Seroprevalence of Hepatitis E Virus (HEV) Antibodies in Human Populations of Sokodé, Togo
Komi Victor-Mari Setondji1†*, Kuan Abdoulaye Traoré1,2†, Jean-Bienvenue Ouoba1, Essodolom Taale3, Bruno Lalidia Ouoba1, Bissah Kokou Nyakou4, Pierre Roques5,6,7,8, Simplice Damintoti Karou3 and Nicolas Barro1
1Department of Biochemistry and Microbiology, Life and Earth Sciences Training Unit, Joseph KI-ZERBO University, Ouagadougou BP 7021, Burkina Faso
2Department of Biology, Life and Earth Sciences Training Unit, Norbert ZONGO University, Koudougou BP 376, Burkina Faso
3Higher School of Biological and Food Technology, Faculty of Health Sciences, University of Lomé, Lomé BP 1515, Togo
4Sokodé Regional Blood Transfusion Center, Laboratory Division of the Ministry of Health and Public Hygiene, Sokodé BP 39, Togo
5IDMIT Département/IBFJ|CEA, 92265 Fontenay-aux-Roses, France; pierre.roques@cea.fr
6Immunology of Viral Infections and Autoimmune Diseases (IMVA-HB), U1184, INSERM, 92265 Fontenay-aux-Roses, France
7UMR1184, IMVA-HB, Université Paris-Saclay, 91400 Orsay, France
8Virology Unit, Institut Pasteur de Guinée, Conakry BP 4416, Guinea
† These authors contribute equally to this work.
*Corresponding author: Komi Victor-Mari Setondji, Department of Biochemistry and Microbiology, Life and Earth Sciences Training Unit, Joseph KI-ZERBO University, Ouagadougou BP 7021, Burkina Faso.
Received: 27 December 2022; Accepted: 06 January 2023; Published: 13 January 2023
Article Information
Citation: Komi Victor-Mari Setondji, Kuan Abdoulaye Traoré, Jean-Bienvenue Ouoba, Essodolom Taale, Bruno Lalidia Ouoba, Bissah Kokou Nyakou, Pierre Roques, Simplice Damintoti Karou and Nicolas Barro. Seroprevalence of Hepatitis E Virus (HEV) Antibodies in Human Populations of Sokodé, Togo. Archives of Clinical and Biomedical Research 7 (2023): 19-27.
View / Download Pdf Share at FacebookAbstract
Background: Hepatitis E virus (HEV) antibodies prevalence is reported globally worldwide. However, there is still some countries where data are not well reported or even studied as in Togo. The aim of this study was to evaluate the seroprevalence of HEV among human populations and analyze demographic variables related to the infection in the city of Sokodé, in central area of Togo.
Results: A total of 289 individuals including 195 blood donors (24 women and 171 men), and 94 pregnant women were recruited from May to October 2020 and socio-economic status were assessed. All obtained sera were tested for the presence of anti-HEV antibodies with the immunochromatography test (MP Diagnostics ASSURE IgM Rapid test) and the MP Diagnostics HEVIgM and HEV-IgG ELISA. The association between anti-HEV status and potential risk factors was assessed. Total HEV antibodies were in 5.6% (95% CI: 3.8 - 7.3%) of all samples. HEV IgM antibodies were detected in 11.7% (95% CI: 9.8-13.5%) of the samples, of which 29 (14.8%) were from the blood donors group and 5 (5.3%) from pregnant women group. Gender, water storage container, type of latrine used and washing hands after toilet were associated to anti-HEV IgM seropositivity in population (p ≤ 0.05).
Conclusion: These findings from asymptomatic population suggest a probable HEV circulation at significant levels. These data are the first step to understand the epidemiology of the HEV infection in Togo that deserved to be extended both in timing and Togo’s region.
