Primary Epididymal Adenocarcinoma: Case report and Review of the Literature
Nives Kolesarić1*, Cvjetko Lež1, Monica Stephany Kirigin2, Ivica Balagović3, Božo Krušlin2
1Department of Pathology and Cytology, Zabok General Hospital, Zabok, Croatia
2“Ljudevit Jurak” Department of Pathology and Cytology, Sisters of Charity Hospital, Zagreb, Croatia
3Department of Urology, Zabok General Hospital, Zabok, Croatia
*Corresponding Author: Nives Kolesarić, Department of Pathology and Cytology, Zabok General Hospital, Zabok, Croatia.
Received: 01 December 2025; Accepted: 31 December 2025; Published: 06 January 2026
Article Information
Citation: Nives Kolesarić, Cvjetko Lež, Monica Stephany Kirigin, Ivica Balagović, Bozo Krušlin. Primary Epididymal Adenocarcinoma: Case report and Review of the Literature. Archives of Clinical and Biomedical Research. 10 (2026): 16-19.
View / Download Pdf Share at FacebookAbstract
Primary epididymal adenocarcinoma (PEA) is an extremely rare tumor, with fewer than 30 cases reported in the English literature. The diagnosis of PEA is based on histological examination and comprehensive clinical evaluation to exclude metastatic adenocarcinoma. We report a case of primary adenocarcinoma of the epididymis in a 63-year-old man presenting with hydrocele. The patient underwent right radical orchiectomy, and the diagnosis of PEA was established. This case demonstrates the importance of pathological examination and the consideration of a malignant differential diagnosis in an apparently benign pathology such as hydrocele, as well as the use of different diagnostic methods to rule out metastatic adenocarcinoma of the epididymis.
Keywords
<p>Epididymal Adenocarcinoma</p>
Article Details
1. Introduction
Primary epididymal tumors are extremely rare, with approximately 25% of them being malignant [1]. Malignant epididymal tumors exist either as primary or metastatic lesions. Metastatic adenocarcinomas can originate from the prostate, stomach, colorectum, kidney and pancreas, as well as other sites, such as malignant mesothelioma [2,3]. The predominant histological types of primary epididymal malignancies are rhabdomyosarcoma, leiomyosarcoma, liposarcoma, and finally adenocarcinoma, which accounts for less than 10% of all epididymal malignancies, with fewer than 30 cases reported in the English literature [4,5].
We report a case of primary adenocarcinoma of the epididymis in a 63-year-old man and summarize 13 cases reported in the English literature over the past 35 years with immunohistochemical analysis and/or extensive radiological imaging.
2. Case Report
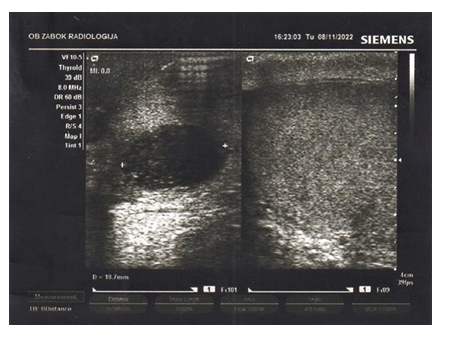
A 63-year-old patient presented to the urology department in September 2022 with a right testicular mass. He reported lifting heavy objects one month earlier. Past medical history included diabetes mellitus, obesity and arterial hypertension. The palpated scrotal mass was compared to the size of a goose egg. Ultrasound performed the same day resulted in a clinical diagnosis of hydrocele caused by trauma.
Right radical orchiectomy was performed and the specimen sent to pathology.
