Primary Gastric Burkitt Lymphoma: An Unusual Diagnosis for a Common Symptom
Maria Rogalidou1*, Georgia Avgerinou2, Kalliopi Stefanaki3, Amalia Patereli3, Maria Gavra4, Elissavet Georgiadou5, Antonis Kattamis2, Alexandra Papadopoulou1
1Division of Gastroenterology and Hepatology, First Department of Paediatrics National and Kapodistrian
University of Athens 'Aghia Sophia' Children's Hospital, Athens, Greece
2Division of Hematology and Oncology, First Department of Paediatrics National and Kapodistrian University of Athens 'Aghia Sophia' Children's Hospital, Athens, Greece
3Pathology Department, Agia Sofia Children’s
Hospital, Athens, Greece
4CT, MRI and PET/CT Department, “Agia Sofia” Children’s Hospital, Athens, Greece
5First Department of Paediatrics National and
Kapodistrian University of Athens 'Aghia Sophia' Children's Hospital, Athens, Greece
*Corresponding author: Maria Rogalidou, MD, PhD, Division of Gastroenterology and Hepatology, First Department of Pediatrics, University of Athens, Agia Sofia Children’s Hospital, Athens, Greece.
Received: September 26, 2025; Accepted: October 21, 2025; Published: November 07, 2025
Article Information
Citation: Maria Rogalidou, Georgia Avgerinou, Kalliopi Stefanaki, Amalia Patereli, Maria Gavra, Elissavet Georgiadou, Antonis Kattamis, Alexandra Papadopoulou. Primary Gastric Burkitt Lymphoma: An Unusual Diagnosis for a Common Symptom. Archives of Clinical and Biomedical Research. 9 (2025): 480-484.
View / Download Pdf Share at FacebookAbstract
Non-Hodgkin lymphomas (NHLs) account for about 4% of malignancies in children younger than 15 years old [1]. Burkitt lymphoma (BL) is an aggressive non-Hodgkin B cell lymphoma, characterized by the translocation of the MYC oncogene [2]. Intermittent epigastric pain and vomiting are common symptoms in children and adolescents, and in most cases no special further investigations are required. Proton pump inhibitors are often prescribed as an initial measure to relieve symptoms. However, if symptoms persist or are accompanied by other findings such as anemia or weight loss, further investigation is required and, surprisingly, a very rare disease may be the final diagnosis. Primary non-Hodgkin's lymphoma (NHL) of the gastrointestinal tract is the most common extranodal lymphoma in children [3]. However, primary gastric NHL is rare in children [4] and accounts for less than 2% of pediatric NHL cases [5]. Burkitt lymphoma (BL) is a common type of NHL, but gastric BL usually occurs in older people, while it is very rare in children [6].
Keywords
<p>Non-Hodgkin lymphomas; Adolescents; Burkitt lymphoma; Pediatric; Gastrointestinal tract; Diagnosis; Vomiting</p>
Article Details
Case Presentation
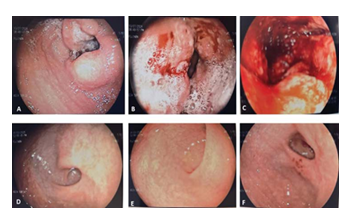
A 14.5 years old male referred for the evaluation of abdominal pain and intermittent coffee grounds vomiting without anemia. The symptoms had started three months before and were initially attributed to gastritis. His general pediatrician (GP) prescribed Proton Pump Inhibitors (PPIs), which initially relieved his symptoms. However, two months later, symptoms recurred. Pediatric gastroenterologist recommended more extensive work-up for Helicobacter pylori (HP) infection and celiac disease and an increased dose of PPIs. Blood tests, performed and revealed anemia and the patient was referred to our department for further evaluation and treatment. Upon admission, the patient was alert, afebrile, tachycardic (pulse 100/min) with normal blood pressure of 110/60 mm Hg and oxygen saturation of 100%. He was undernourished with body weight 34.5kg (z-score -2.73), height 148.5cm (z-score -2.22) and body mass index 15.6 (z-score -2.08). The patient’s medical history was unremarkable, with the exception of a developmental delay for which he had received speech and ergo therapy at a toddler’s age. On clinical examination, the abdomen was relatively soft on gentle palpation, with no tenderness in the epigastric area or palpable mass. The complete blood count (CBC) showed a hemoglobin level of 9.4g/dl, a platelet count of 434.0 × 109/l, and a white cell count of 9.21 × 109/l without blast forms. Biochemical parameters were within normal range. Celiac antibodies were negative and stool monoclonal antigen for HP was positive. Upper gastrointestinal endoscopy revealed nodular gastritis in the fundus and body of the stomach, a large circular friable mass at the level of the gastric angle between the body and antrum, barely allowing passage of the endoscope in the antrum (Figure 1A). The antral mucosa showed edema, multiple ulcers and severe friability (Figure 1 B,C). The esophagus and the duodenum without specific macroscopic findings.
