Surgical Site Infection in Orthopedic and Trauma Surgery at Kinshasa University Clinics
Julien Edunga BOSSA1*, Remy Bayaa MADEE1, Aliocha Natuhoyila NKODILA2, Marie-Ange kalambay MBUYI3, Luc Bakumobatane MOKASSA1
1University of Kinshasa, Department of surgery/ Kinshasa, RD Congo
2Protestant University of Congo, Department of Family Medicine and Primary Care/ Kinshasa, RD Congo
3University of Kinshasa, Department of Pediatrics/ Kinshasa, RD Congo
*Corresponding Author: Julien Edunga BOSSA, University of Kinshasa, Department of surgery/ Kinshasa, RD Congo.
Received: 12 February 2024; Accepted: 20 February 2024; Published: 27 February 2024
Article Information
Citation: Julien Edunga BOSSA, Remy Bayaa MADEE, Aliocha Natuhoyila NKODILA, Marie- Ange Kalambay MBUYI, Luc Bakumobatane MOKASSA. Surgical Site Infection in Orthopedic and Trauma Surgery at Kinshasa University Clinics. Journal of Orthopedics and Sports Medicine. 6 (2024): 29-37.
View / Download Pdf Share at FacebookAbstract
Background: The objective of our study is to identify risk factors, determinants of surgical site infection in our study population and predict the occurrence of surgical site infection according to National nosocomial infection score.
Method: This is a retrospective observational cohort study, conducted in orthopedic and trauma surgery at the Kinshasa University Clinics in Congo/kinshasa, from 2010 to 2021.
Results: A total of 247 patients underwent surgery, 61.1% men and 38.9% women, with a sex ratio of 2H/1F. The mean age was 40.5±18.1 years, with the 20-29 (20.2%) and 30-39 (23.9%) age groups the most represented. The incidence of SSI was 15%, with organ infections predominating (7.7%). A minority, 5.7%, were at high risk of surgical site infection. The national nosocomial infection score was retained as a predictive factor for surgical site infection in at-risk individuals (p=0.033). Male gender [(aOR: 1.93; 95% CI: 1.09-3.43); p = 0.025], emergency surgery [(aOR: 4.58; 95% CI: 1.36-5.45); p = 0.014] and preoperative duration greater than 24 h [aOR: 1.98; 95% CI: 1.02-3.82); p = 0.043] were factors independently and significantly associated with the risk of SSI.
Conclusion: The frequency of SSI is equivalent to that obtained in regions sharing a similar socio-economic context to our own and remains high compared with results from developed countries. Male gender, emergency surgery and preoperative duration of more than 24 hours are factors favoring SSI in our institution, with a National nosocomial infection score retained as a predictive factor.
Keywords
<p>Surgical site infection; Orthopedic and trauma surgery; Risk factor; Determinants; National nosocomial infection score</p>
Article Details
1. Introduction
Nosocomial infection, which is an infection associated with care contracted in a healthcare establishment, is favored by factors linked to the patient's general condition, the therapeutic procedure and the patient's stay in a hospital environment. Depending on the anatomical structures involved, these include urinary tract infections, pulmonary infections, vascular catheter infections, bacteremia and surgical site infections (SSI) [1].
SSI occurs within 30 days of surgery or within 90 days if an implant has been inserted [1,2]. It may be superficial to the incision, deep to the incision or to the organ-space, with the consequence of increasing the morbidity and mortality of the patient affected [1,3]. In orthopedic and trauma surgery, the risk of contracting SSI is low compared to visceral surgery. Despite this low risk, SSI is considered a catastrophe for the patient and a challenge for the surgeon, because of the long hospital stay involved, the financial burden, the imbalance in the patient's homeostasis, and the vital and/or functional risk [3-6].
In order to reduce the risk of SSI worldwide, the World Health Organization (WHO) has drawn up a number of standardized recommendations applicable in both resource-limited and resource-satisfied regions. These recommendations are based on modifiable and non-modifiable SSI risk factors [6]. To improve management of infectious risk in health care establishments, some countries have set up continuous surveillance programs for surgical site infections: the Montreal Orthopaedic SSI Surveillance Pilot Project, the Canadian Nosocomial Infection Surveillance Program (CNISP) in Canada, the Hospital in Europe link for infection control through surveillance in Europe, with 16 member countries (Austria, Belgium, Denmark, France, Finland, England, Germany, Italy, Netherlands, Northern Ireland, Norway, Portugal, Scotland, Spain, Sweden, Wales), the National Nosocomial Infection Surveillance (NNIS) of the Centers for Disease Control and Prevention (CDC) in the USA [7].
