Regenerative Protocol for Knee Degeneration: A Case Study with Five-Year Follow-Up
Kenneth Russ1, Philip Yoo1, Naomi Lambert2*, Alexis Lee2, John Shou2 and Tyler Barrett2
121st Century LaserSTEM Regenerative Medicine Institute, USA
2Regenative Labs, USA
*Corresponding author: Naomi Lambert, Regenative Labs, USA Email: naomi@regenativelabs.com; Tel.: +1800-891-3452
Received: 20 June 2025; Accepted: 24 June 2025; Published: 04 July 2025
Article Information
Citation:
Kenneth Russ, Philip Yoo, Naomi Lambert, Alexis Lee, John Shou and Tyler Barrett. Regenerative Protocol for Knee Degeneration: A Case Study with Five-Year Follow-Up. Archives of Clinical and Biomedical Research. 9 (2025): 275-279.
View / Download Pdf Share at FacebookAbstract
Background/Objectives: Knee osteoarthritis (OA) is a progressive and disabling musculoskeletal disorder characterized by the degeneration of joint cartilage, leading to reduced range of motion and diminished quality of life. Globally, knee OA is estimated to account for approximately 80% of all osteoarthritis cases. The current standard of care is to provide conservative treatment with medication and lifestyle changes, but when they fail, surgical intervention may be required. Approximately 69% of patients with knee OA undergo total knee replacement surgery. Methods: The patient in this case study is an 85-year-old female who failed standard conservative care, presenting with advanced knee OA, poor posture, and an antalgic gait. The patient opted for regenerative medicine-focused care prior to seeking surgical intervention. The protocol included several regenerative therapies, pulsed electromagnetic field therapy (PEMF), myofascial release therapy, red lightemitting diode treatment (red light therapy), and a connective tissue transplant with a Wharton’s jelly tissue allograft. Results: Prior to treatment, the patient reported extreme pain. At the 3-month follow-up, she noted substantial pain reduction, and by the 12-month mark, reported complete resolution of pain. At a 5-year follow-up, the patient continued to report the absence of knee pain. Conclusions: This study observes the sustained improvement in pain and functional outcomes following a multimodal care approach. Aligning complementary regenerative protocols to target root causes instead of focusing on symptom management could improve outcomes-based care practices and should be further studied.
Keywords
<p>Whartons Jelly; Knee OA; Regenerative Medicine; Cartilage Degeneration</p>
Article Details
1. Introduction
Osteoarthritis (OA) is one of the most common rheumatologic disorders. The global prevalence of symptomatic OA is estimated at 240 million individuals, 10% of men and 18% of women 60 years or older [1]. Specifically, knee OA accounts for four-fifths of all known OA cases worldwide and is projected to rise exponentially [2]. By 2050, the global population of individuals suffering from knee OA is estimated to be 642 million [3]. Knee OA significantly decreases the quality of life in an individual, causing them to be more susceptible to sedentary lifestyles, which are detrimental to aging adults. Risk factors for knee OA include a higher BMI index, being over 40 years of age, a history of knee trauma, and being female gender [4]. Identification of these risk factors and symptoms related to knee OA is critical for proper clinical care. The standard of care currently consists of conservative symptom management with injectable steroids or medication, followed by surgical intervention. Approximately 69% of patients with knee OA undergo total knee replacement surgery [5]. Recently, there has been an increase in research dedicated to finding alternative noninvasive therapies to combat the rising number of OA cases each year. Regenerative medicine, a term coined in 1999 by William Haseltine, is one such popular approach to alternative medicine [6]. The goal of regenerating or replacing damaged tissue is a paradigm shift from primarily symptom management.