Figure 1: Macroscopic findings during upper gastrointestinal endoscopy (A,B,C) at diagnosis A: a large circular friable mass at the level of the gastric angle between the body and antrum, barely allowing passage of the endoscope in the antrum. B and C: The antral mucosa showed edema, multiple ulcers and severe friability and D, E, F: Follow-up endoscopy 12 months after completion of treatment revealed resolution of the lesions.
Gastric tumors developing during infancy or childhood show a wide range of pathological types that differ from those in adults. In addition, some tumors that are often encountered in other sites rarely occur in the stomach. Primary gastric tumors in pediatric age are rare [8]. The most common gastric tumors seen in children are summarized in Table 1.
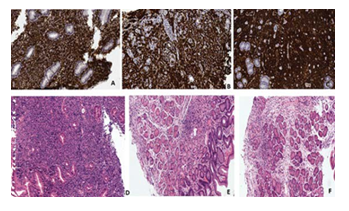
The histological examination (Figure 2 A,B,C and D) revealed a high-grade NHL with features of BL according to the WHO classification 2022 and also HP gastritis, esophagitis and duodenitis. However, it should be noted that although the histology revealed HP gastritis, the CLO test, culture and PCR for HP were all negative and according ESPGHAN guidelines H Pylori infection was not justified [7]. Immunochemistry of gastric lesion revealed expression of CD20/L-26+, CD 10+ bcl-6+, PAX-5/ BSAP+IgM+ monotypic expression κ, c-myc+>90%, Ki-67/MIB-1>95- 100%, MUM-1~10-15%, bcl-2-, CD138-, Tdt-, EBER 1/2of virus Epstein Barr – . Based in the typical histological findings the diagnosis of Burkitt Gastric lymphoma was made.
Table 1: The most common gastric tumors seen in children.