In the Democratic Republic of Congo (D.R.C.), a preliminary study carried out in 1993 in the orthopaedic surgery and traumatology department of the Kinshasa University Clinics (CUK) found a 19% incidence of early SSI, and longer hospital stays for infected patients. It was therefore recommended to improve working conditions and step up measures to control related risk factors [8].
The objective of our study is to identify risk factors, determinants of SSI in our study population and predict the occurrence of SSI according to NNIS score in CUK orthopedic and trauma surgery during the period from January 2010 to December 2021.
2. Patients and Methods
2.1 Design and sitting of study
This is a retrospective observational cohort study of patients operated on for osteoarticular conditions in an aseptic zone at the orthopedic surgery and traumatology department of CUK/D.R.C, during the period from February 2010 to December 2021.
The surgical operating room, community hospitalization and private hospitalization of the CUK orthopedic surgery department served as the study setting. We included in our study any patient who underwent surgery for an osteoarticular condition during the study period, and whose incision was made in a healthy area. We excluded any patient with a septic osteoarticular lesion whose incision is performed in a septic area.
2.2 Participants
A total of 1086 surgical procedures were performed in the CUK osteoarticular surgery operating room during the period from January 01, 2010 to December 31, 2021. We found 294 files in good condition, 247 of which met our inclusion criteria and constituted our study population.
2.3 Data sources
Data were collected from the various patient files found in community and private hospitalization, in the consultation unit, supplemented by some operating room registers. Data were collected using a pre-established data collection form, based on the model of the Quebec National Institute of Public Health [7].
2.4 Variables
For each patient in the cohort, the following data were collected according to the standardized SSI surveillance data collection form, proposed by the Quebec National Institute of Public Health [8]:
- Demographic characteristics: age, sex;
- Preoperative characteristics: ALTEMEIER class, ASA (American Society of Anesthesiologist) score, etiology, reception
- Intraoperative characteristics: type of operation, duration of operation, procedure performed, calculation of NNIS (National Nosocomial Infection Score) index [9-12];
- Post-operative patient characteristics: diagnosis of SSI, type of SSI and length of hospital stay
2.5 Biais
The diagnosis of incident cases (SSI) was based on the clinical criteria proposed by CDC Atlanta, with bacteriological evidence for certain patients. Each case of SSI was identified by an orthopedic surgeon and validated by a staff meeting, with a view to improving management. As a result, we believe there was a diagnostic bias.
2.6 Study size
The sample size was defined by the number of orthopaedic and traumatological surgery patients who underwent surgery during the study period, and whose variables of interest were clearly identified in the medical records.
2.7 Statistical analysis
Data were entered, cleaned and encoded on the computer using Microsoft Office Excel 2010. Incident cases were defined by the surgeon's clinical diagnosis of SSI. Statistical analyses were performed using SPSS version 24 software and presented in the form of Tables and Figures. Descriptive analyses were mean, standard deviation for quantitative data with Gausian distribution and median (EIQ = inter quantile standard deviation) for data with non-Gaussian distribution and the Student's t-test was used to compare means, the Man Whitney test to compare medians, and Pearson's Chi-square or Fischer's Exact tests to compare proportions. Bivariate and multivariate logistic regression were used to assess the effects of variables associated with infectious risk. Logistic regression used the stepwise method in bivariate analysis. Variables significantly associated with infectious risk were entered into the multivariate model, and adjusted Odd Ratios and their 95% confidence intervals were calculated, enabling the degree of association to be assessed. For all tests used, p<0.05 was considered to be the statistically significant threshold.
2.8 Ethical considerations
This study was carried out anonymously and in strict compliance with medical ethics. We certify that no human experimentation took place during the course of this work. We have collected data from our patients' medical records with strict respect for anonymity and with the consent of the person concerned.
3. Results
A total of 1086 surgical procedures were performed in the CUK osteoarticular surgery operating room during the period from January 01, 2010 to December 31, 2021. We found 294 files in good condition, 247 of which met our inclusion criteria and constituted our study population.
