The Benefit of Locked Plate in the Management of Osteoporotic Distal Femur Fracture in the Elderly
Conde Mamady Sekou*, Camara Ibrahima Sory, Bah Amadou Tanou, Diallo Hawa Lamarana, Ba Papa Amadou, Niang Coumba Diouf
Traumatology and Orthopedics Department, Military principal Hospital, Cheikh Anta Diop University, Dakar, Senegal
*Corresponding Author: Conde Mamady Sékou, Traumatology and Orthopedics Department, Military principal Hospital, Cheikh Anta Diop University, Dakar, Senegal.
Received: 08 December 2025; Accepted: 17 December 2025; Published: 24 December 2025
Article Information
Citation: Conde Mamady Sekou, Camara Ibrahima Sory, Bah Amadou Tanou, Diallo Hawa Lamarana, Ba Papa Amadou, Niang Coumba Diouf. The Benefit of Locked Plate in the Management of Osteoporotic Distal Femur Fracture in the Elderly. Journal of Orthopedics and Sports Medicine. 7 (2025): 293-296.
View / Download Pdf Share at FacebookAbstract
Introduction: Osteoporotic distal femur fractures are becoming increasingly common in the elderly. The purpose of this study was to evaluate the efficacy of locked plate in the management of osteoporotic distal femur fractures in elderly.
Materials and method: This was an observational and descriptive study. Patients underwent surgery between July 1, 2023, and June 30, 2024. Patients had a distal femur fracture on porotic bone classified according to the the Association for the Study of Osteosynthesis criteria. Fractures fixation were done by a lateral locked plate. The efficacy of the plate fixation was evaluated by analyzing radiological (anatomical angles and bone union), clinical and functional (satisfaction, pain, gait, knee mobility, morphotype, knee stability, limb inequality) parameters.
Results: The series included 14 patients. There were 2 men and 12 women. The mean age was 75.29 (61 and 96) years. The fractures were type A2 (n=7), A3 (n=5), C2 (n=1) and C3 (n=1). The mean surgical time was 105.35 (85 and 150) minutes. The mean follow-up was 8 (5 and 10) months. The fractures healed between 3 and 6 months. The anatomical axes were correct in all cases. The mean anatomical posterior distal femur angle was 83.07° (80 and 86), that of anatomical lateral distal femoral angle was 80.93° (79 and 83). The mean knee flexion was 97.93° (50 and 131). The knee was painless (n=11). All patients were satisfied. No knee instability was observed. Limb length discrepancy was less than 2 cm in two patients. The mean functional international knee society score was 87.1 (80 and 95). Complications were observed in 4 patients.
Conclusion: Locked plate fixation of distal femur fractures on porotic bones in elderly people allows fracture healing, restores anatomical axes of the distal femur and gives satisfactory knee functional outcomes in the medium term.
Keywords
<p>Elderly; Distal femur fracture; Locked plate; Osteoporosis</p>
Article Details
1. Introduction
Distal femur fractures (DFF) account for 4 to 6% of all femoral fragility fractures, with an overall annual incidence of 4.5/100.000 in the general population [1]. Approximately 50% of these fractures affect the elderly; this constitutes a significant cause of morbidity and mortality in elderly population [2]. In these fractures, low energy trauma resulting from a fall from the standing height predominates as the mechanism of injury [3-6].
The occurrence of osteoporotic DFF is a current epidemic, and its management represents a major burden for our society, which continues to grow up [7]. In most cases, the problem is not the soft tissues or the type of fracture, but the poor quality of the bone stock, which leads to insufficient implant anchorage with hardware loosening, malunion, or nonunion [7].
Locked plate (LP) is a widely used implant in the management of osteoporotic fractures, with good reported results [8]. It is characterized by a finer screw pitch, allowing for better anchorage in the thin cortical bone, and thus minimizing the risk of hardware loosening [7]; In addition, it ensures effective stabilization of bone fragments [9] and promotes early mobilization [8].
Studies evaluating the efficacy of LP in the management of osteoporotic DFF in elderly are few in number, with inconsistent results [10,11].
The purpose of this study was to evaluate the efficacy of locked plate in the management of osteoporotic distal femur fractures in elderly.
2. Patients and Method
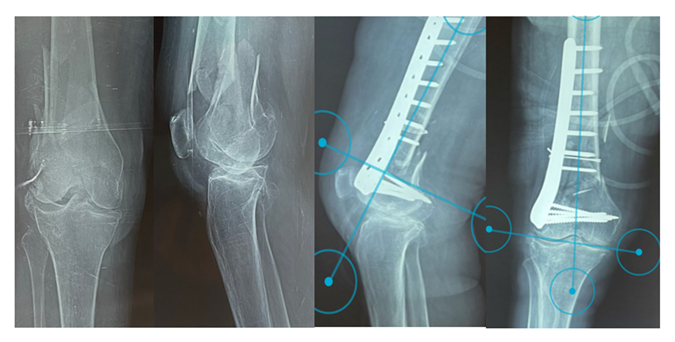
This was an observational and descriptive study. It was conducted on the records of patients hospitalized between July 1, 2023, and June 30, 2024. The patients had DFF on porotic bone (fracture caused by low energy trauma, intraoperative bone fragility), classified according to the criteria of the Association for the Study of Osteosynthesis (AO) [12,13]. Patients with an open or unicondylar fracture were managed using others osteosynthesis material were not included as well as those lost to follow-up or who declined to participate in the study. Fractures were reduced and fixed using a lateral LP (Figure 1). The studied parameters were patient age, gender, previous autonomy, comorbidities, circumstances and mechanism of injury, immediate complications, fracture type, and associated injuries. All procedures were performed under spinal anesthesia, with the patient in the supine position on a standard operating table and the contralateral lower limb supported by a gynecological support.
