Selected Unique Clinical Shoulder Signs as Visualized by MRI
Caldon Jayson Esdaille1,2,3, Daniel Marrero9, Cato T Laurencin2,3,4,5,6,7,8 *
1Howard University College of Medicine, Washington, DC
2Connecticut Convergence Institute for Translation in Regenerative Engineering, University of Connecticut Health Center, Farmington, CT
3Department of Orthopaedic Surgery, University of Connecticut Health, Farmington, CT, USA
4Raymond and Beverly Sackler Center for Biomedical, Biological, Physical and Engineering Sciences, University of Connecticut Health, Farmington, CT, USA
5Department of Chemical and Biomolecular Engineering, University of Connecticut, Storrs, CT, USA
6Department of Biomedical Engineering, University of Connecticut, Storrs, CT, USA
7Department of Materials Science and Engineering, University of Connecticut, Storrs, CT, USA
8Institute of Materials Science, University of Connecticut, Storrs, CT, USA
9University of Connecticut Health Center, Department of Musculoskeletal Radiology, Farmington CT
*Corresponding Author: Cato T Laurencin, MD PhD, Connecticut Convergence Institute for Translation in Regenerative Engineering, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT, USA
Received: 16 March 2021; Accepted: 23 March 2021; Published: 02 July 2021
Article Information
Citation: Caldon Jayson Esdaille, Daniel Marrero, Cato T Laurencin. Selected Unique Clinical Shoulder Signs as Visualized by MRI. Journal of Orthopaedics and Sports Medicine 3 (2021): 102-115.
View / Download Pdf Share at FacebookAbstract
Shoulder pain is a common musculoskeletal complaint that if severe enough, can contribute significantly to morbidity due to its debilitating and often disabling nature which may leave patients unable to perform activities of daily living. Various etiologies of shoulder pain exist which present with clinical signs and symptoms based on the source of the pathology. Although most shoulder injuries can be diagnosed with a detailed history and physical exam, magnetic resonance imaging (MRI) has become a well-established technique for confirming pathology of the shoulder due to its high diagnostic accuracy. The ability to visualize soft tissue as well as bone morphology has allowed it to become widely utilized across all specialties that manage shoulder pathology; especially in orthopaedics. Radiologists that interpret MR images often describe changes to normal anatomy by utilizing terms that have been well studied and published throughout radiology literature. These terms are referred to as “signs” and are used to assist in diagnosis of a disease by correlation with clinical symptoms. These signs are a key component of the fundamental core of musculoskeletal radiology but are not often discussed or utilized in the field of orthopaedics to assist with a diagnosis. This manuscript will discuss and review the presentation of a selection of unique clinical signs of shoulder pathology that are identifiable with MRI as well as how they are described by musculoskeletal radiologists. The signs discussed within this manuscript are unique due to the fact that although they are more published throughout musculoskeletal radiology literature when compared to orthopaedic surgery and sports medicine literature.
Keywords
<p>Double axillary pouch sign; Double oreo cookie sign; Geyser sign; GLOM sign; J-sign; Subcoracoid triangle sign; Tangent sign</p>
Article Details
1. Introduction
Musculoskeletal complaints and impairments comprise a large portion of health care visits in the United States of America, with increasing prevalence in the older population. These disorders affect society by increasing morbidity, long term disability and increasing healthcare costs as a patient’s age increases [1]. The prevalence of musculoskeletal pain varies across studies due to a multitude of factors which include definitions of pain and time periods analyzed. However, there are consistencies across a few studies that show an increased prevalence of musculoskeletal pain amongst older individuals and persons of lower socioeconomic status [2].
Shoulder pain is a common complaint that most physicians who manage musculoskeletal disease will encounter. According to surveys, shoulder pain is present in approximately 18-26% of adults at any point in time [3]. Shoulder pain carries significant morbidity and can become a disabling disease that prohibits individuals from performing their activities of daily living. A variety of occupational and psychosocial factors play a role in the debilitating process as some activities such as repetitive and excessive overhead motion carry increased risk for development of shoulder pathology [4-6].
Although the shoulder is extraordinarily flexible with several planes of motion and able to withstand heavy physical demands, the complex composition of articulating bones, muscles, tendons and ligaments both inside and outside of the joint capsule requires all components to be working synonymously. There is potential for malfunction in each of the various parts of the shoulder and the following patho-anatomical subcategories of shoulder pathology have been adapted: Rotator cuff disease, biceps tendon disease, acromioclavicular joint abnormalities and adhesive capsulitis [3]. These subcategories are not all inclusive but most diagnoses of shoulder pathology fall into one of these areas.