|
Tumor Type |
Benign / Malignant |
Frequency |
Notes |
|
Gastric Teratoma |
Usually benign |
Very rare |
Typically in neonates/ infants; may be mature or immature teratomas |
|
Gastric Adenoma |
Benign, pre-malignant |
Rare |
Associated with FAP, Peutz-Jeghers, or sporadic; can progress to carcinoma |
|
Gastric Adenocarcinoma |
Malignant |
Extremely rare |
Most common adult type; rare in children; poor prognosis |
|
Gastrointestinal Stromal Tumor (GIST) |
Usually malignant |
Rare |
May be sporadic or syndromic (Carney triad, NF1); often KIT wild-type in kids |
|
Lymphoma MALT DLBCL |
Malignant, often associated with Helicobacter pylori |
Uncommon |
More common than adenocarcinoma; often non-Hodgkin’s type |
|
Burkitt Lymphoma |
Malignant |
Uncommon (gastric) |
High-grade B-cell lymphoma; may involve stomach as part of GI tract |
|
Carcinoid Tumor (NET) |
Low-grade malignant |
Rare |
Arises from enterochromaffin-like cells; may be part of MEN1 |
|
Leiomyoma |
Benign |
Very rare |
Smooth muscle origin; endoscopically resectable |
|
Leiomyosarcoma |
Malignant |
Extremely rare |
Aggressive; must differentiate from GIST |
|
Inflammatory Fibroid Polyp |
Benign |
Rare |
Inflammatory pseudotumor; may mimic malignancy |
|
Gastric Duplication Cyst |
Benign |
Rare (congenital) |
Often presents in infancy; may get secondarily infected or obstructive |
|
Rhabdomyosarcoma (Embryonal/Alveolar) |
Malignant |
Extremely rare |
May arise in the gastric wall or GI tract |
|
Hemangioma / Vascular Malformation |
Benign |
Very rare |
May cause bleeding; usually submucosal |
|
Glomus Tumor |
Usually benign |
Very rare |
Rare vascular neoplasm; may mimic GIST |
|
Langerhans Cell Histiocytosis (LCH) |
Clonal proliferation |
Rare |
Can involve GI tract including stomach; systemic disease |
|
Neuroblastoma (metastasis) |
Malignant |
Rare (secondary) |
Primary tumor usually adrenal or sympathetic chain; may infiltrate stomach wall |
Figure 2: A, B, C and D: Histological findings at diagnosis, revealed a high-grade NHL with features of BL according to the WHO classification 2022. Immunochemistry of gastric lesion revealed expression of CD20/L-26+, CD 10+ bcl-6+, PAX-5/ BSAP + IgM + monotypic expression κ, c-myc+>90%, Ki-67/MIB-1>95-100%, MUM-1~10-15%, bcl-2-, CD138-, Tdt-, EBER 1/2of virus Epstein Barr (–). E & F: Histological remission after treatment.
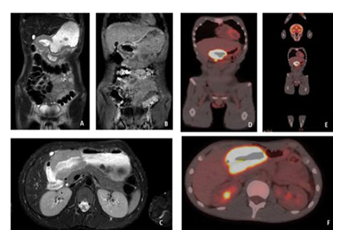
The patient referred to the Pediatric Hematology and Oncology Department for complete work-up and staging. Magnetic resonance imaging (MRI) examination Axial T2w and coronal T1w with gadolinium images demonstrated diffuse thickening of the gastric wall at the level of the pylorus (Figure 3 A,B,C). The positron emission tomography- computed tomography (PET-CT) scan Axial and coronal whole - body PET-CT fusion images (Figure 3 D,E,F) as part of the staging process revealed a hypermetabolic mass in the pyloric antrum with an SUV max of 21,6. There was
Figure 3: Magnetic resonance imaging (MRI) examination A and B: Axial T2w and C: coronal T1w with gadolinium images demonstrated diffuse thickening of the gastric wall at the level of the pylorus. The positron emission tomography-computed tomography (PET-CT) scan D and E: Axial and F: coronal whole - body PET-CT fusion images as part of the staging process revealed a hypermetabolic mass in the pyloric antrum with an SUV max of 21,6. There was also an enlarged hypermetabolic lymph node on the inferior surface of the hypermetabolic lesion. There were no other hypermetabolic findings.
also an enlarged hypermetabolic lymph node on the inferior surface of the hypermetabolic lesion. There were no other hypermetabolic findings.
Bone marrow aspiration revealed infiltration (<5%) by neoplastic lymphocytes. The disease classified as stage III without CNS involvement. The patient stratified into Group R2, according to the staging of the disease and received treatment according to the B-NHL 2013 protocol. At the last follow-up, the patient was asymptomatic with weight gain. Follow-up endoscopy 12 months after completion of treatment revealed resolution of the lesions (Figure 1 D,E,F), accompanied by complete regression of the histologic (Figure 2 E and F) and radiologic abnormalities. Consent form from parents was obtained for anonymised publication of the patient’s history and images of endoscopic, histological and radiological findings.
