks and 3 months.
Results: Vitamin D deficiency was observed in 38% of patients, with only 27.1% being sufficient. Patients with sufficient vitamin D had higher baseline functional scores and better osseointegration (94.3%) compared to deficient patients (81.6%). Deficient patients also showed a higher trend of post-operative complications such as delayed healing and implant loosening.
Conclusion: Preoperative vitamin D deficiency is more common in patients undergoing cementless THR and is associated with lower baseline function, suboptimal osseointegration, and increased complication risk.
Keywords
Vitamin D; Total hip replacement; Osseointegration, Functional outcomes, Arthroplasty
Article Details
1. Introduction
Vitamin D, particularly its circulating form 25-hydroxy-vitamin D (25(OH)D), is a vital regulator of calcium and phosphate metabolism, supporting skeletal health and neuromuscular performance [1]. Deficiency of 25(OH)D has become increasingly widespread and is implicated in the development of musculoskeletal disorders, including osteoarthritis [2]. Suboptimal levels of vitamin D are associated with impaired bone mineralization, reduced muscle function, higher pain perception, and difficulties in mobility and balance [3-5]. In the context of joint replacement surgery, patients with low vitamin D levels often present with diminished pre-operative function and have been reported to experience less favorable recovery trajectories following total hip arthroplasty (THA) and total knee arthroplasty (TKA) [6,7].
For cementless total joint arthroplasty (TJA), osseointegration of press-fit implants is highly dependent on bone quality. Vitamin D deficiency, as a marker of poor skeletal health, has raised concerns regarding its potential to compromise implant fixation and long-term success [8,9]. In response, several centers have introduced pre-operative vitamin D optimization strategies, demonstrating improvements in joint-related symptoms and pain relief prior to surgery [10–13]. Moreover, postoperative vitamin D supplementation has been proposed to provide additional benefits in terms of functional recovery, patient satisfaction, and quality of life [12-14].
Despite this, the true burden of vitamin D deficiency in patients undergoing TJA remains inconsistent across studies. Reports from Europe and the United States describe prevalence rates ranging from 15% to 86% among individuals with osteoarthritis or scheduled for joint replacement [7,15-17]. Importantly, a predominant number of these studies have only assessed White populations, whereas existing evidence reveals that Black patients may experience vitamin D deficiency at rates 15–20 times higher, contributing to worse musculoskeletal outcomes [4,5]. Further variability arises from differences in how deficiency has been defined, though recent guidelines have standardized the classification as <12 nmol/L for deficiency and 12–30 nmol/L for insufficiency [19,20]. This study intends to examine whether pre-operative vitamin D optimization enhances osseointegration and early functional outcomes in cementless THR, while also examining its relationship with patient-reported outcomes and short-term post-operative complications in a diverse surgical population.
2. Methods
2.1 Study design
This was a retrospective comparative cohort investigation designed to examine the effect of pre-operative vitamin D optimization on functional outcomes and osseointegration in cementless THR. Institutional Ethics Committee approvals were obtained from all participating centers, with waiver of informed consent due to the retrospective nature of the study. Clinical charts and radiographs were reviewed to collect pre-operative, peri-operative, and post-operative data along with vitamin D treatment records.
2.2 Study setting and duration
- • The multicentric study was conducted across two institutions: SCB Medical College, Cuttack and IMS & SUM hospital in Odisha, India.
- • The study duration was from January 2024 to August 2025
2.3 Sample size and participants
A total of 258 patients undergoing cementless THR were included. Patients aged 18 years and above undergoing elective primary arthroplasty were eligible. Exclusion criteria included revision surgeries for infection (only aseptic revisions included), arthroplasty for acute trauma or malignancy, incomplete medical or radiographic records, and loss to follow-up before 3 months. Patients were evaluated at baseline, 6 weeks, and 3 months post-operatively.
2.4 Variables
- • Pre-operative: demographic details (age, sex, BMI, smoking/alcohol status, comorbidities), primary diagnosis, baseline serum 25(OH)D levels, and functional scores (Oxford Hip Score/Oxford Knee Score)
- • Peri-operative: surgical procedure, implant type (cementless press-fit), operative time, intraoperative blood loss, and hospital stay
- • Post-operative: functional outcome scores at 6 weeks and 3 months, radiographic evidence of osseointegration (early signs of implant stability and absence of radiolucent lines), and complications including wound healing problems, prosthetic joint infection, re-operation, or readmission
2.5 Vitamin D supplementation protocol
All patients underwent pre-operative serum 25(OH)D testing. Supplementation was prescribed as per institutional protocol:
- • Deficient patients (<12 nmol/L): 60,000 IU cholecalciferol orally once weekly for 6 weeks.
- • Insufficient patients (12–30 nmol/L): 1,000 IU cholecalciferol orally daily for 6 weeks.