Although most shoulder conditions can be diagnosed clinically after a detailed history, observation and physical examination, the use of imaging techniques plays a key role in confirming the diagnosis. Plain radiographs are usually first line in cases of acute injury, but Magnetic resonance imaging (MRI) is often utilized for evaluation of the soft tissue of the joint if pathology of these structures is suspected. The contrast between soft tissue and bones across different planes allows for optimal assessment of muscles, tendons, ligaments, hyaline and fibrous cartilage, joint capsules, fat and bursa.
MRI has high diagnostic value for various forms of pathology that are visible on arthroscopy and can be a useful tool in ruling out abnormalities of the shoulder joint [6, 7]. The most common indications for shoulder MRI include but are not limited to rotator cuff tears, shoulder instability, osteonecrosis, neoplasm, infection and subtle fractures or erosive changes [8]. Each of these conditions have clinical as well as radiographic signs that are common in presentation amongst patients with similar etiologies of shoulder pain.
Radiologists often use certain descriptions of the anatomical, physiological and pathological structures that they encounter in order to establish a pattern of disease presentations. These descriptions normally utilize a metaphor that will indicate a specific pathology and have become an integral part of the nomenclature for each subspeciality of radiology. This allows for patterns of disease and injury to become more easily identified [9]. Musculoskeletal imaging is no different, which has become a diagnostic tool for a variety of specialties such as Orthopedic Surgery, Rheumatology, Family Medicine, Physiatry, Pediatrics and Pain Management. Therefore, it is essential to be familiar with the terminology used by trained musculoskeletal radiologists in their interpretation of an image [10].
The purpose of this review paper is to discuss a selection of unique clinical signs of shoulder pathology that are identifiable with MRI. In this manuscript, the pathophysiology of the shoulder joint abnormality will be reviewed, as well as how it is visualized on MRI and a description of the radiographic signs accompanying the pathology that have been published throughout the radiology literature. The signs discussed within this manuscript are unique due to the fact that although they are published more throughout in the musculoskeletal radiology literature when compared to orthopaedic surgery and sports medicine literature.
2. Review of the Literature
A comprehensive list of MRI signs of shoulder pathology was compiled and cross-referenced with the literature available on PubMed and Google Scholar. Signs that were published in musculoskeletal radiology literature and were not frequently mentioned in orthopaedic or sports medicine literature were deemed unique and appropriate for the scope of this paper. The unique signs were chosen to be described in this review paper.
3. Double Axillary Pouch Sign
The glenoid labrum is composed of redundant, folded fibrocartilage that attaches to the rim of the glenoid of the scapula. It allows for articulation with the head of the humerus and provides stability by inhibiting anterior and posterior translation that may occur with normal movement [11]. Once a sufficient force has been applied to the shoulder to disrupt this articulating surface, a subluxation or dislocation may occur which can injure the labrum in the process. A tear of the anterior inferior labroligamentous complex of the labrum from the glenoid is classically defined as a cartilaginous Bankart lesion. The glenohumeral (GH) ligaments remain attached to humeral head and avulses the labrum from the anterior inferior portion of the glenoid rim which produces the tear. This injury may also lead to periosteal elevation and/or stripping of the joint capsule [12-14]. This commonly occurs in patients who have had a traumatic shoulder dislocation or recurrent subluxations and/or dislocations due to glenohumeral instability and joint laxity [14].
The axial plane of MR imaging is the primary method for evaluation of anterior and posterior labral pathology but additional information can be provided on coronal planes to confirm the diagnosis. In a coronal oblique T1 weighted MRI of an individual with a normal anatomy an axillary pouch exists between the anterior and posterior band of the inferior glenohumeral ligament and lies within the glenohumeral (GH) joint.