Regenerative therapies can include methods that reduce inflammation and promote overall tissue health, like photobiomodulation (PBMT) with laser and light therapies or pulse electromagnetic field (PEMF) therapy. The application of PBMT has shown positive results in patients suffering from diabetic ulcers, neck issues, and neurocognitive challenges linked to aging; findings from a 2023 study revealed that PBMT is particularly effective in addressing knee osteoarthritis, notably in its early stages [7]. PEMF therapy provides technological advances in pain reduction, targeting unaddressed knee muscle weakness. A randomized control trial using PEMF therapy in knee OA patients reported significant drops in pain [8]. Additionally, myofascial release techniques (MRT) can increase the range of motion in patients with knee OA. In a study by Antohe (2024), it was noted that there is a direct connection between the use of MRTs and a patient’s range of motion, suggesting that an increase in motion range is improved through MRTs [9]. Other regenerative therapies, such as platelet-rich plasma (PRP) and intra-articular hyaluronic acid injections (IA-HA) have been introduced to help with the prevention and symptom management of knee OA. However, despite the growing popularity of these therapies, current literature does not provide substantial evidence of positive outcomes. According to a 2020 IA-HA study by Miyazaki and a 2023 PRP study by Shahid, there is no significant difference between the placebo and test groups [10,11]. Further research is needed to determine the best practices for incorporating regenerative techniques into the standard care of knee OA.
Direct tissue supplementation with donated, autologous, or synthetic homologous connective tissues is another facet of regenerative medicine. Wharton’s jelly (WJ) is a connective tissue in the umbilical cord, comprising collagen types I, III, and V, along with growth factors, hyaluronic acid, cytokines, and proteoglycans, crucial for the repair and supplementation of the connective tissue [12]. The composition of Wharton’s jelly resembles that of human cartilage, being predominantly made up of collagen type I, with lesser proportions of types III and V [13]. Intra-articular cartilage serves to relieve pressure while minimizing deformation, harm, and friction; in comparison, WJ provides cushioning and support for the umbilical vasculature to prevent harm from torque, tension, and external forces [14]. The 2022 study by Davis observes promising results for the application of WJ to knee OA. From this retrospective study, a significant number of individuals reported increased overall functionality and joint mobility [15]. Using multiple regenerative practices together can improve overall patient outcomes; though many practices implement this methodology already, the literature is lacking. This case study outlines a regenerative-based protocol on an 85-year-old female patient with grade 4 Knee OA.
2. Materials and Methods
Patient description
85-year-old female presenting with lower back, knee, foot, and general leg pain on the left side. The patient has arthritis and poor posture with an antalgic gait. This case study covers the modalities used to address the patient’s complaints about her left knee.
Case history
The patient previously received a cortisone injection and three rounds of hyaluronic acid with no relief. The patient was recommended for total knee replacement but declined surgical intervention.
Physical examination results
At the initial visit on 11/13/2018, the patient reported a VAS(visual analog scale) score of 10, and the temperature in the left knee registered at 88.7 degrees Fahrenheit.
Results of pathological tests and other investigations
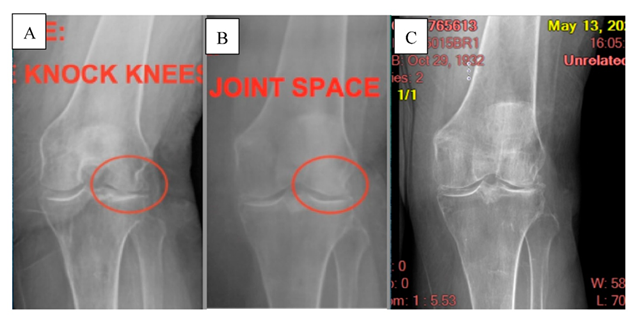
The patient received an initial X-ray on 6/25/18 showing bone-on-bone loss of cartilage space on the lateral side of both knees with genu valgus.
Patient Care Plan
Beginning on 11/13/2018, the patient received the following therapies 6 times over two weeks, concluding on 11/27/2018: 250-watt Cold laser Therapy, PEMF, Myofascial release therapy, and red light therapy. On 12/11/2018, the patient received a 2cc intra-articular application, 1cc of 1 to 24 dilution suspended WJ tissue allograft mixed with 1cc sodium bicarbonate 5%. The application was done laterally at the highest point of inflammation, 88.7 vs. 80 medially. Immediately following the application, the patient received 250-watt Cold laser Therapy, Pulsed electromagnetic field, Myofascial release therapy, and red light therapy. The patient then received two final rounds of the same aforementioned laser, PEMF, myofascial release, and red light therapies, one month and three months after the WJ application. The patient had at-home instructions to incorporate a keto diet, drink alkaline water, and apply a 30-minute daily at-home light diode panel.