Keywords
<p>Blood donors; hepatitis E virus (HEV); Pregnant women; Seroprevalence; Togo</p>
Article Details
List of Abbreviations:
HEV- Hepatitis E virus; ORF- Open Reading Frame
1. Introduction
Hepatitis E virus (HEV) is a non-enveloped, non-enveloped, single-stranded and polarity-positive RNA virus [1]. It ranges in size from 6.4 to 7.2 Kb with three open reading frames (1-3) ORFs [2]. HEV belongs to the family Hepeviridae which is subdivided into two genera: Orthohepevirus and Piscihepevirus [3]. The genus Orthohepevirus contains four species from A to D. Members of the genus Orthohepevirus A includes 8 genotypes: the HEV-1 and HEV-2, restricted to humans, are responsible for large hepatitis E outbreaks described in developing regions like Africa and Asia. HEV-3 and HEV-4, detected in humans and other animals, are the main cause of sporadic infection among humans in developed countries. HEV-5 and HEV-6 are found in wild boars. HEV-7 has identified recently in an immunocompromised transplant patient and in dromedary camels. HEV-8 has been recently described in the Bactrian camels [4]. Orthohepevirus B is divided into four subtypes (I–IV) of avian viruses identified mainly in domestic chicken. Orthohepevirus C contains two genotypes detected in rats (HEV-C1) and carnivores (HEVC2) [5, 6]. Different bat species represent the animal reservoirs for Orthohepevirus D strains [2, 3, 7]. Fecal-oral transmission is the main route of transmission of HEV [8]. Parenteral, [9], transfusional, or iatrogenic transmission of HEV [10, 11] by blood transfusion of blood products has been identified as a new potential mode of contamination, which could be a risk to transfusion safety. Recent studies have reported zoonotic HEV infections due to consumption of raw or undercooked animal meat or direct contact with infected animals [4, 12]. HEV is endemic in much of the world most notably in tropical and subtropical regions [13]. According to the [14] report, from poor hygiene conditions and sanitation problems, our populations are daily exposed to perilous fecal viruses such as HEV which could cause epidemics. Acute hepatitis E, which is most often benign, can result in a mortality of 0.2-5% during epidemics. Fulminant forms affect pregnant women more during the third trimester of pregnancy with a mortality rate of about 20% [15]. These data raise many concerns about the health of populations. Serological evidence of HEV infection was documented worldwide. In developed countries, a great geographical heterogeneity of anti-HEV carriers with low seroprevalence in the United States, Scotland and North America, and high seroprevalence for in the southwest of France, has been reported [16, 17]. Seroprevalence rates are highly variable not only from country to country, but also in the same geographical area and study population [18]. For Immuniglobulin M, it was 5.7% in Saudi Arabia [19] and 14.22% in China [20] among blood donors and pregnant women. In Africa, total antibody seroprevalence was 43.4% in Ethiopia [21], 17.6% in Benin [22] and 78.4% in Cameroon [23]. Specific anti-HEV IgM was 3.19% in Burkina Faso [24], 4.3% in Chad [25] and 1.44% in Benin [22]. In Togo, neither prevalence nor the impact of HEV infection in the population was assessed before. However, because of the socioeconomic situation in a cross-road, the hygiene standards and the nutritional habits marked by the consumption of street-vended products, togolese inhabitants are undoubtedly exposed to this virus (HEV) [26]. The objective of this study was to determine the seroprevalence of HEV in the population of Sokodé, the second largest city in Togo, and to identify risk factors associated with the infection scares that would contribute to its persistence in the population.
2. Material and Methods
2.1 Study Design and Study Site
From May to October 2020, a cross-sectional study was conducted and included 289 asymptomatic persons (171 males and 118 females). These samples represent two populations including 195 blood donors and 94 pregnant women in their last trimester of pregnancy. The study was approved by the Bioethics Committee for Health Research under the n°: 040/2019/CBRS, and moreover the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in approval by the Ministry of Health and Public Hygiene (Togo) under the n°: 027/2020/MSHP/CAB/SG/DGAS/DPML/CBRS. Administrative authorization was also obtained from the Polyclinic and the Regional Blood Transfusion Center of Sokodé.
2.2 Data Collection and Sampling
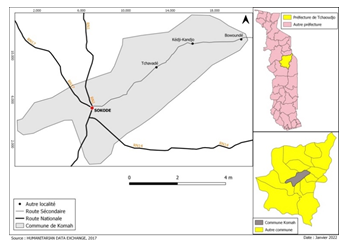
After their informed consent obtained, all participants included in the research were surveyed and their sera were collected at two sites in Sokodé (figure 1): The Polyclinic and the Regional Blood Transfusion Center. Sokodé is a city with around 120,000 inhabitants in the middle of Togo equally distant from the tropical weather from the sea side (320 kM) and the dry Sahelian climate. At 340 m high, the Sokodé weather is thus characterized by a single rain season from April to October with a peak between July to September.
Demographic and baseline characteristics included were age, sex, area of residence, profession, religion. We also collected data on the presence of domestic animals in the home, livestock practice, source of water, treatment of water before consumption, method of cooking meat before consumption, consumption of pork, water storage container, type of latrine used, washing hands after toilet, knowledge of hepatitis, having ever been screened for hepatitis or vaccinated against hepatitis. Five milliliters of blood were collected in EDTA tube from each participant. Blood samples were processed in accordance with the requirements of the Blood Bank Management Committee of the Regional Blood Transfusion Center (RBTC). The sample was centrifuged at 3000g for 10 min at 25°C. The sera were collected in cryotubes and stored at -20 ± 5°C until serological analysis.