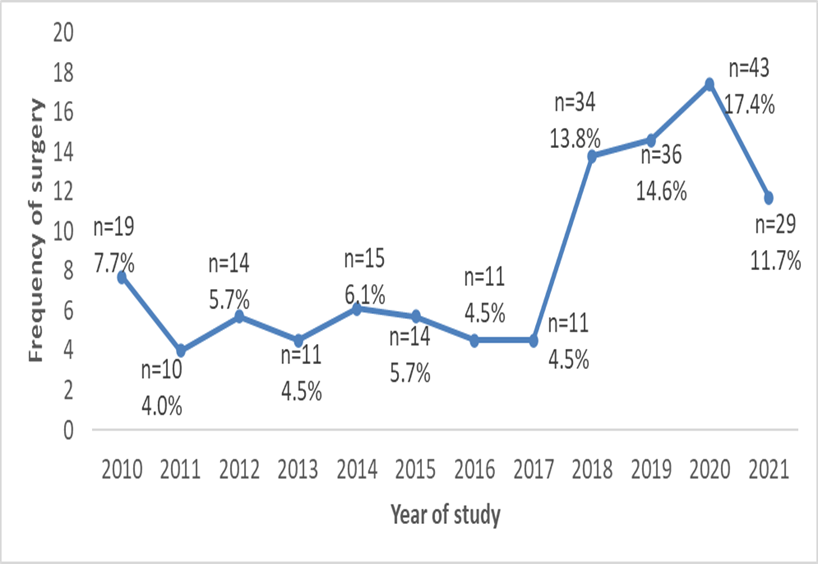
We noted a higher frequency in 2020, 2019 and 2018 of 17.4%, 14.6% and 13.8% respectively. The number of procedures declined from 2010 to 2011, remaining stable from 2011 to 2017, then increasing from 2017 to 2021, with a peak in 2020. The average number of patients operated on over these 12 years is 20.5±8.1 patients, ranging from 10 to 43 per year (Figure 1).
The majority of patients operated on were male, representing 61.1% (151/247) versus 38.9% (96/247) female, with a sex ratio of 2H/1F and the mean age of the study population was 40.5±18.1 years. The youngest patient operated on was 8 years old, and the oldest was 92. The median age was estimated at 36 (26-53) years. The most common age groups were 20-29 and 30-39, with 20.2% (50/247) and 23.9% (59/247) respectively (Table 1).
|
Variable |
N=247 |
Percentage |
|
Age group |
||
|
<20 years |
27 |
10.9 |
|
20-29 years |
50 |
20.2 |
|
30-39 years |
59 |
23.9 |
|
40-49 years |
35 |
14.2 |
|
50-59 years |
29 |
11.7 |
|
60-69 years |
26 |
10.5 |
|
≥70 years |
21 |
8.5 |
|
Reception |
||
|
Emergency |
186 |
75.3 |
|
Elective |
61 |
24.7 |
|
Altemeier's class |
||
|
Clean |
192 |
77.7 |
|
Clean contaminated |
38 |
15.4 |
|
Contamined |
10 |
4 |
|
Dirty or infected |
7 |
2.8 |
|
ASA score |
||
|
I |
200 |
81 |
|
II |
40 |
16.2 |
|
III |
7 |
2.8 |
|
Etiology |
||
|
Non-trauma |
63 |
25.5 |
|
Trauma |
184 |
74.5 |
|
Polytrauma |
||
|
Yes |
31 |
12.6 |
|
No |
216 |
87.4 |
|
Preoperative time |
||
|
< 24 h |
55 |
22.3 |
|
> 24 h |
192 |
77.7 |
|
Operator |
||
|
Senior |
172 |
69.6 |
|
Junior |
75 |
30.4 |
|
Type of intervention |
||
|
Primary |
218 |
88.3 |
|
Secondary |
29 |
11.7 |
|
Intervention time |
||
|
<1h |
33 |
13.4 |
|
1-2h |
119 |
48.2 |
|
>2h |
95 |
38.5 |
|
ISO |
||
|
Non |
210 |
85 |
|
Organ/cavity |
19 |
7.7 |
|
Yes Deep |
3 |
1.2 |
|
Superficial |
15 |
6.1 |
Table 1: General parameter of population, recruited at CUK-Orthopedics and Traumatology Department/ DRC, from 2010 to 2021 (N=247).
There was a decrease in the frequency of intervention with increasing age. Table 1 shows that 186 patients (75.3%) were seen in the emergency department, the majority with clean wounds (77.7%) and contaminated wounds (15.4%). The majority of patients had an ASA score of I (81%), traumatic origin was found in 74.5% of patients, with 31 (12.6%) polytraumatized, and 77% of patients underwent surgery more than 24 hours after admission.