3. Results
The patient reported a VAS score of 10 at the first visit and a score of 2 one month later at the WJ application visit, but noted little to no functionality improvement. At the three-month visit following the WJ application, the patient reported a 90% pain improvement and an 85% improvement in functionality of the joint. Six months following the WJ application, a follow-up X-ray was conducted, showing improved cartilage space. Twelve months following the WJ application, the patient reported a VAS score of zero. The five-year x-ray shows 50% medial / 100% distal joint space degradation, which is still an improvement from the initial state, but additional WJ tissue supplementation may be beneficial. At the five-year follow-up, the patient reported no pain and had maintained full functionality of the affected knee.
Figure 1A: The first X-ray taken on 6/25/18 shows bone-on-bone loss of cartilage space. B: The second X-ray taken on 6/26/19, six months after the WJ allograft placement, shows improved cartilage space. C: The final X-ray was taken on 5/13/24 at the five-year follow-up. Some continued degeneration of the cartilage space is shown, but the patient did not experience decreased functionality.
4. Discussion
Incorporating regenerative medicine into patient care requires a shift in focus to the root causes of pain in the specified disorder. In the case of knee OA, hypertrophic changes in the bone cause cartilage thinning and deterioration across the joint, leading to inflammation, swelling, stiffness, and pain [16]. Knee OA can not be repaired unassisted because repetitive adverse forces on the knee cause synovial macrophages and then local chondrocytes, osteocytes, and fibroblasts to dysregulate and stop the normal healing and repair process [17]. Chronic inflammation advances tissue degeneration, causing pain and decreased functionality of the joint. The combination of regenerative practices in this protocol aims to combat both inflammation and tissue degeneration.
Light, laser, electric, and massage therapies were implemented before and after tissue supplementation with Wharton’s Jelly. Beginning with myofascial release therapy (MRT), the patient received trigger point massage to improve range of motion, pain, and electrical muscle activity [18]. Following the MRT, the patient received red light therapy, also known as photobiomodulation therapy. A comprehensive review of the mechanisms and efficacy of PBM by Zhang in 2023 concluded that PBM reduces pain, swelling, and stiffness in patients with OA by promoting cell activity and functional normalization by regulating a number of cellular responses, including promoting mitochondrial ATP production, releasing intracellular nitric oxide, and regulating immune cell secretion of inflammatory cytokines [19]. Following PBM, the patient received class 4 laser therapy, which has been shown to be an effective modality in the treatment of patients with knee OA pain based on its analgesic, anti-inflammatory, and anti-edematous properties [20]. The patient then received PEMF therapy, which, in recent studies, has been reported to result in a reduction in pain and improvement in function [21]. The combination of these therapies aims to reduce patients’ inflammation and pain as well as regulate and normalize the biochemical processes occurring in an arthritic knee.
A WJ connective tissue allograft was used to address tissue loss in the joint space. The allograft comes from the connective tissue in human umbilical cords. The graft was purchased from Regenative Labs (Pensacola, FL, USA), which uses minimal manipulation processing according to the FDA’s 361 guidelines for tissue processing to ensure the connective tissue maintains its structural integrity post-processing [22]. WJ’s primary function in the umbilical cord is cushioning and protecting. When used alone to replace intraarticular cartilage, it has shown significant improvements in patient pain scales for multiple musculoskeletal locations such as hip, SI, and knees [23,24,25]. While the literature on WJ connective tissue allografts still requires additional randomized trials for dosing protocol development, the information available shows promising results for regenerative medicine.