- • Sufficient patients (>30 nmol/L): no supplementation.
Supplementation began at least two weeks before surgery whenever feasible, and compliance was reinforced during pre-anesthetic evaluations.
2.6 Data sources and management
Data were retrieved from hospital electronic health records and patient files. Functional outcome scores (Oxford Hip score/Oxford Knee Score, range 0–48) were documented numerically. Vitamin D levels were measured using chemiluminescence immunoassay. Radiographic evaluation of osseointegration was independently performed by two orthopaedic surgeons blinded to vitamin D status. Post-operative complications were categorized as binary outcomes (yes/no).
2.7 Statistical analysis
SPSS v20 was used to analze the data with p value < 0.05 considered statistically significant.
3. Results
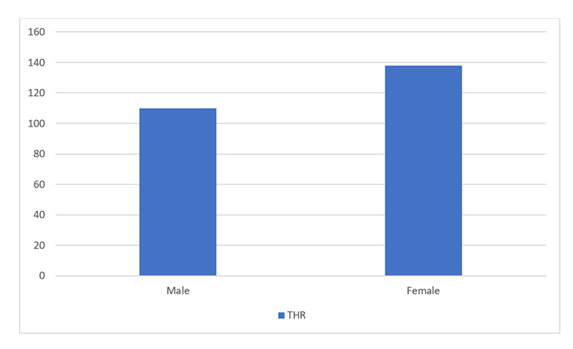
The study cohort encompassed 258 patients undergoing THR. The mean age was slightly higher in the women (62.3 ± 8.4 years) compared to men (60.2 ± 7.9 years). The overall gender distribution showed a slight female predominance (138 females vs. 110 males). BMI values reported a mean of 26.8 ± 3.5 kg/m² across the cohort. Vitamin D deficiency was prevalent with 39.4% of all patients having deficient levels and an additional 34.1% categorized as insufficient. Only 26.5% of participants had sufficient vitamin D at baseline, highlighting a significant burden of hypovitaminosis D in this surgical population (Table 1, Figure 1).
|
Variable |
THR (n=258) |
|
Age (years, mean ± SD) |
61.4 ± 8.2 |
|
Mean age of males |
60.2 ± 7.9 years |
|
Mean age of females |
62.3 ± 8.4 years |
|
Gender (Male/Female) |
110/138 |
|
BMI (kg/m², mean ± SD) |
26.8 ± 3.5 |
|
Vitamin D Deficient (%) |
39.4% |
|
Vitamin D Insufficient (%) |
34.1% |
|
Vitamin D Sufficient (%) |
26.5% |
Table 1: Baseline Characteristics of Participants.
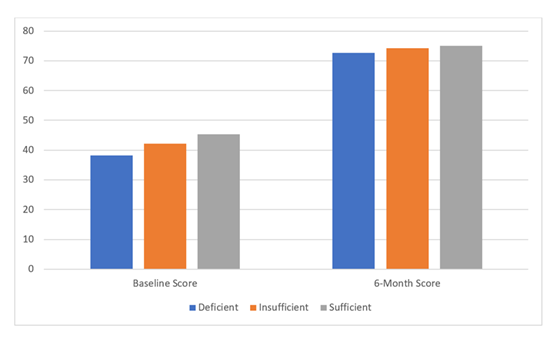
At baseline, patients with sufficient vitamin D reported higher functional scores (45.3 ± 6.7) compared to those with insufficient (42.1 ± 6.9) and deficient levels (38.2 ± 7.6), with differences being statistically significant (p < 0.001). This suggests that vitamin D sufficiency is associated with better pre-operative musculoskeletal function and quality of life. Interestingly, although patients with sufficient vitamin D had the highest absolute scores post-operatively at 6 months, the greatest improvement was noted in the deficient cohort (+34.4 points), in contrast to insufficient (+32.2) and sufficient (+29.8) (Table 2, Figure 2).
|
PROMs (Mean ± SD) |
Deficient (n=98) |
Insufficient (n=90) |
Sufficient (n=70) |
p-value |
|
Baseline Score |
38.2 ± 7.6 |
42.1 ± 6.9 |
45.3 ± 6.7 |
<0.001 |
|
6-Month Score |
72.6 ± 8.4 |
74.3 ± 8.1 |
75.1 ± 7.9 |
0.032 |
|
Mean Improvement |
+34.4 |
+32.2 |
+29.8 |
0.018 |
Table 2: Patient-Reported Outcome Measures (PROMs) by Vitamin D Status.