In our study, the majority of patients were operated on by senior surgeons (172, 69.6%), and most procedures were primary (218, 88.3%). Mean operative time was 2.2±1.4 hours, with extremes ranging from 0.25 to 8 hours. The majority of interventions lasted between 1-2 hours (48.2%) (Table 1) and the most frequently used procedure was osteosynthesis in 65.6%, followed by amputation / disarticulation in 6.9% (Table 2).
|
Procedure |
Numbers |
Percentage |
|
Osteosynthesis |
162 |
65.6 |
|
Amputation/disarticulation |
17 |
6.9 |
|
Intervention on joints, except joint prosthesis |
15 |
6.1 |
|
Double osteosynthesis |
15 |
6.1 |
|
Intervention on bone (except skull and spine), without osteosynthesis |
14 |
5.7 |
|
Removal of osteosynthesis materials |
12 |
4.9 |
|
Surgery of muscle, aponeurosis, tendons, ligaments |
7 |
2.8 |
|
Hip joint prosthesis |
2 |
0.8 |
|
Amputation/disarticulation + Intervention on joints, except joint prosthesis |
1 |
0.4 |
|
Amputation/disarticulation + osteosynthesis |
1 |
0.4 |
|
Total hip joint prosthesis |
1 |
0.4 |
|
Total |
247 |
100 |
Table 2: Distribution of study population by surgical procedure carried out at CUK-Orthopedics and Traumatology Department/ DRC, from 2010 to 2021 (N=247).
During our study period, 37 cases of SSI were diagnosed out of 247 patients operated on, representing a frequency of 15%. Organ or cavity infection was predominant, with 19 cases corresponding to 7.7% (Table 1). The frequency of SSI was significantly higher in male patients (p=0.035), with a M/F sex ratio of 3.1. The frequency of SSI in patients aged between 30 and 39 years was visibly higher than in other patients, at 29.7% (11/37), but a comparison of frequencies showed no significant difference (p=0.793) (Table 3).
|
Variables |
No ISO |
Presence of ISO |
p |
|
(n=210) |
(n=37) |
||
|
Age |
0.793 |
||
|
<20 years |
22(10.5) |
5(13.5) |
|
|
20-29 years |
45(21.4) |
5(13.5) |
|
|
30-39 years |
48(22.9) |
11(29.7) |
|
|
40-49 years |
29(13.8) |
6(16.2) |
|
|
50-59 years |
24(11.4) |
5(13.5) |
|
|
60-69 years |
24(11.4) |
2(5.4) |
|
|
≥70 years |
18(8.6) |
3(8.1) |
|
|
Gender |
0.035 |
||
|
Male |
123(58.6) |
28(75.7) |
|
|
Female |
87(41.4) |
9(24.3) |
|
|
ASA score |
0.578 |
||
|
I |
170(81.0) |
30(81.1) |
|
|
II |
34(16.2) |
6(16.2) |
|
|
III |
6(2.9) |
1(2.7) |
|
|
Pre-operative time >24 h |
157(74.8) |
33(89.2) |
0.026 |
|
Trauma |
154(73.3) |
30(81.1) |
0.217 |
|
Altemeier's class |
0.004 |
||
|
Clean |
172(81.9) |
20(54.1) |
|
|
Clean contaminated |
28(13.3) |
10(27.0) |
|
|
Contaminated |
6(2.9) |
4(10.8) |
|
|
Dirty or infected |
4(1.9) |
3(8.1) |
|
|
Operator |
<0.001 |
||
|
Senior |
164(78.1) |
8(21.6) |
|
|
Junior |
46(21.9) |
29(78.4) |
|
|
Intervention time |
0.005 |
||
|
<1 h |
32(15.2) |
1(2.7) |
|
|
1-2 h |
98(46.7) |
21(56.8) |
|
|
>2 h |
80(38.1) |
15(40.5) |
|
|
Length of stay >30 days |
143(68.1) |
32(86.5) |
0.015 |
|
NNIS |
0.033 |
||
|
0 |
135(64.3) |
16(43.2) |
|
|
1 |
63(30.0) |
19(51.4) |
|
|
2 |
12(5.7) |
2(5.4) |
Table 3: General characteristics of patients depending on ISO, at CUK-Orthopedics and Traumatology Department/ DRC, from 2010 to 2021 (N=247).