5. Conclusions
The use of WJ tissue allografts alongside other regenerative practices, such as laser and light therapies, could maximize patient outcomes for musculoskeletal issues like those presented in this study. Recent literature on individual regenerative methods shows positive results. Aligning complementary regenerative protocols to target root causes instead of focusing on symptom management could improve outcomes-based care practices and should be further studied.
Author Contributions
Conceptualization, K.R.,P.Y. and T.B.; methodology, K.R., P.Y; software, T.B., J.S.; validation, N.L., A.L. and T.Y.; formal analysis, N.L., A.L.; investigation, K.R.,P.Y.; resources, N.L., A.L.; data curation, P.Y.; writing—original draft preparation, P.Y., N.L., A.L.; writing—review and editing, R.P., N.L., A.L.; visualization, K.R.,P.Y., N.L.; supervision, J.S., T.B.; project administration, T.B.; funding acquisition, K.R.,P.Y., T.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Acknowledgments
The authors would like to thank the staff at 21st Century Laser STEM Regenerative Medicine Institute for their contribution to data collection and filing.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
|
MDPI |
Multidisciplinary Digital Publishing Institute |
|
DOAJ |
Directory of open access journals |
|
OA |
Osteoarthritis |
|
PEMF |
Pulsed Electromagnetic Field Therapy |
References
- Allen KD, Thoma LM, Golightly YM. Epidemiology of osteoarthritis. Osteoarthritis Cartilage. 30 (2022): 184-195.
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. Published 2020 Nov 26.
- GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990-2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol 5 (2023): e508-e522.
- Dong Y, Yan Y, Zhou J, Zhou Q, Wei H. Evidence on risk factors for knee osteoarthritis in middle-older aged: a systematic review and meta analysis. J Orthop Surg Res 18 (2023): 634.
- Wang CC, Huang KC, Ku MC, Pan CC, Hsieh CP, Chang IL, Tzeng CY, Chen CP, Lee YH, Chen YJ, Tsai YS, Kung PT, Chou WY, Tsai WC. Factors influencing the decision to receive total knee replacement among patients with severe knee osteoarthritis under universal health insurance coverage. Sci Rep 14 (2024): 30028.
- Sampogna G, Guraya SY, Forgione A. Regenerative medicine: Historical roots and potential strategies in modern medicine. J Microsc Ultrastruct 3 (2015): 101-107.
- Zhang Y, Ji Q. Current advances of photobiomodulation therapy in treating knee osteoarthritis. Front Cell Dev Biol. 2023;11:1286025.
- Wang QW, Ong MT, Man GC, et al. The effects of pulsed electromagnetic field therapy on muscle strength and pain in patients with end-stage knee osteoarthritis: a randomized controlled trial. Front Med (Lausanne) 11 (2024): 1435277.
- Antohe BA, Alshana O, Uysal HS, Rata M, Iacob GS, Panaet EA. Effects of Myofascial Release Techniques on Joint Range of Motion of Athletes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sports 12 (2024): 132.
- Miyazaki T, Sakamoto T, Aoki N, Nakajima H, Oki H, Matsumine A. Does hyaluronic acid injection prevent the progression of knee Osteoarthritis ? Osteoarthritis and Cartilage 28 (2020): S500.
- Shahid A, Malik A, Bukhari A, Shaikh A, Rutherford J, Barkatali B. Do Platelet-Rich Plasma Injections for Knee Osteoarthritis Work?. Cureus 15 (2023): e34533.
- Gupta A, El-Amin SF 3rd, Levy HJ, Sze-Tu R, Ibim SE, Maffulli N. Umbilical cord-derived Wharton’s jelly for regenerative medicine applications. J Orthop Surg Res 15 (2020): 49.
- Ouyang Z, Dong L, Yao F, et al. Cartilage-Related Collagens in Osteoarthritis and Rheumatoid Arthritis: From Pathogenesis to Therapeutics. Int J Mol Sci. 24 (2023): 9841.
- Lin L, Xu Y, Li Y, et al. Nanofibrous Wharton’s jelly scaffold in combination with adipose-derived stem cells for cartilage engineering. Materials & Design 186 (2020): 108216.