A lateral approach to the thigh was performed in all patients. After plate fixation of the fracture, the stability of the assembly and the knee was assessed. Bone grafting was performed in a case of significant metaphyseal bone loss; and cerclage wiring was used in a case of a very complex fracture. Rehabilitation began immediately postoperatively with passive knee mobilization. Weight-bearing on the operated leg was strictly prohibited until consolidation. The efficacy of the osteosynthesis was evaluated by measuring anatomical angles of the distal femur: anatomical lateral distal femoral angle (aLDFA), and anatomical posterior distal femoral angle (aPDFA); bone union (disappearance of the fracture line, ferrule callus formation, and recalcification); and clinical and functional parameters according to international knee society score (IKSS) (patient satisfaction, pain, gait, knee mobility, knee morphotype, knee stability, and leg length discrepancy).The functional IKSS ranges from 0 to 100; with the best functional score being 100.
The operating room and hospitalization registers, as well as patient medical records, were used to collect data. Data entry was performed using Microsoft Word 2021. statistical data were entered and analyzed using Sphinx V5.1 software. Informed consent was obtained from all patients.
3. Results
The series comprised 14 patients: 2 men and 12 women. The male-to-female ratio was 0.16. The mean age was 75.29 years with a range of 61 and 96. All patients had experienced falls from standing height. The right lower limb was affected in the same proportion as the left (n=7). Nine (9) patients had comorbidities: hypertension (n=7), diabetes (n=1), obesity (n=2), knee stiffness (n=1), and hip stiffness (n=1). The mean Parker score was 7.71 with a range of 6 and 9. The fracture type was A2 (n=7), A3 (n=5), C2 (n=1), and C3 (n=1). One (1) patient had an associated obturator foramen fracture. All patients had a fracture associated with gonarthrosis (Figure 1).
Upon admission, patients received adhesive traction (n=12) and a led splint (n=2) as a temporary measure. The mean length of hospital stay was 13.5 with a range of 8 and 19 days. The mean time to surgery was 10.64 with a range of 6 and17 days. The mean surgery time was 105.35 with a range of 85 and 150 minutes. The mean follow-up was 8 with a range of 5 and 10 months.
Fractures healed between 3 and 6 months.
Postoperative anatomical axes were identical to those at the last follow-up; the mean aPDFA was 83.07° with a range of 80° and 86°, and the mean aLDFA was 80.93° with a range of 79° and 83° (Figure 1). The mean knee flexion was 97.93° with a range of 50° and 131° (Figure 2). Knee extension was full in all cases. No axial deformity of the limb was observed. The knee was painless (n=11), with mild pain (n=2), and moderate pain (n=1). No knee instability was observed. All patients were satisfied. The mean functional IKS score was 87.1 with a range of 80 and 95. Complications were observed in 4 patients: knee stiffness (n=1), early infection associated to knee stiffness (n=1), leg length discrepancy less than 2 cm (n=1) and ischemic stroke (n=1).
4. Discussion
DFF on porotic bone in the elderly, most often with multiple comorbidities, are becoming increasingly common, following a low energy trauma. In this series, the sample size was small and the follow up time was short; however, patients were followed up prospectively. Fractures were comminuted. Bone union was achieved in all cases. Anatomical alignment was correct in all patients. Knee function was satisfactory.
DFF occur in older people with osteoporosis, similarly to high-energy trauma fractures that occur in younger people [14]. These fractures are often comminuted in older people [2]. The time required to treat these fractures depends on the context [15]. The bone union time depends on the complexity of the fracture line, the size of the skin opening, the stability of the osteosynthesis, and the quality of the initial management [12]. Consolidation periods can take up to 6 months. Shorter periods [11], and longer [10] are postponed. The normal anatomical axes of the distal femur (aLDFA and aPDFA) are respectively between (79°-83°) and (80°-86°) [16]. The restored anatomical axis in all patients can be explained by the stability conferred by the locking mechanism [17,18]; and the perfect configuration of the implant to fit the lateral face of the lateral condyle of the distal femur. LP, because of its biomechanical characteristic, promotes early mobilization, which can result in satisfactory outcomes [8].
Some authors have found good functional outcomes with greater degrees of knee flexion [10, 11]. However, modest functional results are reported [11]; and a higher complication rate [10]. Modest results in some patients may most often be due to fracture complexity, pre-existing arthritic lesions, muscle and scar adhesions, delayed rehabilitation, patient non-compliance, and postoperative complications.