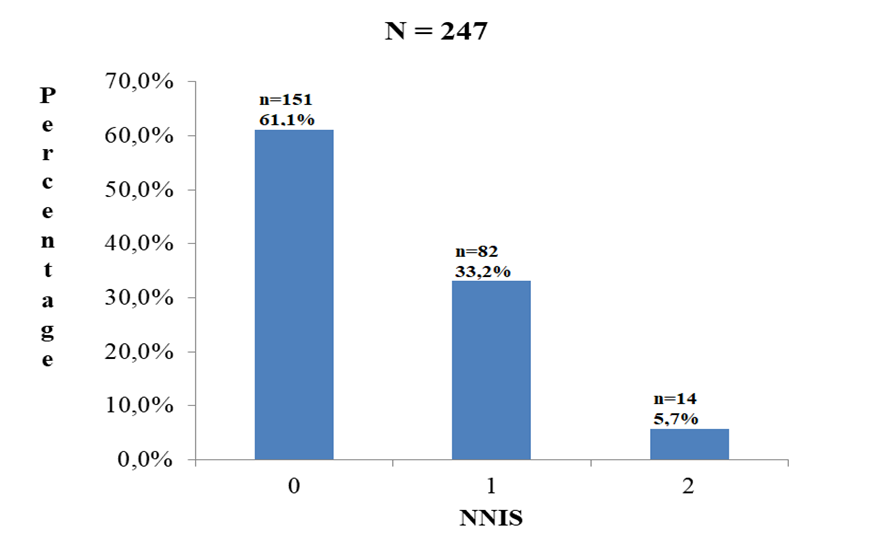
The frequency of SSI was significantly higher in patients admitted to the emergency department (p=0.039), in those whose preoperative duration exceeded 24 hours (p=0.026) and varied according to wound type, but inversely with septic status (p=0.004) (Table 3). The frequency of SSI was significantly higher in patients operated on by a junior doctor (p=0.001), in those whose operation lasted more than one hour (p=0.005) and in those whose post-operative hospital stay exceeded 30 days (p=0.015) (Table 3). Figure 2 shows that the risk of SSI in our study population, as assessed by the NNIS score, is predominantly represented by a NNIS score of 0, with a total of 151 patients (61.1%). A minority, 14 patients (5.7%), had a high risk of SSI and we found that NNIS score significantly predicted the occurrence of SSI in at-risk individuals (p=0.033) (Figure 2).
In univariate analysis, male gender, secondary operation, emergency operation, traumatic etiology and preoperative duration of more than 24 h were the factors associated with the risk of infection. After adjustment, multivariate analysis showed that male gender [(aOR: 1.93; 95% CI: 1.09-3.43); p = 0.025], emergency surgery [(aOR: 4.58; 95% CI: 1.36-5.45); p = 0.014] and preoperative duration greater than 24 h [aOR: 1.98; 95%CI: 1.02-3.82); p = 0.043] were the factors independently and significantly associated with the risk of infection (Table 4).
|
Variables |
Uni-varied analysis |
Multi-varied analysis |
||
|
p |
OR (95%CI) |
p |
aOR (95%CI) |
|
|
Sex |
||||
|
Female |
1 |
1 |
||
|
Male |
0.027 |
1.84 (1.07-3.17) |
0.025 |
1.93 (1.09-3.43) |
|
Type of intervention |
||||
|
Primary |
1 |
1 |
||
|
Secondary |
0.044 |
2.19 (1.89-5.29) |
0.542 |
1.45 (0.44-4.81) |
|
Reception |
||||
|
Elective |
1 |
1 |
||
|
Emergency |
0.002 |
2.98 (1.51-5.86) |
0.014 |
4.58 (1.36-5.45) |
|
Etiology |
||||
|
Non-trauma |
1 |
1 |
||
|
Trauma |
0.045 |
1.84 (1.09-3.42) |
0.228 |
1.95 (0.66-5.76) |
|
Preoperative time |
||||
|
≤ 24 h |
1 |
1 |
||
|
> 24 h |
0.025 |
2.0 (1.09-3.63) |
0.043 |
1.98 (1.02-3.82) |
Table 4: Determinants of ISO in the study population, at CUK-Orthopedics and Traumatology Department/ DRC, from 2010 to 2021 (N=247).
4. Discussion
During our study period, from January 2010 to December 2021, 1,086 surgical procedures were recorded in the CUK osteoarticular surgery operating theatre, with 247 cases meeting our inclusion criteria and constituting our study population. We noted a higher frequency in 2020, 2019 and 2018 of 17.4%, 14.6% and 13.8% respectively. The number of procedures declined from 2010 to 2011, remaining stable from 2011 to 2017, then increasing from 2017 to 2021, with a peak in 2020. The average number of patients operated on over the 12-year period was 20.5±8.1, ranging from 10 to 43 per year. This variation was linked to a failure to archive files, which explains an ascending frequency over the years. The majority of patients operated on were male, representing 61.1% (151/247) versus 38.9% (96/247) female, with a sex ratio of 2H/1F. This male predominance is found in the majority of studies carried out in the D.R. Congo [8,13-15] and elsewhere in Africa and Asia [16,17]. This is justified by the fact that men, being the hub of the household, are called upon to frequent road traffic for their mobility, and are exposed to occupations at risk of accident, unlike women, who for the most part are responsible for housework. In France, ortho-traumatological surgery is predominantly performed by women (56.9%), which can be explained by bone fragility linked to osteoporosis following the menopause, given that the French population is ageing [18]. We note that the most represented age groups were 20-29 and 30-39, constituting a young adult population, with respectively 20.2% (50/247) and 23.9% (59/247), and there was a decrease in the frequency of intervention with increasing age. These results are in harmony with those of MOBA and colleagues, who found a high frequency of road traffic trauma in this same population in 6 different towns in the DRC [13]. Benie bi vroh and colleagues [19] in Côte d'ivoire noted a high frequency of traffic accidents in this same population. This situation could be explained by the fact that this category of people is not only part of the student population, but also of the working population, and is therefore a mobile population.
