The Cost of Living Remotely: Long Distance Travel Associated with Overutilization of Chest Radiography Following Thoracic Surgery
Eleah D Porter1*, Spencer W Trooboff1, Olivia A Sacks2, Kayla A Fay1, Rian M Hasson1, 2, Timothy M Millington1, 2, David J Finley1, 2, Joseph D Phillips1, 2
1Section of Thoracic Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, USA
2Geisel School of Medicine, Hanover, USA
*Corresponding author: Eleah D Porter, Department of Surgery, Dartmouth-Hitchcock Medical Center, 1 medical Center Dr, Lebanon, NH 03756, USA
Received: 09 December 2020; Accepted: 17 December 2020; Published: 08 January 2021
Article Information
Citation: Eleah D Porter, Spencer W Trooboff, Olivia A Sacks, Kayla A Fay, Rian M Hasson, Timothy M Millington, David J Finley, Joseph D Phillips. The Cost of Living Remotely: Long Distance Travel Associated with Overutilization of Chest Radiography Following Thoracic Surgery. Archives of Clinical and Biomedical Research 5 (2021): 1-15.
View / Download Pdf Share at FacebookAbstract
Background: Healthcare overutilization is a crisis in the US. We sought to investigate if travel distance and/or other perioperative factors were associated with the ordering of unnecessary pre-discharge chest x-rays in thoracic surgery patients at a rural institution.
Methods: This was a retrospective cohort study of adults admitted after undergoing thoracic surgery with a chest tube placed at a rural, academic center. Prior to discharge, all patients underwent a standard single post-chest tube removal chest x-ray. Our primary outcome was the incidence of an unnecessary repeat (more than the standard one) chest x-ray in an asymptomatic patient. Our primary exposure was travel distance (driving distance from home zip code to hospital), dichotomized at 50 miles (short vs. long). A multivariable analysis was performed to identify if travel distance or other factors were associated with undergoing an unnecessary repeat chest x-ray.
Results: Of 241 included patients; 155 (64%) traveled long distance and 86 (36%) traveled short distance. There were no preoperative differences between patients. On multivariable analysis, long distance travel increased the odds of undergoing an unnecessary repeat chest x-ray by almost three-fold compared to short distance travel (Odds Ratio: 2.80, 95% Confidence Interval: 1.32-5.97). A patient’s rural designation, the operating surgeon, and having a postoperative complication were also independently associated with this unnecessary chest x-ray.
Conclusions: Long distance travel independently increased the odds of a thoracic surgery patient undergoing an unnecessary pre-discharge chest x-ray. Awareness of this overutilization may improve the efficiency of postoperative care pathways in rural settings.
Keywords
<p>Thoracic surgery; Chest radiography; Utilization of health services; Quality; Rurality</p>
Article Details
Abbreviations:
ASA: American Society of Anesthesiologists; CD: Clavien-Dindo; CT: Chest Tube/Tube Thoracostomy; CXR: Chest Radiograph; PFT: Pulmonary Function Test; RUCA: Rural-Urban Commuting Area Codes
1. Introduction
Healthcare overutilization is a crisis in the United States that may disproportionately affect remote environments. At our rural institution, we recently found a disparity in thoracic surgery patients in that some were more often undergoing a pre-discharge repeat chest x-ray (CXR) after chest tube (CT) removal than others [1]. Decision-making on whether to order a repeat chest film in an asymptomatic thoracic surgery patient prior to discharge may be influenced by several factors. Travel distance is a non-clinical factor that is a less well-described, but often limiting aspect of discharge planning in the rural environment [2]. To our knowledge, no study has characterized the relationship between travel distance and CXR utilization in rural thoracic surgery.
While there are reports that show limited utility of obtaining even one CXR after CT removal in an asymptomatic patient, guidelines on appropriate CXR use in thoracic surgery are lacking [1, 3-7]. Standard practice at our institution has been to obtain a single CXR after final CT removal in all thoracic surgery inpatients prior to discharge, regardless of clinical stability. An additional, or ‘repeat’, CXR is performed at the provider’s discretion. When we reviewed this practice, we found that although many of the initial CXRs had a radiographic abnormality, which may or may not have been unexpected or clinically relevant, this was inconsistently managed [1]. Some patients were kept hospitalized to undergo observation and a repeat CXR, while others were discharged with no further imaging. Considering others have found disparity in surgical care secondary to geographic barriers [2, 8-12] we wished to explore if factors such as travel distance in a rural environment were similarly biasing behavior. The goal of this study was to investigate the relationship between travel distance and other perioperative factors on the ordering of an unnecessary repeat CXR after final CT removal in asymptomatic patients following thoracic surgery at a rural center. We hypothesized that long distance travel (>50 miles) would increase the odds of undergoing this unnecessary CXR as compared to short distance travel.