2.3 Serological Analyses
A total of 289 serum of samples collected from 195 blood donors and 94 pregnant women were tested for the presence of anti-HEV antibodies (IgM and total HEV antibodies) with enzyme-linked immunosorbent assays (ELISA) and immunochromatographic assay: 178 samples were tested with total (IgG, IgM, and IgA) HEV antibody ELISA 4.0 kit, 89 samples with HEV immunoglobulin M (IgM) ELISA 3.0 kit and 200 samples with ASSURE HEV IgM/ Rapid Test (MP Biomedicals Asia Pacific Pte Ltd, Singapore; formerly Genelabs Diagnostics Pte) (Table 1).
|
Total HEV ab ELISA 4.0 |
Total HEV ab ELISA 4.0 +TDR IgM |
Total HEV ab ELISA 4.0+ HEV IgM ELISA 3.0 |
HEV IgM ELISA 3.0 |
ASSURE HEV TDR IgM |
|
|
Blood donor |
178 |
106 |
72 |
89 |
106 |
|
Pregnant women |
- |
- |
- |
- |
94 |
|
Total |
178 |
106 |
72 |
89 |
200 |
Table 1: The different tests performed by population groups.
The tests were carried out according to the manufacturer’s instructions and assay validity was evaluated according to the manufacturer’s specifications. MP Diagnostic HEV ELISA 4.0 uses a proprietary recombinant antigen, which is highly conserved between different HEV strains, recognized by anti-HEV specific antibodies including IgG, IgM and IgA classes. MPD HEV IgM ELISA 3.0 is an indirect immunoassay that utilizes a highly conserved conformational epitope derived from open reading frame 2 (ORF 2) of the hepatitis E virus limited to IgM detection with a reported sensitivity of 98% and specificity of 96.7%. MPD HEV ELISA 4.0 and ELISA 3.0 results were based on signal-to-cutoff (CO) ratio. Specimens with absorbance values less than the CO value are considered non-reactive, and with absorbance values greater than or equal to the CO value are considered initially reactive. The Assure HEV IgM rapid test is a Rapid Diagnostic Test (RDT) based on solid phase immunochromatographic assay for qualitative and differential detection of IgM antibodies to Hepatitis E virus in human serum, plasma or whole blood with sensitivity 100% and specificity 95.41% according to the manufacturer's manual.
2.4 Statistical Analysis
Data analysis was performed with SPSS version 21 software. Descriptive statistical analysis was used to calculate the mean, median, percentages of sociodemographic variables, percentage of seropositivity to anti-IgM and anti-IgG antibodies at the 95% confidence interval (95%CI). Statistical analysis was performed using the Chi-square test (x2). The test was considered significant at a p value < 0.05.
3. Results
3.1 Socio-Demographic Characteristics of Study Participants
A total of 289 individuals participated in this study, of whom 118 (40.8%) were women and 171 (59.2%) were men. The age range was 17 to 51 years, with a mean age of 26.16 (± 6.53SD) years and a median of 24 years. Among 94 pregnant women, the age range was 17 to 40 years, with a mean age of 27.04(± 6.7SD). In donors, the age range was 18 to 51 years, with a mean age of 25.75 (± 5.63SD), and 87.7% (171/195) were male. In the study population 94.1% lived in urban areas, 71.7% treated water with chlorine or boiled it before consumption, 98.6% cooked meat well before consumption, and 70.5% did not consume pork. Concerning the type of latrine used, 65.7% had individual latrines compared to 34.3% who used community latrines. Also, 99% observed handwashing after washing, and 94.8% did so with a soap. Regarding the age, 47.9% (45/94) of pregnant women and 67.1% (131/195) of donors were under 25 years. The data are presented in table 2.