During our study period, we noted some 37 cases of SSI, representing a frequency of 15%, with a predominance of organ or cavity infections, 19 cases corresponding to 7.7%. In 1993, Mutombo and colleagues [8] studied the same site in Kinshasa and found a frequency of 19%, considering only cases of aseptic surgery. Bercion et al. [20] in the Central African Republic found 18%. Our results are slightly higher than those of IDE in Cotonou, who found a frequency of 9.59%, with a predominance of deep SSI in 85.2% of cases, bearing in mind that the study population was made up of patients who had undergone clean surgery with approximately 72 hours' antibiotic prophylaxis [16]. Afifi and Baghagho [21] in Egypt found an 8.2% frequency of SSI after a 3-month prospective study. A prospective study carried out in Brazil in 2015 revealed a frequency of 3.9%, low compared with the African results [22]. The rate of SSI is very low in France, with 1.37% and 1.10% respectively in orthopedic and traumatological surgery. Being better organized, France has set up a network for the alert, investigation and surveillance of nosocomial infections (RAISIN) with a view to detecting any changes and taking early action [18,23,24]. We believe that the variation in the frequency of SSIs is inversely proportional to the level of development and organization of the healthcare sector. The frequency of SSI was significantly higher in male patients (p=0.035), with a M/F sex ratio of 3.1. These results are similar to those of IDE and colleagues, who also found a clear predominance of SSI in men, with a sex ratio identical to ours, in the Beninese population in 2018 [16]. According to the ISO-RAISIN/2015 report, there is no significant difference between men and women in a Caucasian population, who have a higher standard of living than Africans [18]. In the literature, we did not find elements that could justify this difference in SSI frequency between men and women. In our study, the frequency of SSI is visibly higher in people aged between 30 and 39, with no significant difference when comparing frequencies (p=0.793). Our results are similar to the ISO-RAISIN/2015 report in France, which noted no significant relationship between SSI and patient age (p=0.63) in traumatology, in contrast to orthopedic surgery, where SSI is proportionally high as a function of age (p=0.02). This latter trend is justified by the comorbidity assessed by the ASA score, which showed a 1.67 incidence of SSI in patients with an ASA score of 3, 4, 5 (p=0.0001) [18]. Bercion and colleagues [20] in the Central African Republic found no relationship between age and the occurrence of SSI, following a prospective study carried out in 2007. In the light of our results, the frequency of SSI was significantly higher in patients whose preoperative duration exceeded 24 hours (p=0.026) and varied according to wound type, but inversely with septic status (p=0.004). This inversion of the septic risk could be justified by the irrational use of antibiotics in our departments, not complying with the indications for antibiotic prophylaxis according to Altemeier's classes, thus inducing germ selection [22,25]. Bercion and colleagues [20] in the Central African Republic noted no difference between patients operated on in less or more than 24 hours (p=0.005). The results in relation to preoperative duration are similar to those of the ISO-RAISIN/2015 report in orthopedics (p=0.0001), unlike in trauma surgery where there is no statistically significant evidence (p=0.21), and there was also a statistically significant rise in the incidence of SSI in Altemeier class 3 and 4 (3.09%, p=0.0001), in both orthopedics and trauma [18]. The frequency of SSI was significantly higher in patients undergoing emergency surgery (p=0.039), in those whose operating time exceeded one hour (p=0.005) and in those operated on by a junior (p<0.001). According to the ISO-RAISIN/2015 report in France, our results corroborate our findings insofar as there is an increase in the incidence of SSI (2.22%, p=0.0001) in orthopedics unlike traumatology (p=0.21), we find more SSI when the duration of the intervention exceeds the 75th percentile (p=0.0001). This report does not consider the quality of the operator [18]. Bercion et al. [20] in the Central African Republic found that there were more SSIs in patients whose operation lasted longer than 1 hour (p=0.001). The majority of our patients (61.1%) had a low risk of SSI, reflected by an NNIS index of 0. Abalo et al. [26] in Togo also had a predominance of patients with no risk of infection, with an NNIS index of 0 (69 patients, equivalent to 59.4%). In traumato-orthopedics, the majority of patients are victims of an accident or present to hospital with a condition that is not directly life-threatening. We find that the NNIS score significantly predicts the occurrence of SSI in at-risk individuals (p=0.033). This predictive power is supported by Abalo and colleagues in Togo, who note a 100% incidence of infection in patients with an NNIS index of 3 [26] Touré et al. [27] in Benin also reported a similar finding, with p=0.017. Ercole et al. [28] in Brazil, following a study evaluating the predictive power of the NNIS score in orthopedic surgery patients, found that this score was a moderate predictor of SSI when the incidence of infection was low. He proposed the integration of 4 other factors (the implant, the number of people in the operating room, the type of anesthesia and the health status of the hospital) in his prediction model, which to date has not been validated in the rest of the world [28].