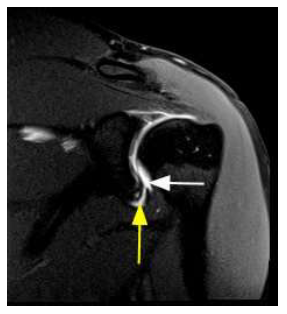
Figure 1: Double Axillary Pouch Sign. Coronal oblique T1 weighted fat saturated magnetic resonance imaging of a patient with an anterior inferior labral tear. The white arrow depicts fluid within the axillary pouch which is a normal finding. The yellow arrow depicts additional fluid undercutting the chondrolabral junction along an anterior inferior labral tear and accumulating between the torn anterior inferior glenoid labrum and the glenoid rim. This accumulation of fluid gives the appearance of a second axillary pouch which is a key defining feature of this sign.
This pouch may become distended secondary to effusion or gadolinium-based contrast. The double axillary pouch sign is seen as a small collection of fluid or contrast that extends into the substance of the inferior labrum.
The fluid accumulates between the torn anterior inferior glenoid labrum and the glenoid rim, giving the appearance of a second axillary pouch (Figure 1). Considered as a complementary piece of information, the double axillary pouch sign is often used to confirm a suspected labral tear [13-16].
4. Double Oreo Cookie Sign
Tears of the superior portion of labrum are known as superior labrum anteroposterior (SLAP) lesions which may begin posteriorly and extend anterior but stop before or at the mid-glenoid notch [13]. SLAP lesions are further categorized into Types I-IV, with different pathological features that guide management. A type III lesion is defined as a bucket handle tear of the superior portion of the labrum with the biceps attachment site remaining intact and is usually considered as a lesion that requires surgical intervention [14, 17, 18]. These patients classically present with this abnormality after a fall onto an outstretched arm [19].
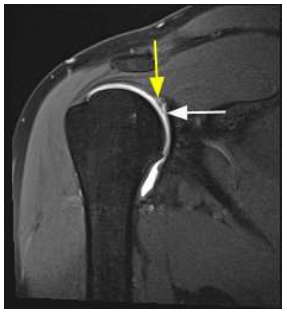
Figure 2: Double Oreo Cookie Sign. Coronal oblique T1 weighted fat saturated magnetic resonance imaging of a patient with a type 3 superior labral anteroposterior (SLAP) lesion, which is characterized by a bucket handle tear of the superior portion of the labrum with the biceps attachment site remaining intact. White arrows depicts the normal labrum anatomy and the yellow arrow depicts the bucket handle tear that is displaced into the joint. The intralabral tear parallels the chondrolabral junction (white arrow), which produces two parallel high intensity signals. An area of increased signal is present medially, while the more lateral high intensity signal represents contrast in a labral tear. The white lines between both areas of high intensity represent fluid within the labral tear and the recess, which gives the characteristic appearance of two Oreo cookies.
The double Oreo cookie sign refers to a type 3 superior labral anteroposterior (SLAP) lesion as the detached tear of the labrum is displaced into the joint with the peripheral portion of the labrum remaining attached to the glenoid labrum [17]. On a coronal oblique T1 weighted plane, the intralabral tear parallels a physiological sublabral recess, which produces two high intensity signals. An area of increased signal is present medially, while the more lateral high intensity signal represents contrast in a labral tear. The presence of two layers of white signal and three layers of intertwining dark signals likens this sign two the appearance of two Oreo cookies (Figure 2). The white lines between both areas of high intensity represent fluid within the labral tear and the recess [17, 19-21].
5. Geyser Sign
Acromioclavicular (AC) joint cysts are an uncommon sequela of shoulder pathology but usually arise in the setting of chronic degenerative changes to the rotator cuff and AC joint. Degenerative joint disease of the AC joint may be simply age-related changes of the intra-articular disc but may also occur secondary to posttraumatic and inflammatory arthropathies, impingement and infection [22]. Following massive damage to the rotator cuff, mechanical instability of the humeral head can lead to deterioration of the inferior acromioclavicular capsule, also known as cuff tear arthropathy and lead to an overproduction of synovial fluid. Eventually, fluid from the GH joint “erupts” superiorly into the degenerated AC joint and produces a cystic formation directly above the AC joint [23]. This phenomenon requires a direct communication between the GH joint and the AC joint thus a severe degree of degeneration or injury to the rotator cuff or AC capsule is required [24]. Patients will present with an insidious and slowly enlarging painless mass or pseudo-tumor that lies directly superior to the AC joint.