Discussion
Burkitt lymphoma is a highly aggressive B-cell NHL characterized by translocation and deregulation of the MYC gene on chromosome 8 [9]. There are three distinct clinical forms of BL: endemic (African), sporadic (non-endemic) and immunodeficiency-associated. Although they are histologically identical and have similar clinical behavior, there are differences in epidemiology, clinical presentation, and genetic features between the three forms of BL [10]. The exact worldwide incidence of BL is not known. The sporadic variant occurs in the United States and Western Europe. Burkitt lymphoma accounts for 30%of pediatric lymphomas and <1% of adult NHL in the United States [8]. In Europe, the incidence is approximately 2.2 cases per million people per year [11]. A study examining primary pediatric gastrointestinal lymphomas concluded that they are very rare in the pediatric population and are more common in Whites and males, with BL most commonly located in the small intestine [12]. Burkitt lymphoma accounts for about 25–30% of NHL in children presenting with an abdominal tumor. In most cases, the tumor is in the ileum or cecum, and those with primary gastric tumor are rare [13]. Primary gastric lymphoma accounts for 3% of all gastric cancers in adults and only 1.48-2% in children [5]. Symptoms may include abdominal pain, weight loss, constipation, vomiting and anemia [14]. It should be noted however, that all of the above symptoms are non-specific, so diagnosis may be delayed. The diagnosis includes endoscopy, histology and radiologic examination. Gastric Burkitt lymphoma is characterized histologically by a classic "starry sky" appearance, resulting from numerous macrophages (the "stars") scattered among a dense population of monomorphic, medium-sized neoplastic lymphoid cells (the "sky"). This pattern arises due to the tumor’s high mitotic and apoptotic activity, with macrophages phagocytosing apoptotic debris. The tumor cells display round nuclei, coarse chromatin, multiple small nucleoli, and deeply basophilic cytoplasm often containing vacuoles, especially on cytologic smears. The Ki-67 proliferation index approaches 100%, reflecting the tumor’s aggressive nature. Cells are tightly packed with scant cytoplasm, forming sheets without significant architectural pattern, and show diffuse infiltration of the gastric tissue rather than forming follicles or nodules. Immunohistochemically, the cells are positive for CD20, CD10, and BCL6, negative for BCL2, and show a very high Ki-67 index. Genetically, the tumor is defined by a MYC gene translocation, most commonly t(8;14) (q24;q32), which drives uncontrolled cellular proliferation [15]. All these findings were found in our patient. Occasional case reports suggest that gastric BL is strongly associated with HP infection. However, the relationship between HP and gastric BL in children remains unclear. Some studies suggest a possible association [5,16], while others do not [14]. The association between gastric cancer and HP infection is well known, and chronic gastritis caused by HP is associated with low-grade gastric lymphoma arising from mucosa- assisted lymphoid tissue. Furthermore, this low-grade lymphoma sometimes progresses to high-grade lymphoma [6]. Although there are few reports suggesting a relationship between HP infection and gastric NHL, there are currently no experimental data to support such an association [14]. The immune response to CagA or other HP proteins, which might lead to the development of high-grade lymphoma, has been suggested as a mechanism for this association [17]. A case report of a patient with BL and HP infection, reported that the patient responded well to chemotherapy without HP eradication treatment [18]. In our patient although there was some evidence of possible H. Pylori infection the diagnosis could not be justified according to the ESPGHAN guidelines [7]. Patient was successfully treated only with chemotherapy without HP eradication. Of note, no signs of HP gastritis were found on subsequent endoscopies. Chemotherapy with multi- agent regimes, is the first-line therapy for inducing remission in BL. Recently, monoclonal antibodies have been used in first line treatment in BL. The anti-CD20 monoclonal antibody rituximab has been used in combination with chemotherapy for the treatment of BL, where it has shown improvement in survival by over 95% [19]. Surgical intervention is not indicated. However, there are some serious complications such as tumor lysis syndrome or chemotherapy-associated toxicities. Diagnosis is confirmed by biopsy of a specific disease site or lymph node. The system that is still used for BL classification is the Ann Arbor or the St Jude/Murphy staging system, extending from I to IV [Sandlund, J.T. Burkitt lymphoma: Staging and response evaluation. Br. J. Haematol. 