In univariate analysis, male gender, secondary operation, emergency operation, traumatic etiology and preoperative duration of more than 24 h were significantly associated with SSI. Multivariate analysis, after adjustment, determined that male gender [(aOR: 1.93; 95%CI: 1.09-3.43); p = 0.025], the procedure performed as an emergency [(aOR: 4.58; 95%CI: 1.36-5.45); p = 0.014] and preoperative duration greater than 24 h [(aOR: 1.98; 95%CI: 1.02-3.82); p = 0.043] were factors independently and significantly associated with SSI. The risk factors for SSI reported in our study are comparable to those described in the literature [29-32]. Eriksen et al. [33] in Tanzania demonstrated in a study that during preoperative hospitalization, the microbial skin flora undergoes a change from the 3rd and 4th day of hospitalization, which would favor the occurrence of SSI.
5. Conclusion
The present study, devoted to the evaluation of SSI in CUK orthopedic and traumatological surgery, based on the predictive power of the NNIS score for infectious risk, and by determining the factors associated with this same phenomenon, gives an idea of the evolution of preventive measures for SSI in the orthopedic and traumatological surgery department on the one hand, and the level of hospital hygiene on the other in our institution. The frequency of SSI in the present study was 15%. This may seem low, but it should not be overlooked in view of the individual impact on the patient (social, psychological, functional and sometimes vital), on his or her family and on the nursing staff. Male gender, emergency surgery and a preoperative duration of more than 24 hours are factors favoring SSI in our institution, and the NNIS score is retained as a predictor of SSI.
What is known
To date, no study with this methodological orientation has been carried out in this population.
What this Study Adds
This study, carried out in the orthopedic surgery and traumatology department of CUK in the DRC, is unique in that:
- It identifies the risk factors for surgical site infection, as well as the determinants of this catastrophe in this population
- It also demonstrates the predictive potential of the NNIS score in determining surgical site infection in this population
Conflict of interest and source of funding
The authors declare no conflicts of interest
Authors contributions
The authors wrote the manuscript, collected and analyzed the data
All authors have read and approved the final version of the manuscript
References
- CDC/NHSN. Surgical site infection event (SSI) [Internet]. janv [cité 18 févr 2024] (2024). Disponible sur: https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf
- Maître S, Pirrello T, Hoffmeyer P, et al. Measures against surgical site infections in orthopaedic surgery. Rev Med Suisse 25 (2012): 890-893.
- Sganga G, Baguneid M, Dohmen P, et al. Management of superficial and deep surgical site infection: an international multidisciplinary consensus. Updat Surg 73 (2021): 1315-1325.
- Tucci G, Romanini E, Zanoli G, et al. Prevention of surgical site infections in orthopaedic surgery: a synthesis of current recommendations. Eur Rev Med Pharmacol Sci 23 (2019): 224-239.
- Kolasinski W. Surgical site infections - review of current knowledge, methods of prevention. Pol Przegl Chir 91 (2018): 41-47.
- Organization WH. Global guidelines for the prevention of surgical site infection. World Health Organization (2016).
- Lowe AM. Surveillance of Surgical Site Infections: Tools and Methodologies for Healthcare Settings. desLibris (2014).
- Mutombo DP, Krubwa Y, Kalunda M. Infections post opératoires précoces en chirurgie ostéoarticulaire à Kinshasa. Etude préliminaire de facteurs pathogéniques. A propos de 189 interventions. Médecine D’Afrique Noire 40 (1993).
- Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care–associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. Juin 36 (2008): 309-332.
- RAISIN, CLIN-Ouest C, CLIN-Paris-Nord C, et al. Surveillance des infections du site opératoire en France en 1999 et 2000. Rapport RAISIN (2003).
- Ling ML, Apisarnthanarak A, Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control 8 (2019): 174.