The characteristics of the Geyser sign allow it to be viewed on MRI as well as ultrasound and the conventional arthrogram. It was originally described in 1984 by Craig et al. [25] as leakage of dye from the glenohumeral joint into the subdeltoid bursa on an MR arthrogram in the presence of a long-standing full thickness rotator cuff tear with a secondary cystic swelling of the AC joint. On a sagittal oblique T2 section, the leakage of hyper-intense fluid outlines the AC joint and almost appears to be erupting as a “geyser” of fluid, as fluid moves towards the cyst along the acromion and clavicle (Figure 3) [24-26]. Initially described via an MR arthrogram, these lesions are now evaluated with non-contrast MRI as a more available and less invasive alternative. On coronal planes, AC joint cysts appear as decreased signal intensity on T1 and increased signal intensity on T2 images with communicating fluid from the GH joint into the AC joint cyst representing the Geyser sign [27].
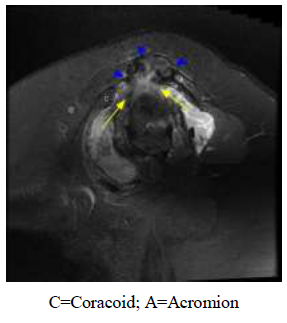
Figure 3: Geyser Sign. Sagittal oblique T2 weighted fat saturated magnetic resonance imaging of a patient with a full thickness rotator cuff tear with a joint effusion creating an acromioclavicular (AC) joint cyst. Fluid is being forced through the joint and accumulating within the cranial aspect of the AC joint. Yellow arrow depicts direction of fluid movement beneath the clavicle and acromion which outlines the AC joint and almost appears to be erupting as a “geyser” of fluid. The small blue arrow heads indicate heterogeneous fluid accumulation along the cranial aspect of the AC joint.
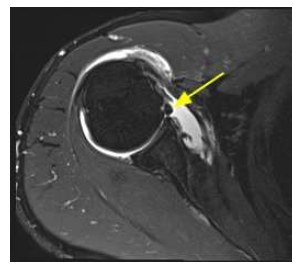
Figure 4: Glenoid Labrum Ovoid Mass Sign. Axial T2 weighted fat saturated magnetic resonance imaging of a patient with a prominent middle glenohumeral ligament (GHL) represented by a globular appearance in the anterior glenohumeral (GH) joint. The yellow arrow depicts a globular structure that lies anterior to the glenoid labrum.
6. Glenoid Labrum Ovoid Mass Sign (Glom)
Shoulder trauma is the leading cause of glenoid labrum pathology and is a key reason why MRI is used as an initial step in evaluation of an acute injury. The Glenoid Labrum ovoid mass (GLOM) sign is visualized on MR Arthrography in a T2 weighted sequence that represents a variety of pathologies such as a torn labral fragment that retracts superiorly, a dislocated biceps tendon or a prominent middle GH ligament. An oval-shaped, low intensity mass is seen on axial section and lies anterior to the glenoid within the GH joint (Figure 4). Due to its wide differential, it should be correlated with physical exam findings and other imaging findings to arrive at an accurate diagnosis [14].
7. J Sign
The inferior glenohumeral ligament (IGHL) is essential for stability and attaches medially to the glenoid labrum and laterally to the anatomical neck. It has an anterior band that is a part of an anterior labroligamentous complex that assists with anterior stability of the shoulder. A humeral avulsion of the glenohumeral ligament (HAGL) was originally used to describe a tear of the anterior band of the IGHL but a tear can occur at any portion along the ligament with involvement of the humeral attachment site [15]. This condition is also associated with anterior shoulder dislocation with resultant shoulder instability.

Figure 5: J Sign. Coronal oblique T1 weighted fat saturated magnetic resonance imaging of a patient with fluid extending inferior and laterally along axillary recess secondary to avulsion of the inferior glenohumeral ligament (GHL). Yellow arrow depicts fluid within the axillary pouch which takes the shape of the letter J. The axillary pouch is normally found between the anterior and posterior band of the inferior glenoid ligament which has a U shaped appearance when distended with gadolinium based contrast or fluid from an effusion. The avulsion of the inferior ligament from the neck of the humerus results in the detached end of the anterior or posterior band falling inferior which causes the fluid to transform from the normal U shaped appearance into a J shape.