|
Population: |
Pregnant women |
Blood donors |
|
N=94(%) |
N=195(%) |
|
|
Age |
||
|
≤25 |
45(47.9) |
131(67.1) |
|
26-35 |
41(43.6) |
54(27.6) |
|
36≥ |
8(8.5) |
15(5.3) |
|
Gender |
||
|
Female: |
94(100) |
24(12.3) |
|
Male: |
171(87.7) |
|
|
Area of residence |
||
|
Urban: |
87(92.5) |
185(94.5) |
|
Rural: |
7(7.4) |
10(5.5) |
|
Profession |
||
|
Butcher: |
1(1.1) |
0(0) |
|
Breeder: |
0(0) |
2(1) |
|
Other: |
93(98.9) |
193(99) |
|
Religion |
||
|
Christian: |
29(30.9) |
93(47.6) |
|
Muslim: |
64(68.1) |
98(50.2) |
|
Other: |
1(1.1) |
4(2.2) |
|
Presence of animals in the house: |
||
|
Yes: |
40(42.6) |
90(46.1) |
|
No: |
54(57.4) |
105(53.9) |
|
Breeding practice |
||
|
No: |
47(50) |
135(69.2) |
|
Yes: |
47(50) |
60(30.8) |
|
Source of water consumed |
||
|
Well: |
35(37.2) |
83(42.5) |
|
Tap: |
56(59.6) |
109(55.8) |
|
Mineral: |
3(3.2) |
3(1.7) |
|
Water treatment before consumption (chlorine or slurry) |
||
|
No: |
||
|
Yes: |
46(48.9) |
36(18.4) |
|
48(51.1) |
159(81.6) |
|
|
Cooking method of the meat before consumption |
||
|
Cooked to medium rare: |
91(96.8) |
194(99.4) |
|
No medium rare: |
3(3.2) |
1(0.6) |
|
Consume pork meat |
||
|
No: |
76(80.9) |
128(65.6) |
|
Yes: |
18(19.1) |
67(34.4) |
|
Water storage container |
||
|
Seal: |
68(72.3) |
129(66.1) |
|
Can: |
15(16.0) |
46(23.5) |
|
Container: |
11(11.7) |
20(12.4) |
|
Type of latrine used |
||
|
Individual: |
65(69.1) |
125(64.1) |
|
Common: |
29(30.9) |
70(35.9) |
|
Washing hands after toilet |
||
|
No: |
0(0) |
3(1.5) |
|
Yes: |
94(100) |
192(98.5) |
|
Hands washing with detergent |
||
|
No: |
1(1.1) |
14(7.1) |
|
Yes: |
93(98.9) |
181(92.9) |
|
Have knowledge of hepatitis |
||
|
No: |
42(44.7) |
90(46.1) |
|
Yes: |
52(55.3) |
105(53.9) |
|
Already screened for hepatitis |
||
|
No: |
57(60.6) |
28(14.3) |
|
Yes: |
37(39.4) |
167(85.7) |
|
Already vaccinated against hepatitis |
||
|
No: |
86(91.5) |
175(89.7) |
|
Yes: |
8(8.5) |
20(10.3) |
Table 2: Socio-demographic characteristics of study participants.
3.2 Seropositivity of HEV Antibodies
Overall, 34 samples (11.7%; 95% confidence interval: 9.8%-13.5%) were positive for IgM antibodies, HEV markers of acute infection. Amongst these, 14.8% (95% CI: 12.2 - 17.3%) were blood donors and 5.6% (95% CI: 3.8 - 7.3%) of pregnant women. Of these 178 blood donors tested to total HEV antibodies, 5.6% (95% CI: 3.8 - 7.3%) were positive (table 3). In total, 7 of the 118 women samples (5.93%) (95% CI: 1.67-10.19) were positive for anti-HEV IgM, including 2/24 samples (8.33%) (95% CI: 0-19.38%) from blood donor women and 5/89 samples (5.32%) (95% CI: 0.78-9.86) from pregnant participants with no significant difference according to sex female (p = 0.31) (Supplemental table S1).
|
ELISA IgM |
TDR IgM |
|||
|
Blood donor’s n (%) |
Blood donor’s n (%) |
Pregnant women n (%) |
Total n (%) |
|
|
Total antibodies positives |
7(7.86) |
3(2.83) |
- |
10 (5.62) |
|
Anti-IgM positives |
12(13.48) |
17(16.04) |
5(5.32) |
34 (11.76) |
|
Total antibodies positive and IgM negative |
6(6.74) |
2(1.89) |
- |
8 (4.49) |
|
IgM positive and Total antibodies positive |
1(1.12) |
1(0.94) |
- |
2 (1.12) |
|
IgM positive and Total antibodies negative |
11 (12.36) |
16 (15.09) |
- |
27 (15.17) |
Table 3: Results of HEV total and M immunoglobulin detection.
|
Anti-IgM HEV |
|||
|
Women |
Pos: n (%) |
Neg: n (%) |
P value |
|
Blood donor |
2 (8.33) |
22 (91.7) |
0.31 |
|
Pregnant |
5 (5.32) |
89 (94.7) |
|
|
Total |
7 (5.93) |
111 (94.1) |
|
Supplemental Table S1: Seroprevalence of HEV in women.
3.3 Risk Factors associated with HEV Infection
Regarding the risk factor analyses, gender, water storage container, type of latrine used and washing hands after toilet were significantly associated to anti-HEV IgM seropositivity in population (p ≤ 0.05). Table 4 below presents the risk factors associated with HEV infection.