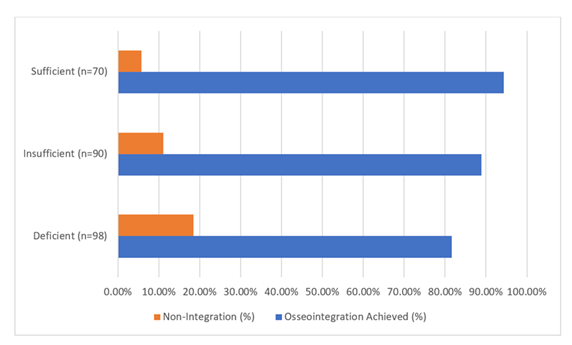
Radiographic assessment revealed that osseointegration was most successful in the vitamin D sufficient group, with 94.3% achieving integration compared to 88.9% in the insufficient group and 81.6% in the deficient group (p = 0.041). The higher rate of non-integration among deficient patients (18.4%) highlights a clinically significant concern. Inadequate osseointegration may predispose these patients to chronic complications like implant loosening and early revision (Table 3, Figure 3).
|
Vitamin D Status |
Osseointegration Achieved (%) |
Non-Integration (%) |
|
Deficient (n=98) |
81.6% |
18.4% |
|
Insufficient (n=90) |
88.9% |
11.1% |
|
Sufficient (n=70) |
94.3% |
5.7% |
|
p-value |
0.041 |
Table 3: Radiological Osseointegration at 12 Months.
Post-operative complications were observed across all vitamin D groups, but with a trend toward higher frequencies in the deficient group. Superficial infections were reported in 6.1% of deficient patients, compared to 4.4% and 2.9% in the insufficient and sufficient groups, respectively. Similarly, delayed wound healing occurred more often in deficient patients (8.2%), suggesting impaired tissue recovery in the presence of low vitamin D. Implant loosening, though rare, was only observed in deficient (2%) and insufficient (1.1%) patients, while none occurred in the sufficient group (Table 4).
|
Complication Type |
Deficient (n=98) |
Insufficient (n=90) |
Sufficient (n=70) |
p-value |
|
Superficial Infection |
6 (6.1%) |
4 (4.4%) |
2 (2.9%) |
0.42 |
|
Delayed Healing |
8 (8.2%) |
5 (5.5%) |
2 (2.9%) |
0.38 |
|
Implant Loosening |
2 (2.0%) |
1 (1.1%) |
0 (0%) |
0.56 |
Table 4: Post-Operative Complications.
4. Discussion
The present study observed a high prevalence of vitamin D deficiency and insufficiency among patients undergoing THA, with 38% of participants classified as deficient and an additional 34.9% as insufficient. This aligns with findings from a systematic review indicating that 13% to 75% of patients undergoing total joint arthroplasty (TJA) have vitamin D deficiency [21]. However, the optimal threshold for vitamin D levels remains a subject of debate, as some studies suggest that levels above 20 ng/mL may be sufficient for bone health [21,22].
In terms of functional outcomes, the present study found that patients with sufficient vitamin D levels reported higher baseline patient-reported outcome measures (PROMs) scores compared to those with insufficient or deficient levels. This is consistent with research indicating that low preoperative vitamin D levels are associated with lower baseline PROMs [23]. Interestingly, the greatest improvement in PROMs scores postoperatively was observed in the deficient group, suggesting that its supplementation may have a more pronounced effect in patients with lower baseline levels. This finding is in line with a study that reported improved functional outcomes following vitamin D supplementation in individuals with deficiency of that vitamin [23].
Regarding radiological outcomes, the present study demonstrated that osseointegration rates were greatest in the vitamin D sufficient group, supporting the notion that this vitamin plays a critical role in bone healing and implant fixation. This is corroborated by research indicating that deficiency of this vitamin resulted in lower osseointegration rates and increased risk of periprosthetic joint infection [24]. The higher rate of non-integration among deficient patients in the present study highlights a clinically significant concern, as inadequate osseointegration may predispose these patients to long-term complications such as implant loosening and early revision.
The present study also observed a trend toward higher frequencies of postoperative complications, including superficial infections and delayed wound healing, in the vitamin D deficient group. This is consistent with findings from other studies that have reported an increased risk of postoperative complications, including periprosthetic joint infection, in patients with low preoperative vitamin D levels [22,25].
The present investigation, being retrospective in nature, is subject to inherent biases related to data collection and patient selection. The follow-up period was also relatively short (3 months), limiting the ability to assess the chronic implant survival and functional outcomes. Additionally, while we accounted for vitamin D supplementation, compliance and exact serum level changes post-supplementation were not systematically monitored. Future research should focus on prospective, randomized controlled trials with longer follow-up to evaluate the optimal dosing and timing of vitamin D supplementation, its sustained impact on osseointegration, and the reduction of postoperative complications in diverse patient populations.
5. Conclusion
The study demonstrates that preoperative vitamin D deficiency is highly prevalent among patients undergoing total hip arthroplasty and is associated with lower baseline functional scores, reduced rates of osseointegration, and a higher trend of postoperative complications. Optimizing vitamin D levels prior to surgery appears to improve functional recovery, enhance implant integration, and potentially reduce the risk of complications. These findings underscore the importance of routine preoperative screening and supplementation of vitamin D as a key component of patient optimization in cementless THR.