Not to be confused with the “J Sign” that represents lateral patellar translocation anterolaterally and proximal to the trochlear groove during leg extension [28], the J sign in the shoulder refers to the presence of a humeral avulsion of the glenohumeral ligament (HAGL) [29]. There is an axillary pouch between the anterior and posterior band of the IGHL and fluid distension of the glenohumeral joint secondary to effusion or gadolinium-based contrast gives the inferior glenohumeral ligament a U shape in appearance on an oblique coronal T2 weighted MR image [14, 29]. Avulsion of the inferior ligament from the neck of the humerus results in the detached end of the anterior or posterior band to fall inferior. The retraction of the inferior glenohumeral recess causing a transformation from the normal U shaped appearance to a J shaped appearance (Figure 5) [29].
8. Subcoracoid Triangle Sign
Adhesive capsulitis, also known as frozen shoulder or periarthritis scapulae, is characterized by a progression of painful and restrictive in active and passive motion of the shoulder. A thickened, tight GH joint with adhesions and a fibrotic capsule is thought to be a key feature of pathology. Patients typically present with an insidious onset of referred deltoid pain of several months’ duration. Night pain, pain with repetitive overhead activity and a mechanical restraint of external rotation of the shoulder are key findings that are suggestive of adhesive capsulitis. Although adhesive capsulitis is often idiopathic, systemic conditions often contribute as well as a history of trauma, surgery or immobilization [24, 30].
On a sagittal T1 weighted MRI of a shoulder with normal anatomy, the subcoracoid fat triangle pad is a well-defined region of fat signal intensity that is bound by the coracoid process anterosuperiorly, GH joint capsule posteroinferiorly and coracohumeral ligament (CHL) superiorly. This area has fat intensity signaling and fills the intervening gap between the rotator interval joint capsule, CHL and the coracoid process. Complete obliteration of this fat triangle on MR imaging is considered diagnostic for adhesive capsulitis and is known as the subcoracoid triangle sign (Figure 6) [17]. The subcoracoid triangle sign is considered a highly specific (100%) but not sensitive sign for adhesive capsulitis, as previous studies have reported a 32% sensitivity [31]. Previous studies also have not been able to correlate this sign with clinical impairment [32-34]. However, Chellathurai et al. [35] found that it was more common in stages II and IV as it is related to fibrosis in late-stage adhesive capsulitis.
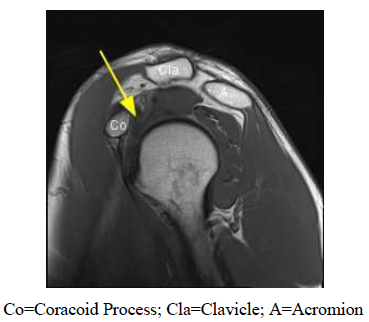
Figure 6: Subcoracoid Triangle Sign. Sagittal oblique T1 weighted magnetic resonance imaging of a patient with adhesive capsulitis. Yellow arrow depicts obliteration of triangular subcoracoid fat secondary to inflammation within the rotator cuff interval secondary to adhesive capsulitis. In a patient with normal anatomy, the subcoracoid fat triangle pad is a well-defined region of fat with high signal intensity that would be seen directly below the coracoid process (Co) as it usually fills the gap between the rotator cuff joint capsule and other structures. The absence of this area of fat is known as the subcoracoid triangle sign.
9. Tangent Sign
The supraspinatus tendon is one of the most commonly injured muscles of the rotator cuff. Infiltration of fatty tissue and atrophy can occur in the setting of chronic dysfunction and repair of a rotator cuff tear will not result in optimal function if the ability of the muscle to contract is irreversibly lost [36-38]. The cross-sectional area of the supraspinatus muscle can be measured on MR imaging which can be used to assess the degree of atrophy of the supraspinatus. The tangent sign has proven to be a reliable indicator of supraspinatus muscle fatty infiltration and atrophy and also plays a role in predicting clinical treatment outcomes. It is defined as the failure of the supraspinatus to cross a linear tangent that is drawn from the superior border of the coracoid process to the superior border of the scapula on a sagittal view of an MR image (Figure 7) [38, 39].
A supraspinatus with normal muscle composition crosses this tangent. As stated above, it is thought to be associated with chronic pathology and one study found a positive tangent sign indicated an average of 4.5 years since the initial onset of shoulder symptoms [19]. Studies have also shown that a positive tangent sign indicates poor prognosis of an irreparable rotator cuff tear [37, 40].