|
Anti-IgM HEV |
|||||||||
|
Population |
Blood donors |
Pregnant women |
General population |
||||||
|
Neg: n (%) |
Pos: n (%) |
Pvalue |
Neg: n (%) |
Pos: n (%) |
P value |
Neg: n (%) |
Pos: n (%) |
P value |
|
|
Age |
|||||||||
|
≤25 |
104(82.5) |
22(17.5) |
0.36 |
42(93.3) |
3(6.7) |
0.44 |
146(85.3) |
25(14.7) |
0.19 |
|
26-35 |
48(88.9) |
6(11.1) |
40(97.6) |
1(2.4) |
88(92.6) |
7(7.4) |
|||
|
36≥ |
14(93.3) |
1(6.7) |
7(87.5) |
1(12.5) |
21(91.3) |
2(8.7) |
|||
|
Gender |
|||||||||
|
Female: |
22(91.7) |
2(8.3) |
0.34 |
89(94.7) |
5(5.3) |
>0.5 $ |
111(94) |
7(5.9) |
0.011* |
|
Male: |
144(84.2) |
27(15.8) |
- |
- |
144(84.2) |
27(15.8) |
|||
|
Area of residence |
|||||||||
|
Urban: |
156(84.3) |
29(15.7) |
0.17 |
82(94.3) |
5(5.7) |
0.51 |
238(87.5) |
34(12.5) |
0.121 |
|
Rural: |
10(100) |
0(0) |
7(100) |
0(0) |
17(100) |
0(0) |
|||
|
Profession |
|||||||||
|
Butcher: |
0(0) |
0(0) |
0.55 |
1(100) |
0(0) |
0.81 |
1(100) |
0(0) |
0.817 |
|
Breeder: |
2(100) |
0(0) |
0(0) |
0(0) |
2(100) |
0(0) |
|||
|
Other: |
164(85.0) |
29(15.0) |
88(94.6) |
5(5.4) |
252(88.1) |
34(11.9) |
|||
|
Religion |
|||||||||
|
Christian: |
77(82.8) |
16(17.2) |
0.52 |
29(100) |
0(0) |
0.29 |
106(86.8) |
16(13.2) |
0.623 |
|
Muslim: |
85(86.7) |
13(13.3) |
59(92.2) |
5(7.8) |
144(88.8) |
18(11.2) |
|||
|
Other: |
4(100) |
0(0) |
1(100) |
0(0) |
5(100) |
0(0) |
|||
|
Presence of animals in the house: |
|||||||||
|
Yes: |
72(80.0) |
18(20) |
0.06 |
51(94.4) |
3(5.6) |
0.91 |
123(85.4) |
21(14.5) |
0.138 |
|
No: |
94(89.5) |
11(10.5) |
38(95.0) |
2(5.0) |
132(91) |
13(9) |
|||
|
Breeding practice |
|||||||||
|
No: |
118(87.4) |
17(12.6) |
0.18 |
44(93.6) |
3(6.4) |
0.65 |
162(89) |
20(11) |
0.593 |
|
Yes: |
48(80.0) |
12(20.0) |
45(89.8) |
2(4.3) |
93(86.9) |
14(13.1) |
|||
|
Source of water consumed |
|||||||||
|
Well: |
67(80.7) |
16(19.3) |
0.28 |
34(97.1) |
1(2.9) |
0.62 |
101(85.5) |
17(14.5) |
0.38 |
|
Tap: |
96(88.1) |
13(11.9) |
52(92.9) |
4(7.1) |
148(89.6) |
17(10.4) |
|||
|
Mineral: |
3(100) |
0(0) |
3(100) |
0(0) |
6(100) |
0(0) |
|||
|
Water treatment before consumption (chlorine or slurry) |
|||||||||
|
No: |
28(77.8) |
8(22.2) |
0.17 |
41(89.1) |
5(10.9) |
0.02* |
69(84.1) |
13(15.9) |
0.174 |
|
Yes: |
138(86.8) |
21(13.2) |
48(100) |
0(4.8) |
186(89.8) |
21(10.2) |
|||
|
Cooking method of the meat before consumption |
|||||||||
|
Cooked to medium rare: |
165(85.1) |
29(14.9) |
0.67 |
87(95.6) |
4(4.4) |
0.03* |
252(88.4) |
33(11.6) |
0.408 |
|
No medium rare: |
1(75) |
0(25) |
2(66.7) |
1(33.3) |
3(75) |
1(25) |
|||
|
Consume pork meat |
|||||||||
|
No: |
107(83.6) |
21(16.4) |
0.4 |
71(93.4) |
5(6.6) |
0.26 |
175(87.5) |
26(12.5) |
0.423 |
|
Yes: |
59(88.1) |
8(11.1) |
18(100) |
0(0) |
77(90.7) |
8(9.3) |
|||
|
Water storage container |
|||||||||
|
Seal: |
110(85.3) |
19(14.7) |
0.07 |
65(95.6) |
3(4.4) |
0.27 |
175(88.8) |
22(11.2) |
0.019* |
|
Can: |
36(78.3) |
10(21.7) |
13(86.7) |
2(13.3) |
49(80.3) |
12(19.7) |
|||
|
Container: |
20(100) |
0(0) |
11(100) |
0(0) |
33(100) |
0(0) |
|||
|
Type of latrine used |
|||||||||
|
Individual: |
111(88.8) |
14(11.2) |
0.05* |
63(96.9) |
2(3.1) |
0.15 |
174(91.5) |
16(8.5) |
0.015* |
|
Common: |
55(78.6) |
15(21.4) |
26(89.7) |
3(10.3) |
81(81.8) |
18(18.2) |
|||
|
Washing hands after toilet |
|||||||||
|
No: |
1(33.3) |
2(66.7) |
0.01* |
0(0.0) |
0(0.0) |
- |
1(33.3) |
2(66.7) |
0.003* |
|
Yes: |
165(85.9) |
27(14.1) |
89(94.7) |
5(5.3) |
254(88.8) |
32(11.2) |
|||
|
Hands washing with detergent |
|||||||||
|
No: |
13(92.9) |
1(7.1) |
0.4 |
1(100) |
0(0) |
0.81 |
14(93.3) |
1(6.7) |
0.529 |
|
Yes: |
153(84.5) |
28(15.5) |
88(94.6) |
5(5.4) |
241(87.9) |
33(12.1) |
|||
|
Have knowledge of hepatitis |
|||||||||
|
No: |
77(85.6) |
13(14.4) |
0.88 |
39(92.9) |
3(7.1) |
0.48 |
116(87.8) |
16(12.2) |
0.863 |
|
Yes: |
89(84.8) |
16(15.2) |
50(96.2) |
2(3.8) |
139(88.5) |
18(11.6) |
|||
|
Already screened for hepatitis |
|||||||||
|
No: |
24(85.7) |
4(14.3) |
0.92 |
53(93.0) |
4(7.0) |
0.36 |
77(90.6) |
8(9.4) |