Acknowledgement:
The authors sincerely thank the staff and patients of Shree Jagannath Medical College & Hospital, IMS & SUM Hospital, and SCB Medical College for their support and participation in this study.
Source of Funding:
This study received no source of funding.
Conflicts of Interest:
None.
References
- Norman AW. From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. Am J Clin Nutr 88 (2008): 491S-499S.
- Holick MF. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord 18 (2017): 153-165.
- Bergink AP, Zillikens MC, Van Leeuwen JPTM, et al. 25-Hydroxyvitamin D and osteoarthritis: a meta-analysis including new data. Semin Arthritis Rheum 45 (2016): 539-546.
- Kim H, Chandler P, Ng K, et al. Obesity and efficacy of vitamin D3 supplementation in healthy black adults. Cancer Causes Control 31 (2020): 303-307.
- Xia J, Tu W, Manson JE, et al. Combined associations of 25-hydroxivitamin D and parathyroid hormone with diabetes risk and associated comorbidities among U.S. white and black women. Nutr Diabetes 11 (2021): 29.
- Maniar RN, Patil AM, Maniar AR, et al. Effect of preoperative vitamin D levels on functional performance after total knee arthroplasty. Clin Orthop Surg 8 (2016): 153-156.
- Jansen J, Haddad F. High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl 95 (2013): 569-572.
- Matthias J, Bostrom MP, Lane JM. A comparison of risks and benefits regarding hip arthroplasty fixation. J Am Acad Orthop Surg Glob Res Rev 5 (2021): e21.
- Lei P, Hu R, Hu Y. Bone defects in revision total knee arthroplasty and management. Orthop Surg 11 (2019): 15-24.
- Chevalley T, Brandi ML, Cashman KD, et al. Role of vitamin D supplementation in the management of musculoskeletal diseases: update from an European society of clinical and economical aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO) working group. Aging Clin Exp Res 34 (2022): 2603-2623.
- Young AR, Morgan KA, Ho TW, et al. Melanin has a small inhibitory effect on cutaneous vitamin D synthesis: a comparison of extreme phenotypes. J Invest Dermatol 140 (2020): 1418-1426.e1.
- Mouli VH, Schudrowitz N, Carrera CX, et al. High-dose vitamin D supplementation can correct hypovitaminosis D prior to total knee arthroplasty. J Arthroplasty 37 (2022): 274-278.
- Weintraub MT, Guntin J, Yang J, et al. Vitamin D3 supplementation prior to total knee arthroplasty: a randomized controlled trial. J Arthroplasty 38 (2023): S114-S119.
- Morrison RJM, Fishley WF, Rankin KS, et al. The effect of vitamin D supplementation on outcomes following total hip or knee arthroplasty surgery: a rapid systematic review of current evidence. EFORT Open Rev 7 (2022): 305-311.
- Maier GS, Horas K, Seeger JB, et al. Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop 38 (2014): 1499-1504.
- Nawabi DH, Chin KF, Keen RW, et al. Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement: a cause for concern? J Bone Joint Surg Br 92-B (2010): 496-499.
- Maier GS, Maus U, Lazovic D, et al. Is there an association between low serum 25-OH-D levels and the length of hospital stay in orthopaedic patients after arthroplasty? J Orthop Traumatol 17 (2016): 297-302.
- Bischoff-Ferrari HA. Positive association between serum 25-hydroxyvitamin D level and bone density in osteoarthritis. Arthritis Care Res (Hoboken) 53 (2005): 926-931.
- Munns CF, Shaw N, Kiely M, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metabol 101 (2016): 394-415.
- Bouillon R, Carmeliet G. Vitamin D insufficiency: definition, diagnosis and management. Best Pract Res Clin Endocrinol Metab 32 (2018): 669-684.
- Iglar PJ, Hogan KJ. Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg 9 (2015): 14.
- Birinci M, Hakyemez ÖS, Geçkalan MA, et al. Effect of vitamin D deficiency on periprosthetic joint infection and complications after primary total joint arthroplasty. J Arthroplasty 39 (2024): S151-S157.
- Aggarwal S, Scott M, Koch M, et al. Low pre-operative vitamin D associated with lower baseline PROMs but greater improvement following total joint arthroplasty. J Orthop Rep 4 (2025): 100430.
- Maier GS, Horas K, Seeger JB, et al. Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop 38 (2014): 1499-1504.
- Lakhera KK, Babu A, Patel P, et al. Association between pre-operative 25-hydroxy vitamin D deficiency and surgical site infection after oral cavity oncology surgery: a cross-sectional study in a tertiary cancer center in northwestern India. Indian J Surg Oncol 15 (2024): 218-224.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 