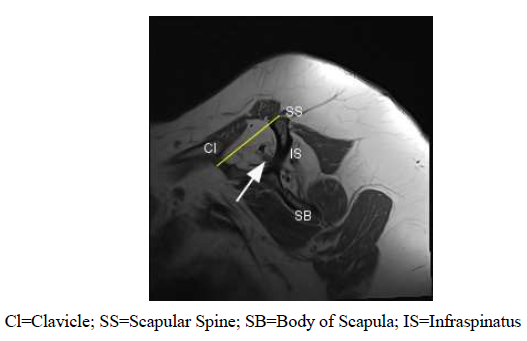
Figure 7: Tangent Sign. Sagittal oblique T1 weighted magnetic resonance imaging of a patient with severe atrophy of the supraspinatus. The white arrow depicts supraspinatus muscle fibers and the Tangent line is depicted by yellow line which is drawn between the superior border of the scapula and the scapular spine. In a patient with a normal anatomy, the muscle fibers of the supraspinatus intersect the tangent as large, dark accumulation of fibers. The severe atrophy of this patient’s muscle has caused the fibers to appear much lower than the proposed tangent line and the lack of intersection is a key characteristic of the tangent sign.
10. Conclusions
This paper serves as a mini review of a selection of unique clinical signs of shoulder pathology whose names are derived from their identification on MRI. Although the signs covered in this manuscript is not an all-inclusive list, these MRI radiographic signs are well published throughout the radiology literature and are well known to musculoskeletal radiologists. However, they are not as prevalent in literature associated with orthopaedics or sports medicine. Feedback amongst physicians and radiologist is important in furthering the diagnostic accuracy of MR imaging and thus it is essential to consistently develop methods in which patterns of disease of easily recognized.
Conflict of Interest
The authors wish to state that there was no personal or financial conflict of interest within the duration of the study.
Acknowledgements
We thank the Raymond and Beverly Sackler Center for Biomedical, Biological, Physical and Engineering Sciences and NIHDP1 AR068147 for their support.
References
- Lee P. The economic impact of musculoskeletal disorders. Qual Life Res 3 (1994): S85-S91.
- McBeth J, Jones K. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol 21 (2007): 403-425.
- Linaker CH, Walker-Bone K. Shoulder disorders and occupation. Best Pract. Res. Clin. Rheumatol 29 (2015): 405- 423.
- Pope DP, Silman AJ, Cherry NM, et al. Macfarlane GJ. Association of occupational physical demands and psychosocial working environment with disabling shoulder pain. Ann Rheum Dis 60 (2001): 852-858.
- Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med 30 (2002): 136-151.
- Lin DJ, Wong TT, Kazam JK. Shoulder Injuries in the Overhead-throwing athlete: Epidemiology, Mechanism of Injury, and Imaging Findings. Radiology 286 (2018): 370-387.
- Momenzadah OR, Gerami MH, Sefidbakht S, et al. Assessment of Correlation between MRI and Arthroscopic Pathologic Findings in the Shoulder Joint. Arch Bone Jt Surg 3 (2015): 286-290.
- Vahlensieck M. MRI of the Shoulder. Eur Radiol 10 (2000): 242-249.
- Baker SR, Noorelahi YM, Ghosh S, et al. History of Metaphoric signs in Radiology. Eur J Radiol 82 (2013): 1584-1587.
- Sofka C, Pavlov H. The history of clinical musculoskeletal radiology. Radiol Clin North Am 47 (2009): 349- 356.
- Carson Jr, WG. Arthroscopy of the shoulder: anatomy and technique. Orthop Rev 21 (1992): 143-153.
- O'Neill DB. Arthroscopic Bankart repair of anterior detachments of the glenoid labrum. A prospective study. J Bone Joint Surg Am 81 (1999): 1357-1366.
- Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy 18 (2002): 764-769.
- Rowan KR, Keogh C, Andrews G, et al. Essentials of Shoulder MR Arthrography: A Practical Guide for the General Radiologist. Clin Radiol 59 (2004): 327-334.
- Sharma P, Morrison WB, Cohen S. Imaging of the Shoulder with Arthroscopic Correlation. Clin Sports Med 32 (2013): 339-359.
- Zlatkin MB, Sanders TG. Magnetic Resonance Imaging of the Glenoid Labrum. Radiol Clin North Ame 51 (2013): 279-297.