- Davis JM, Sheinkop MB, Barrett TC. Evaluation of the Efficacy of Cryopreserved Human Umbilical Cord Tissue Allografts to Augment Functional and Pain Outcome Measures in Patients with Knee Osteoarthritis: An Observational Data Collection Study. Physiologia. 2 (2022): 109-120.
- Goodman S. Osteoarthritis. In: Yee A, Paget S, eds. Expert Guide to Rheumatology. Philadelphia, Pa.: American College of Physicians; 2005:269–283.
- Huston P. Why osteoarthritis of the knee is called "a wound that does not heal" and why Tai Chi is an effective treatment. Front Med (Lausanne) 10 (2023): 1208326.
- E Silva DCCM, de Andrade Alexandre DJ, Silva JG. Immediate effect of myofascial release on range of motion, pain and biceps and rectus femoris muscle activity after total knee replacement. J Bodyw Mov Ther 22 (2018): 930-936.
- Zhang R, Qu J. The Mechanisms and Efficacy of Photobiomodulation Therapy for Arthritis: A Comprehensive Review. Int J Mol Sci 24 (2023): 14293.
- Bettencourt F (2020) Effects of Class IV Laser in Knee Osteoarthritis: A Randomized Control Trial. J Arthritis 9: 289.
- Bagnato GL, Miceli G, Marino N, Sciortino D, Bagnato GF. Pulsed electromagnetic fields in knee osteoarthritis: a double blind, placebo-controlled, randomized clinical trial. Rheumatology (Oxford) 55 (2016): 755-762.
- Davis JM, Purita JR, Shou J, Barrett TC. Three-Dimensional Electron Microscopy of Human Umbilical Cord Tissue Allograft Pre and Post Processing: A Literature Comparison. J Biomed Res Environ Sci. 2022 Aug 15; 3(8): 934-940. Article ID: JBRES1535, Available at: https://www.jelsciences.com/articles/jbres1535.pdf.
- Lai, A., Tamea, C., Shou, J., Okafor, A., Sparks, J., Dodd, R., Lambert, N., Woods, C., Schulte, O., Kovar, S., & Barrett, T. Retrospective Evaluation of Cryopreserved Human Umbilical Cord Tissue Allografts in the Supplementation of Cartilage Defects Associated with Hip Osteoarthritis. Journal of Clinical Medicine, 13 (2024): 4040.
- Lai, A., Shou, J., Traina, S. A., & Barrett, T. The Durability and Efficacy of Cryopreserved Human Umbilical Cord Tissue Allograft for the Supplementation of Cartilage Defects Associated with the Sacroiliac Joint: A Case Series. Reports 6 (2023): 12.
- Timmons RB, Sugaya K, Bane LD. Homologous Use of Allogeneic Umbilical Cord Tissue to Reduce Knee Pain and Improve Knee Function. Life (Basel) 12 (2022): 260.
Related PubMed Articles
- International Delphi Consensus on Medial Meniscal Root Tears Shows High Agreement on Diagnosis, Treatment, and Rehabilitation but Lack of Agreement on Treatment of Asymptomatic Tears.
- Novel Collagenous Sponge Composites for Osteochondral Regeneration in Rat Knee Models: A Comparative Study of Keratin, Hydroxyapatite, and Combined Treatments.
- Mucoid Degeneration of Anterior Cruciate Ligament-A Systematic Approach for Debulking.
- A New Approach to Postoperative Rehabilitation following Mosaicplasty and Bone Marrow Aspiration Concentrate (BMAC) Augmentation.
- Biomechanics of the Human Osteochondral Unit: A Systematic Review.
- Study protocol for a randomised placebo controlled trial of platelet-rich plasma injection to prevent post-traumatic knee osteoarthritis after anterior cruciate ligament reconstruction.
- Alleviation of osteoarthritis by intra-articular transplantation of circulating mesenchymal stem cells.
- Systematic study of single-cell isolation from musculoskeletal tissues for single-sell sequencing.
- Stem cells in degenerative orthopaedic pathologies: effects of aging on therapeutic potential.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 