0.423 |
|
Yes: |
142(85) |
25(15.0) |
36(97.3) |
1(2.7) |
178(87.2) |
26(12.8) |
|||
|
Already vaccinated against hepatitis |
|||||||||
|
No: |
148(84.6) |
27(15.4) |
0.52 |
82(95.3) |
4(4.7) |
0.34 |
230(88.1) |
31(11.9) |
0.856 |
|
Yes: |
18(90.0) |
2(10.0) |
7(87.5) |
1(12.5) |
25(89.2) |
3(10.8) |
|||
*Significant (p<0.05).
$ here we compare positive females ratio between blood donor female and pregnant female.
Table 4: HEV immunoglobulins associated with risk factors. In bold significant values (p<0.05) or data that will be commented.
4. Discussion
This study is the first to determine the seroprevalence and risk factors of HEV infection in different populations including blood donors and pregnant women in Sokodé, Togo. Blood donors and pregnant women are fairly representative of the general healthy population. Therefore, studies focusing on these two groups together have a public health importance. In this study, the overall IgM anti-HEV (11.7%) were similar to those described in Cameroon (12.2%) [27]. IgM seropositivity were 5.32% and 14.87% in pregnant women and blood donors respectively. This high seropositivity to IgM shows that there was possibly an outbreak of HEV infection although no reference test is available. Moreover, a high seroprevalence was observed in males compared to females, which may be linked to cultural practices among other factors that probably expose them to contaminated food or water more frequently than women [28]. The men are commonly involved with other environmentally related works locally considered as men’s job, spending much time with the animals, and handling animals at home, irrigation farming using contaminated river water, working in animal farms, and disposal of human and animal waste [29]. In Togo, street food consumers are also mainly men [30], who are more likely to be exposed to HEV-infected foods. Anti-HEV IgM positivity is no significantly in pregnant females (5.27%) compared to blood donor females (P = 0.31). An extensive sample of female blood donors is needed to enable in-depth risk factor analysis. Total HEV antibody seropositivity in blood donors was less than 6%. This study is not the first study to show the high seropositivity to IgM (14.87%) compared with total HEV antibodies (5.62%). A study in Cameroon had already shown high seropositivity to IgM (22.0%) compared with IgG (5.8%) [31]. The high seropositivity to IgM shows that there was possibly an outbreak of HEV infection whose origin was unknown. However, this prevalence could be associated to the poor sanitation system and insufficient distribution of potable water in various arteries of the city. Total HEV antibody seroprevalence in this study was lower than those observed in Nigeria (21%) and Niger (38.4%) [32, 33]. The differences in seroprevalences may be due to the different assays used, differences in demographic characteristics between studies, or various factors fueling HEV transmission in the different geographical areas. Although it is not clear if transmission pathways vary by age group, we observed that type of latrine used and washing hands after toilet after defecation were associated were independently associated with risk of a recent exposure to HEV (P<0.05). This is basically consistent with what had been found in other studies. In line with others studies, we found no significant evidence of an association between HEV infection and dietary risk factors in either women or blood donors (p≥ 0.05). However, this does not completely disregard them as putative risk factors, but may require thorough investigations in Sokodé. [31], had also observed that no alimentary risk factors were significantly associated with HEV infection in all three populations (elderly people, pregnant women, and HIV-infected patients). But unlike these studies, [34], reported a significant correlation between rural area of residence on the one hand and use of fecally contaminated water on the other [35] as well as consumption of pork products [36].