- Modarresi S, Motamedi D, Jude CM. Superior Labral Anterioposterior Lesions of the Shoulder: Part 2, Mechanisms and Classifications. Am J Roentgenol 197 (2011): 604-611.
- Snyder SJ, Karzel RP, Pizzo WD, et al. SLAP lesions of the shoulder. Arthroscopy 6 (1990): 274-279.
- Mohana-Borges AVR, Chung CB, Resnick D. Superior Labral Anteroposterior Tear: Classification and Diagnosis on MRI and MR Arthrography. Am J Roentgenol 181 (2003): 1449-1462.
- Dong Q, Jacobson JA, Brandon CJ, et al. Important Signs in Musculoskeletal MRI. Journal of Advances in Medicine & Medical Research 6 (2015): 240-253.
- Park YH, Lee JY, Moon SH, et al. MR Arhthrography of the Labral Capsular Ligamentous Complex in the Shoulder Imaging Variations and Pitfalls. Am J Roentgenol 175 (2000): 667-672.
- Mall NA, Foley E, Chalmers PN, et al. Degenerative Joint Disease of the Acromioclavicular Joint: A Review. Am J Sports Med 41 (2013): 2684-2692.
- Hiller AD, Miller JD, Zeller JL. Acromioclavicular Joint cyst formation. Clin Anat 23 (2010): 145-152.
- Palmer W, Bancroft L, Bonar F, et al. Glossary of terms for musculoskeletal radiology. Skeletal Radiol 49 (2020): 1- 33.
- Craig EV. The geyser sign and torn rotator cuff: clinical significance and pathomechanics. Clin Orthop 191 (1984): 213-215.
- Negi CRS, Gogoi CB, Randhawa MAS. MR Geyser Sign in chronic rotator cuff tears. Med J Armed Forces India 74 (2018): 304-306.
- Nowak DD, Cowey AS, Grant RT, et al. Massive Acromioclavicular joint cyst. J Shoulder Elbow Surg 18 (2009): 12-14.
- Beckert MW, Albright JC, Zavala J, et al. Clinical Accuracy of J-Sign Measurement Compared to Magnetic Resonance Imaging. Iowa Orthop J 36 (2016): 94-97.
- Carlson CL. The J Sign. Radiology 3 (2004): 725-726.
- Neviaser AS, Neviaser RJ. Adhesive Capsulitis of the Shoulder. J Am Acad Orthop Surg 19 (2011): 536-542.
- Fields BK, Skalski MR, Patel DB, et al. Adhesive Capsulitis: Review of imaging findings, pathophysiology, clinical presentation and treatment options. Skeletal radiol 48 (2019): 1171-1184.
- Park YH, Lee JY, Moon SH, et al. MR Arhthrography of the Labral Capsular Ligamentous Complex in the Shoulder Imaging Variations and Pitfalls. Am J Roentgenol 175 (2000): 667-672.
- Lee SY, Park J, Song SW. Correlation of MR arthrographic findings and range of shoulder motions in patients with frozen shoulder. AJR Am J Roentgenol 198 (2012): 173-179.
- Park S, Lee DH, Yoon SH, et al. Evaluation of adhesive capsulitis of the shoulder with fat-suppressed T2- weighted MRI: association between clinical features and MRI findings. AJR Am J Roentgenol 207 (2016): 135-141.
- Chellathurai A, Subbiah K, et al. Adhesive Capsulitis: MRI Correlation with clinical stages and proposal of MRI staging. Indian J Radiol Imaging 29 (2019): 19-24.
- Lapner PL, Jiang L, Zhang T, et al. Rotator cuff fatty infiltration and atrophy are associated with functional outcomes in anatomic shoulder arthroplasty. Clin Orthop Relat Res 473 (2015): 674-682.
- Melis B, DeFranco MJ, Walch G. Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res 468 (2010): 1498-1505.
- Morag Y, Jacobson JA, Miller B, et al. MR Imaging of Rotator Cuff Injury: What the Clinician Needs to Know. Radiographics 26 (2006): 1046-1065.
- Kissenberth MJ, Rulewicz GJ, Hamilton SC, et al. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elbow Surg 23 (2014): 1023-1027.
- Williams MD, Ladermann A, Melis B, et al. Fatty infiltration of the supraspinatus: A reliability study. J Shoulder Elbow Surg 18 (2009): 581- 587.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 