- Flouchi R, Far ME, Hibatallah A, et al. Incidence of surgical site infections and prediction of risk factors in a hospital center in Morocco. J Infect Dev Ctries 16 (2022): 1191-1198.
- Moba JN, Nkodila AN, Mokassa LB, et al. Trend Over Six Years of Incidence of Mortality Related To Road Traffic Accidents in Six Cities of the Democratic Republic of the Congo: A Retrospective Survey in Population Based. J Environ Sci Public Health 6 (2022): 257-261.
- Nzanzu ES, Mokassa LB. Issue of locked intramedullary nailing of the femur and the tibia in two hospitals in the Democratic Republic of Congo. Rév Méd Gd Lacs 12 (2021): 37-44.
- Lembalemba B, Kitoko A, Bakumobatane M, et al. Epidemiological and anatomopathological profile of Dupuytren's Fractures in Kisangani-R.D Congo. KisMed 10 (2020): 394-400.
- Idé G, Wahab MA, Hama Y, et al. Surgical site infections in clean trauma bone surgery at Cotonou. Health Sci Dis 19 (2018).
- Khan MS, Rehman S, Ali MA, et al. Infection in orthopedic implant surgery, its risk factors and outcome. J Ayub Med Coll Abbottabad 20 (2008): 23-25.
- Surveillance des infections du site opératoire dans les établissements de santé français. Résultats 2015 [Internet]. Disponible sur: https://www.santepubliquefrance.fr/notices/surveillance-des-infections-du-site-operatoire-dans-les-etablissements-de-sante-francais.-resultats-2015
- Benie Bi Vroh 1 2 J, Tiembré 1 2 I, Ekra 1 2 DK, et al. Determinants of Fatal Road Traffic Injuries in Côte d’Ivoire from 2002 to 2011. Santé Publique 28 (2016): 647-653.
- Bercion R, Gaudeuille A, Mapouka PA, et al. Surgical site infection survey in the orthopaedic surgery department of the "Hôpital communautaire de Bangui," Central African Republic. Bull Société Pathol Exot 100 (2007): 197-200.
- Afifi IK, Baghagho EA. Three months study of orthopaedic surgical site infections in an Egyptian University hospital. Int J Infect Control 6 (2010).
- Vieira G de D, Mendonça HR, Alves T da C, et al. Survey of infection in orthopedic postoperative and their causative agents: a prospective study. Rev Assoc Medica Bras 61 (2015): 341-346.
- Mabit C, Marcheix PS, Mounier M, et al. Impact of a surgical site infection (SSI) surveillance program in orthopedics and traumatology. Orthop Traumatol Surg Res OTSR 98 (2012): 690-695.
- Grammatico-Guillon L, Banaei-Bouchareb L, Solomiac A, et al. Validation of the first computerized indicator for orthopaedic surgical site infections in France: ISO-ORTHO. Antimicrob Resist Infect Control 12 (2023): 44.
- Hawn MT, Richman JS, Vick CC, et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg juill 148 (2013): 649-657.
- Abalo A, Walla A, Ayouba G, et al. Surgical site infection (SSI) in orthopaedics’ patients in a developing country. Rev Chir Orthopédique Traumatol 96 (2010): 112-117.
- Toure L, Lawson E, Chigblo P, et al. Incidence, etiology and risk factors of surgical site infections in orthopedics-traumatology in Cotonou. Health Sci Dis 21 (2020).
- Ercole FF, Chianca TCM, Duarte D, et al. Surgical site infection in patients submitted to orthopedic surgery: the NNIS risk index and risk prediction. Rev Lat Am Enfermagem 19 (2011): 269-276.
- Migaud H, Senneville E, Gougeon. The risk of infection in orthopaedic surgery/ Encyclopédie médico-chirurgicale. Elsevier Masson (2005).
- Ngaroua N, Ngah JE, Bénet T, et al. Incidence of surgical site infections in sub-Saharan Africa: systematic review and meta-analysis. Pan Afr Med J 24 (2016).
- Picard J, Nkoumazok B, Arnaud I, et al. Utilisation des comorbidités du PMSI pour l’ajustement du risque d’infection du site opératoire. Médecine Mal Infect Form 2 (2023): S81-82.
- Martin ET, Kaye KS, Knott C, et al. Diabetes and Risk of Surgical Site Infection: A Systematic Review and Meta-analysis. Infect Control Hosp Epidemiol 37 (2016): 88-99.
- Eriksen HM, Chugulu S, Kondo S, et al. Surgical-site infections at Kilimanjaro Christian Medical Center. J Hosp Infect 55 (2003): 14-20.


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 