2012, 156, 761-765. [CrossRef]]. BL is fatal if left untreated. Prognosis depends on the extent of the disease, the patient’s age, and the timing of diagnosis, described as excellent for the early/moderate stages (survival rate reaching 97–98%), while in the advanced stages (III or IV) it drops to 87.3% [20]. The features associated with an adverse outcome include older age, advanced stage, poor performance status, bulky disease, high lactate dehydrogenase (LDH), and central nervous system (CNS) or bone marrow involvement [21]. In a recent study, four factors were identified as independently prognostic for patients’ outcomes: age ≥ 40 years, LDH > 3× normal, Eastern Cooperative Oncology Group Performance Status (ECOG PS) ≥ 2, and CNS involvement [22].
Conclusions
BL is an aggressive B cell lymphoma, but promptly diagnosed, it rapidly responds to treatment and exhibits a satisfactory long-term prognosis. In the case presented here, the most clinically significant diagnostic aspect was the fact that the first manifestations were in the stomach, presenting with signs and symptoms that mimicked common gastritis. Following initial attempts to alleviate the patient’s symptoms appropriate referral to a specialized medical doctor and immediate diagnostic work-up, both imaging and microscopic, was virtually life-saving; it ensured establishing the correct diagnosis and initiating the appropriate chemotherapy at the right time for such an aggressive and rapidly progressing neoplasm. Our patient completed his treatment with prompt response, without major complications. In conclusion, primary gastric BL is an extremely rare disease in children. The symptoms are nonspecific, with abdominal pain with or without vomiting being prominent. Upper gastrointestinal endoscopy plays a significant role in the diagnosis and follow- up of these patients. Chemotherapy is the treatment of choice. Close monitoring during treatment and surveillance following its completion are mandatory; follow-up is recommended every 2–3months with thorough clinical examination, imaging studies, and blood investigation. Further investigations are needed to determine the link between HP infection and BL.
Acknowledgments:
None
Conflict of Interest Disclosures (includes financial disclosures):
The authors have no conflict of interest to declare.
Funding/Support:
No funding was secured for this study.
Article Summary:
A 14.5 -year-old boy presented with vomiting and epigastric pain and was diagnosed with primary Burkitt gastric lymphoma a very rare condition in childhood. Informed consent was obtained to submit the patient's anonymized data for publication.
Contributors Statement Page:
Dr. Maria Rogalidou conceptualized and designed the study, drafted the initial manuscript, and contributed to its review and revision. Prof Kattamis and Prof. Alexandra Papadopoulou critically reviewed the manuscript. Dr Kalliopi Stefanaki and Amalia Patereli were the pathologists interpreted the histological
findings. Dr. Georgia Avgerinou, Maria Gavra, and Dr Maria Rogalidou supervised and coordinated data collection related to imaging studies and endoscopy & pathology findings, while also critically reviewing the manuscript. All authors have approved the final version of the manuscript as submitted and take full responsibility for all aspects of the work.
References
- Alexander DD, Mink PJ, Adami HO, et al. The non- Hodgkin lymphomas: a review of the epidemiologic Int J Cancer 12 (2007): 1-39.
- Kalisz K, Alessandrino F, Beck R, et An update on Burkitt lymphoma: a review of pathogenesis and multimodality imaging assessment of disease presentation, treatment response, and recurrence. Insights Imaging 10 (2019): 56.