2.1 Pathological Examination
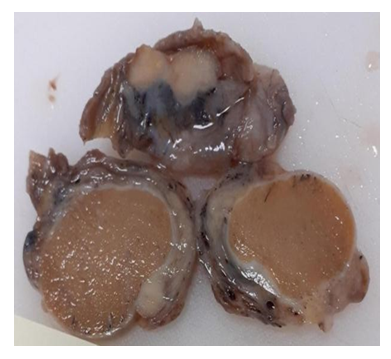
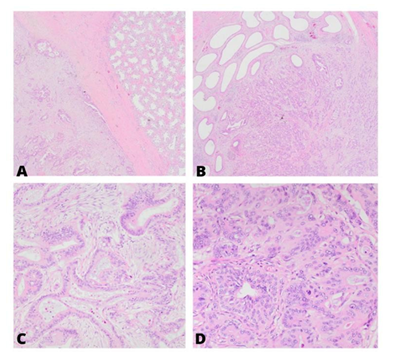
Right testis, epididymis and spermatic cord measuring 4.8 × 4.1 × 3.3 cm were submitted to pathology. Gross examination showed a unifocal, nodular, grey tumor confined to the epididymis, measuring 2.2 cm in largest diameter. Histologic examination revealed a tumor consisting of well and moderately differentiated glandular formations with marked mitotic activity. The tumor infiltrated surrounding fatty tissue, the tunica albuginea and tunica vaginalis. No lymphovascular invasion was found. Resection margins were negative (Figure 1).
Immunohistochemical analysis was performed to rule out the most common metastatic adenocarcinomas to the epididymis. PSA, Calretinin, TTF-1, CK7, WT1 and EMA stains came back negative. Only CAIX showed focal positivity.
2.2 Laboratory Tests
HE4, CEA, alpha-fetoprotein, CA 19-9, PSA, free and total PSA level were normal, but CYFRA 21-1 levels were slightly elevated (2.96 ug/L). All hormone tests came back normal (total testosterone, SHBG, FAI, free testosterone, bHCG).
Blood tests showed iron deficiency anemia. Iron supplementation was prescribed (Figure 2).
2.3 Abdominal and Pelvic CT and Postoperative Ultrasound:
CT scan of the abdomen and pelvis did not detect other primary tumors or signs of metastatic disease. The only pathological radiological finding was diverticulosis of the sigmoid and descending colon.
Postoperative ultrasound showed a smaller hematoma in the right testicle at the site of the previous operation (Figure 3.)
No further treatment was suggested by clinicians. 13 months after the surgery, a follow-up CT scan revealed multiple metastases in the liver, wall of the transverse colon, within the right seminal vesicle and in the right ureter. The patient died less than two years after the diagnosis.
3. Discussion
Although there are only about thirty cases of primary adenocarcinoma of the epididymis in the literature, the actual number is probably lower due to lack of use of immunohistochemistry and other diagnostic methods to rule out metastatic adenocarcinoma. There are only ten published cases in the literature with the use of different immunohistochemical stains, and the results are variable [3]. Considering the small number of similar methods employed and differing results, it is still very important to interpret the results of immunohistochemical analysis in the context of the morphological features of the tumor. It is also useful to include other diagnostic methods, such as imaging techniques, endoscopy, hormone tests, tumor markers etc.
In the following, we will specify some important features of our case and reveal new knowledge based on literature review.
The patients were between the ages of 27 and 82, while the average age was 56. According to previous research, patients over the age of 50 are more likely to have primary benign tumors rather than primary malignant tumors, while younger patients have a higher risk of malignancy [2].
In our review, as many as 9 out of 13 patients (69%) were older than 50, so we believe that malignancy should also be suspected in older men with epididymal masses.
8 out of 13 patients (61%) developed metastases in lymph nodes or distant organs. The most common sites of metastases were retroperitoneal lymph nodes, bones, lungs and ureter.
All sites and their frequency are shown in Table 1.
|
Site |
Number |
|
Retroperitoneal lymph nodes [6-9] |
3 |
|
Lungs [1,5] |
2 |
|
Ureter [8,10] |
2 |
|
Bones |
2 |
|
acetabulum [11] |
1 |
|
Shoulder [8] |
1 |
|
Ribs [8] |
1 |
|
Spine [8] |
1 |
|
Spleen [11] |
1 |
|
Liver [11] |
1 |
|
Testis [12] |
1 |
|
Vena cava [8] |
1 |
Table 1: All metastases of primary adenocarcinoma of the epididymis reported in the literature.