5. Conclusion
Osteosynthesis of distal femoral fractures in patients with porotic bone in the elderly, using a locked plate, achieves bone union, restores the anatomical axes of the distal femur, and provides satisfactory knee function in the medium term. A study evaluating long-term data could provide further information on this subject.
References
- Zhivodernikov IV, Kirichenko TV, Markina YV, et al. Molecular and cellular mechanisms of osteoporosis. Int J Mol Sci 24 (2023): 15772.
- Porter JL, Varacallo MA. Osteoporosis. StatPearls (2023).
- Sarafrazi N, Wambogo EA, Shepherd JA. Osteoporosis or low bone mass in older adults: United States, 2017–2018. Natl Center Health Stat Data Brief 405 (2021).
- Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States. J Bone Miner Res 29 (2014): 2520-2526.
- Christianson MS, Shen W. Osteoporosis prevention and management. Clin Obstet Gynecol 56 (2013): 703-710.
- Chen Y-J, Jia L-H, Han T-H, et al. Osteoporosis treatment: current drugs and future developments. Front Pharmacol 15 (2024).
- Kennel KA, Drake MT. Adverse effects of bisphosphonates: implications for osteoporosis management. Mayo Clin Proc 84 (2009): 632-638.
- Gupta M, Gupta N. Bisphosphonate-related jaw osteonecrosis. StatPearls (2023).
- Krupa KN, Parmar M, Delo LF. Romosozumab. StatPearls (2025).
- Song J, He Y, Luo C, et al. New progress in the pharmacology of protocatechuic acid. Pharmacol Res 161 (2020): 105109.
- Jang S-A, Song HS, Kwon JE, et al. Protocatechuic acid attenuates trabecular bone loss in ovariectomized mice. Oxid Med Cell Longev (2018): 7280342.
- Qu Z, Zhao S, Zhang Y, et al. Natural compounds for bone remodeling. Biomed Pharmacother 180 (2024): 117490.
- Wu Y-X, Wu T-Y, Xu B-B, et al. Protocatechuic acid inhibits osteoclast differentiation and stimulates apoptosis. Biomed Pharmacother 82 (2016): 399-405.
- Jang SA, Song HS, Kwon JE, et al. Protocatechuic acid attenuates trabecular bone loss in ovariectomized mice. Oxid Med Cell Longev (2018): 7280342.
- Rivera-Piza A, An YJ, Kim DK, et al. Protocatechuic acid enhances osteogenesis but inhibits adipogenesis. J Med Food 20 (2017): 309-319.
- Xu G, Pei QY, Ju CG, et al. Detection on effect of different processed Cibotium barometz on osteoblasts. Zhongguo Zhong Yao Za Zhi 38 (2013): 4319-4323.
- Feng X, Feng W, Wu P, et al. Mechanism of protocatechuic acid in treating osteoporosis via HIF-1 pathway. J Funct Foods 122 (2024): 106531.
- Beaudart C, Veronese N, Douxfils J, et al. PTH1 receptor agonists for fracture risk. Osteoporos Int (2025).
- Zhu S, Chen W, Masson A, et al. Cell signaling and transcriptional regulation of osteoblast lineage commitment. Cell Discov 10 (2024).
- Zohar R, Cheifetz S, McCulloch CAG, et al. Intracellular osteopontin as a marker of osteoblastic differentiation. Eur J Oral Sci 106 (1998): 401-407.
- Mardiyantoro F, Chiba N, Seong C-H, et al. Two-sided function of osteopontin during osteoblast differentiation. J Biochem (2024).
- Sodek J, Chen J, Nagata T, et al. Regulation of osteopontin expression in osteoblasts. Ann N Y Acad Sci 760 (1995): 223-241.
- Komori T. Roles of RUNX2 in skeletal development. Adv Exp Med Biol (2017): 83-93.
- Jonason JH, Xiao G, Zhang M, et al. Post-translational regulation of RUNX2 in bone and cartilage. J Dent Res 88 (2009): 693-703.
- Artigas N, Ureña C, Rodríguez-Carballo E, et al. MAPK-regulated interactions between Osterix and Runx2. J Biol Chem 289 (2014): 27105-27117.
- Kanakaris NK, Petsatodis G, Tagil M, et al. Bone morphogenetic proteins in osteoporotic fractures. Injury 40 (2009): S21-S26.
- Manolagas SC. Wnt signaling and osteoporosis. Maturitas 78 (2014): 233-237.
- Canalis E. Wnt signalling in osteoporosis. Nat Rev Endocrinol 9 (2013): 575-583.
- Garrett IR, Chen D, Gutierrez G, et al. Proteasome inhibitors stimulate bone formation. J Clin Invest 111 (2003): 1771-1782.
- An J, Yang H, Zhang Q, et al. Natural products for treatment of osteoporosis. Life Sci 147 (2016): 46-58.
- Yang Y, Jiang Y, Qian D, et al. Prevention and treatment of osteoporosis with natural products. J Orthop Surg Res 18 (2023).



 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 