5. Limitations of the Study
This study has some limitations. It could not confirm the presence of HEV RNA in the seropositive population samples in order to examine active HEV prevalence, especially in those asymptomatically infected individuals. Another limitation is no pregnant women samples were tested in this study due to the limited number of total HEV antibody assays. It is not known if any recipient has developed post-transfusion hepatitis/jaundice because recipients (if any) were not evaluated or examined for HEV antibodies and/or RNA. We assume that the blood products were used because HEV screening is not mandatory in Sokodé, Togo unlike HCV, HIV and HBV.
6. Conclusion
This study showed the presence of anti-HEV antibodies in human populations in Sokodé, suggesting that they have been in contact with HEV. The high seroprevalence of IgM anti-HEV obtained indicates there is a risk of major outbreaks of this infection in Sokodé. Further studies are needed to identify the different strains of HEV in circulation and the different potential reservoirs of the virus in order to understand the epidemiology and persistence of the infection in the population while seeking to control its transmission.
Consent to Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Funding
This study was financed by the Directorate of Scholarships and Training of the Togolese State.
Author Contributions
KVMS, KAT, JBO, ET, PR, SDK, and NB participated in the study design. KVMV, BKN, and KAT performed serological analyses, KVM, KAT, BLO, and PR performed the statistical analysis, and all authors participated in drafting and revising the manuscript. All authors read and approved the final version.
Acknowledgements
Not applicable.
Ethical Approval
The study was approved by the Bioethics Committee for Health Research of the Ministry of Health and Public Hygiene of Togo under No.: 040/2019/CBRS, and furthermore the study protocol complies with the ethical guidelines of the 1975 Declaration of Helsinki, as evidenced by the approval of the Ministry of Health and Public Hygiene (Togo) under No.: 027/2020/MSHP/CAB/SG/DGAS/DPML/CBRS. The administrative authorization was also obtained from the Polyclinic and the Regional Blood Transfusion Center of Sokodé. Informed consent was obtained from all study participants after they were informed of the project.
Availability of Data and Materials
Not applicable.
References
- Hepatitis E (2016).
- Purdy MA, Harrison TJ, Jameel S, et al. Journal of General Virology 98 (2017): 2645-2646.
- Smith DB, Simmonds P, Jameel S, et al. Consensus proposals for classification of the family Hepeviridae. J Gen Virol 96 (2015): 1191-1192.
- Spahr C, Knauf-Witzens T, Vahlenkamp T, et al. Review article Hepatitis E virus and related viruses in wild, domestic and zoo animals. Zoonoses Public Health 65 (2017): 11-29.
- Thiry D, Mauroy A, Pavio N, et al. Hepatitis E Virus and Related Viruses in Animals. Transboundary and Emerging Diseases (2015).
- Modiyinji AF, Rivero-Juarez A, Lopez-Lopez P, et al. First molecular characterization of the hepatitis E virus in humans in Cameroon: Confirmation of the HEV outbreak in Touboro, North-Cameroon. Journal of Medical Vorology 93 (2021): 4018-4022.
- Woo PCY, Lau SKP, Teng JLL, et al. New hepatitis E virus genotype in Bactrian Camels, Xinjiang, China, 2013. Emerging Infectious Diseases 22 (2016): 2219-2221.
- Wu J, Si F, Jiang C, et al. Molecular detection of hepatitis E virus in sheep from southern Xinjiang, China. Virus Genes 50 (2015): 410-417.
- Mansuy JM, Saune K, Rech H. Seroprevalence in blood donors reveals widespread, multi-source exposure to hepatitis E virus, southern France, October 2011. Euro Surveillance 20 (2015): 27-34.
- Hewitt PE, Ijaz S, Brailsford SR, et al. Hepatitis E virus in blood components: a prevalence and transmission study in southeast England. Lancet 384 (2014):1766-1773.
- Huzly D, Umhau M, Bettinger D. Transfusion-transmitted hepatitis E in Germany, 2013. Euro Surveillance 19 (2014): 20812.
- Wang B, Meng XJ. Hepatitis E virus: host tropism and zoonotic infection. Curr Opin Microbiol 59 (2021): 8-15.
- Izopet J, Dubois M, Bertagnoli S. Hepatitis E virus strains in rabbits and evidence of a closely related strain in humans, France. Emerg Infect Dis 18 (2012): 1274-1281.