There are no specific immunohistochemical markers to diagnose PEA, but immunohistochemical analysis can help rule out metastatic adenocarcinoma of the epididymis. We used prostate specific antigen (PSA), calretinin, TTF-1 and WT-1 to exclude metastatic prostate cancer, mesothelioma and lung adenocarcinoma.
In previous research, it was concluded that EMA is positive in primary adenocarcinoma of the epididymis [3], which was not the case in our patient. We also found a case of undifferentiated adenocarcinoma of the epididymis with negative EMA stain [12]. We believe a stain that should be positive in all PEAs has not yet been discovered. The results of our immunohistochemical analysis are compared with those reported in the literature in Table 2.
|
Strain |
Results |
Positive cases |
Negative cases |
|
CalX |
– |
1/1 |
0/1 |
|
EMA |
– |
3/4 |
1/4 |
|
CK7 |
– |
1/4 |
3/4 |
|
CK20 |
– |
1/2 |
1/2 |
|
PSA |
– |
0/6 |
6/6 |
|
Calretinin |
– |
0/1 |
1/1 |
|
TTF-1 |
– |
0/2 |
2/2 |
Table 2: Our IHC results compared with those reported in the literature
All patients with PEA should undergo radical orchiectomy, but there are no exact guidelines describing who should receive chemotherapy and radiotherapy, nor which chemotherapy drugs are recommended. Cisplatin and etoposide combination chemotherapy was the most commonly used protocol. Although the patients most often received radiation for palliative purposes, one such patient remained disease- free after 42 months, which was the duration of his follow-up [7].
Acknowledgements:
The research project was conducted under the supervision of: prof. dr. sc. Božo Krušlin, dr. med., Specialist in pathology, area of interest – uropathology.
This research project was conducted from 05/02/2023 to 15/12/2023.
Conflicts of Interest:
The authors declare no conflict of interests.
References
- Aydin A, Aksoy HZ, Reis A, et al. Undifferentiated carcinoma of the epididymis. Acta Clin Croat 50 (2021): 415-8
- Ganem JP, Jhaveri FM, Marroum MC. Primary adenocarcinoma of the epididymis: case report and review of the literature. Urology 52 (1998): 904-8.
- Zou ZJ, Xiao YM, Liu ZH. Clinicopathological Characteristics, Treatment, and Prognosis of Rarely Primary Epididymal Adenocarcinoma: A Review and Update. Biomed Res Int 2017:2017.
- Bhatt R, Davaro F, Wong R, et al. Contemporary analysis of epididymal tumors using a national database. Cent European J Urol 74 (2021): 39-43.
- Gupta S, Yan B, Leow PC, et al. Primary mucinous adenocarcinoma of the epididymis: report of a rare case with molecular genetic characterization including mutation analysis of the TP53 gene. Appl Immunohistochem Mol Morphol 23 (2025): 308-12.
- Staník M, Doležel J, Macík D, et al. Primary adenocarcinoma of the epididymis: the therapeutic role of retroperitoneal lymphadenectomy. Int Urol Nephrol 44 (2012): 1049-53.
- Soumarová R, Maňásek V, Perková H, et al. Radiotherapy in the treatment of epididymal adenocarcinoma - case report. Onkologie 35 (2012): 43-5.
- Chauhan RD, Gingrich JR, Eltorky M, et al. The natural progression of adenocarcinoma of the epididymis. J Urol. 166 (2001): 608-10.
- Yu CC, Huang, et al. Papillary Cystadenocarcinoma of the Epididymis: A Case Report and Review of the Literature. J Urol 147 (1992), 162-165.
- Arisan S, Akbulut ON, Cakir OO, et al. Primary adenocarcinoma of the epididymis: case report. Int Urol Nephrol 36 (2004): 77-80.
- Pindoria N, Miki Y, Tay A, et al. Epididymal papillary cystadenocarcinoma metastasising to the testis in a patient with infertility managed with Onco-microTeSE. J Surg Case Rep (2016):1-3.
- Zengin AY, Topkan E, Aydin A, et al. Undifferentiated Primary Carcinoma of the Epididymis Treated with Sequential Chemoradiotherapy: A Case Report. Int J Hematol Oncol 19 (2009): 242-245.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 