- Bandyopadhyay R, Sinha SK, Chatterjee U, et Primary pediatric gastrointestinal lymphoma. Indian J Med Paediatr Oncol 32 (2011): 92-95
- Choe BK, Kim JY, Hwang JB, et al. A Case of Primary Gastric Lymphoma in a Child. J Pediatr Hematol Oncol 28 (2006): 296–299
- Moschovi M, Menegas D, Stefanaki K, et al. Primary Gastric Burkitt Lymphoma in Childhood: Associated with Helicobacter pylori? Med Pediatr Oncol 41 (2003): 444-447.
- Kim SC, Hwang JW, Lee MK. Rare Case of Primary Gastric Burkitt Lymphoma in a Korean J Gastroenterol 68 (2016): 87-92
- Matjaž Homan, Nicola L Jones Patrick Bontems, Matthew W Carroll, et al. On behalf of ESPGHAN/NASPGHAN, Updated joint ESPGHAN/NASPGHAN guidelines for management of Helicobacter pylori infection in children and adolescents J Pediatr Gastroenterol Nutr 79 (2024): 758-785.
- Zheng N, Xiao XM, Dong KR, et al. Primary gastric tumors in infants and children: 15 cases of 20 year J Cancer Res Clin Oncol 142 (2016): 1061-1067.
- Alaggio R, Amador C, Anagnostopoulos I, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia 36 (2020): 17-20.
- Morton LM, Wang SS, Devesa SS, et al. Lymphoma incidence patterns by WHO subtype in the United States, 1992-2001. Blood 107 (2006): 107-265.
- Sant M, Allemani C, Tereanu C, et Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood 116 (2010): 3724-3734.
- Sant M, Allemani C, Tereanu C, et Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood 116 (2010): 372-3734.
- Link MP, Weinstein Malignant non-Hodgkin lymphomas in children. In: Pizzo PA, Poplack DG (eds) Principles and practice of pediatric oncology. Lippincott JB, Philadelphia(2006): 722-774
- Kupeli S, Varan A, Demir H, et Association of Helicobacter pylori and childhood lymphoma. J Pediatric Hematol Oncol 29 (2007): 301-304.
- Derqaoui S, Boujida I, Marbouh O, et al. NonHodgkin Lymphoma Among Children: Pathological Aspects and Diagnostic Clin Pathol (2022).
- Ruan W, Febo-Rodriguez L, Daignault C, et Endoscopic ultrasound-guided diagnosis of Helicobacter pylori-associated gastric Burkitt's lymphoma in an adolescent patient: a rare case. Clin J Gastroenterol 14 (2021): 88-91.
- Kuo SH, Chen LT, Lin CW, et Detection of the Helicobacter pylori CagA protein in gastric mucosa- associated lymphoid tissue lymphoma cells: clinical and biological significance. Blood Cancer J 3 (2013): e125.
- Sharon N, Kenet G, Toren A, et al. Helicobacter pylori- associated gastric lymphoma in a girl. Pediatr Hematol Oncol 14 (1997): 177-180.
- Kalisz K, Alessandrino F, Beck R, et An update on Burkitt lymphoma: a review of pathogenesis and multimodality imaging assessment of disease presentation, treatment response, and recurrence. Insights Imaging 10 (2019): 56.
- Minard-Colin V, Aupérin A, Pillon M, et al. Rituximab for High-Risk, Mature B-Cell Non-Hodgkin's Lymphoma in N Engl J Med 382 (2020): 2207-2219.
- Patte C, Auperin A, Michon J, et al. Highly effective multiagent chemotherapy tailored to the tumor burden and initial response in 561 unselected children with B-cell lymphomas and L3 leukemia. Blood 97 (2001): 3370-
- Evens AM, Danilov A, Jagadeesh D, et Burkitt lymphoma in the modern era: real-world outcomes and prognostication across 30 US cancer centers. Blood 137 (2021): 374-386.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 