- Waterborne hepatitis E epidemics: identification (2017).
- Kamar N, Izopet J, Pavio N, et al. Hepatitis E virus infection. Nature Review 3 (2017): 1-16.
- Mansuy JM, Bendall R, Legrang-Abravanel F, et al. Hepatitis E Virus Antibodies in blood donors, France. Emerging Infectious Diseases 17 (2011): 12.
- Pavio N, Rose NBJ, Tessé S, et al. Endémicité du virus de l’hépatite E dans le cheptel porcin français et transmissions zoonotiques probables par l’alimentation. Bulletin épidémiologique, santé animale et alimentation 52 (2012).
- Bonnet D, Kamar N, Izopet J, et al. L’hépatite virale E : une maladie émergente Hepatitis E: An emerging disease. La Revue de Médecine Interne 33 (2012): 328-334.
- Alhatlani BY, Aljabr WA, Almarzouqi MS, et al. Seroprevalence of the hepatitis E virus antibodies among blood donors in the Qassim region, Saudi Arabia. Future Virology 16 (2021): 6.
- Fu P, Lin B, Wu B, et al. Hepatitis E virus prevalence among blood donors in Dali, China. Virology Journal 18 (2021): 141.
- Niguse S, Hailekiros H, Buruh G, et al. Seroprevalence and risk factors of Hepatitis E virus infection among pregnant women attending antenatal care in health facilities of Tigray, Northern Ethiopia. Journal of Medical Virology 90 (2018): 1364-1369.
- De Paschale M, Ceriani C, Romano L, et al. Epidemiology of hepatitis E virus infection during pregnancy in Benin. Tropical Medicine and International Health 21 (2016): 108-113.
- Demanou M, Mahamat A, Nimpa MM, et al. First documented outbreak of hepatitis E in Northern Cameroon. Annals of Tropical Medicine and Public Healt 6 (2013): 682-683.
- Traoré KA, Ouoba JB, Huot N, et al. Hepatitis E virus exposure is increased in pork butchers from Burkina Faso. Am J Trop Med Hyg 93 (2015): 1356-1359.
- Yandai FH, Traore KA, Moussa AM, et al. Prevalence and Diversity of Hepatitis Virus Markers among Patients with Acute Febrile Jaundice in Chad. Microbiol Res 12 (2021): 878-887.
- Barro N, Tahita MC, Traore O, et al. Risks associated with practices, processes and environment of ready-to-eat and street-vended foods that lead to contamination by common foodborne viruses. In Hygiene and Its Role in health. P.L. Aderson and J.P. Calhan (2008): 129-153.
- Ndam AWN, Njoya ONM, Kowo RN, et al. Seroprevalence of Hepatitis E Virus Infection and Factors Associated in HIV Infected Patients in Yaoundé (Cameroon). Open Journal of Gastroenterology 10 (2020): 181-186.
- Nouhin J, Madec Y, Prak S, et al. Declining hepatitis E virus antibody prevalence in Phnom Penh, Cambodia during 1996–2017. Epidemiology and Infection 147 (2019): 1-6.
- Yoon Y, Jeong HS, Yun H, et al. Hepatitis E Virus (HEV) Seroprevalence in the general population of the Republic of Korea in 2007–2009: a nationwide cross-sectional study. BMC Infectious Diseases 14 (2014): 517.
- Adjalo DK, Houedakor KZ, Zinsou-Klassou K. Usage des emballages plastiques dans la restauration de rue et assainissement des villes ouest-africaines: exemple de Lomé au Togo. Int J Biol Chem Sci 14 (2020): 1646-1656.
- Modiyinji AF, Amougou-Atsama M, Monamele CG, et al. Seroprevalence of hepatitis E virus antibodies in different human populations of Cameroon. J Med Virol (2019): 1-6.
- Osundare FA, Klink P, Majer C, et al. Hepatitis E Virus Seroprevalence and Associated Risk Factors in Apparently Healthy Individuals from Osun State, Nigeria. Pathogens 9 (2020): 392.
- Lagare A, Ibrahim A, Ousmane S. Outbreak of hepatitis E virus in displaced person camps in Diffa Region, Niger, 2017. Am J Trop Med Hyg 99 (2018): 1055-1057.
- Cevrioglu AS, Altindis M, Tanir HM, et al. Investigation of the incidence of hepatitis E virus among pregnant women in Turkey. J Obstet Gynaecol Res 30 (2004): 48-52.
- Kumar H, Kamar N, Kumar D. Hepatitis E: Current Status in India and Other Asian Countries. J Pure Appl Microbiol 13 (2019): 141-159.
- Tedder RS, Ijaz S, Kitchen A, et al. Hepatitis E risks: pigs or blood—that is the question. Transfusion 57 (2017): 267-272.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 