2. Materials and Methods
2.1 Study design and setting
This was a retrospective cohort study of a prospectiv-
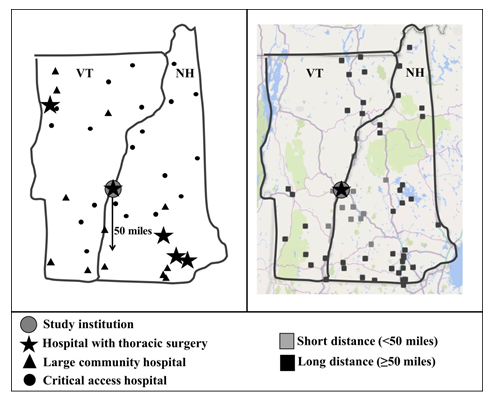
ely maintained thoracic surgery database at our 396-bed, rural, academic quaternary care hospital. The study took place between 1 July 2017 and 30 June 2018. Patient data were monitored for 30 days post discharge. This study was reviewed and approved by our Institutional Review Board with a granted waiver of consent. During the study period, it was standard practice to perform a routine single CXR after final CT removal on all patients to ensure no unexpected changes prior to discharge. This study follows the outcomes of all asymptomatic patients after this initial chest film. In these patients, an additional repeat CXR within 24 hours of final CT removal was labeled as “unnecessary” and could have indicated provider preference or concern. All CXRs were ordered by either surgical residents or advanced practice providers on the thoracic surgery team under the direction of an attending surgeon. Our primary outcome was the incidence of this unnecessary repeat (more than the standard one) CXR. Our primary exposure was travel distance, calculated by driving distance from a patient’s home zip code to the hospital using the Google Maps website, and dichotomized at 50 miles (short vs. long distance travel) based on previously published reports that define 50 miles as long distance [10, 11, 13].
2.2 Patient selection and data classification
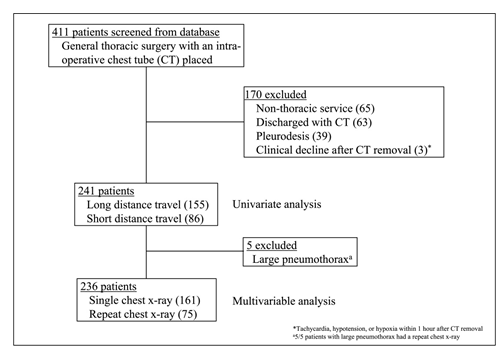
Consecutive patients who underwent thoracic surgery with an intraoperative CT placed were reviewed for eligibility. Patients were excluded if they were discharged with a CT still in place, as they would have not undergone a final CT removal CXR. Patients were also excluded if their CXR orders were not exclusively managed by the thoracic surgery service, if they experienced a clinical decline (ie; symptomatic) after CT removal that would have prompted an intervention and repeat CXR, or if they underwent pleurodesis, as this procedure necessitated a unique CXR ordering algorithm to guide clinical care (Figure 1).
Data obtained from the prospective thoracic surgery database and electronic medical record included demographics, comorbidities, American Society of Anesthesiologists (ASA) class, baseline pulmonary function tests (PFTs), procedural data, morbidity, and 30-day readmission and mortality rates. Surgical procedures were categorized into lung, pleura, mediastinum, esophagus, or diaphragm. Data pertaining to CXRs were obtained by manual chart review and included their frequency, results, and any subsequent procedural interventions secondary to those results.
Postoperative grade 3 or 4 complications as classified by Clavien-Dindo (CD) [14, 15] were monitored during the index admission (irrespective of when the final CT was removed). Grade 3 or 4 CD complications are those that require surgical, endoscopic or radiological intervention, or complications which are life threatening. Our CT management algorithm and classification of CXR results has been previously described [1].
2.3 Rural designation
In addition to travel distance, the impact of rurality on the ordering of a repeat CXR following CT removal in an asymptomatic patient was evaluated. A patient’s home zip code was categorized into mutually exclusive classifications using the Rural-Urban Commuting Area Codes (RUCA) taxonomy system [16]. We aggregated RUCA codes by the ‘Categorization B’ system, which groups zip codes into three categories: urban, large rural, and small (isolated) rural [17]. There were two patients for whom a home zip code calculated to over 1000 miles of driving distance, but upon chart review it was identified that these patients recovered from their surgery at a local hotel or residence. Therefore, the travel distance and RUCA designation for these two patients were based on the local address.
2.4 Analysis
Statistical analysis was performed using Stata/IC 15.1 (College Station, TX: StataCorp LLC). Univariate analysis was conducted using Student's t-test for continuous variables and Pearson's chi-square test or Fisher's exact test for categorical variables, as indicated by cell counts. A P -value of < .05 was considered statistically significant. Univariate analysis of travel distance (short vs. long) was performed to compare perioperative factors. Patients were also dichotomized by the primary outcome of having one vs. a repeat CXR after final CT removal. A multivariable regression model was then built to assess for factors associated with undergoing a repeat CXR after final CT removal. There were 5 patients excluded from multivariable analysis. These patients developed a large pneumothorax after final CT removal and all subsequently underwent a repeat CXR, which prevented them from being included in regression modeling. All perioperative factors with a demonstrated or theoretical association with undergoing a repeat CXR after final CT removal – long distance travel, advanced age (³ 65 years), sex, ASA class ³ 3, operating surgeon, operative approach, post-operative day of CT removal (0 vs. 1-3 vs. ³ 4), CXR result, and complications – were included in the model. Although a complication could have occurred before or after final CT removal, this was included in the model to reduce bias, as the indication for a repeat CXR could not be consistently determined from the medical record. The discriminatory power of these models was determined using the receiver operating characteristic. STROBE guidelines were used in the
writing of this manuscript [18].
3. Results
3.1 Perioperative characteristics stratified by trav- el distance
Over the 1-year study period, 241 patients were reviewed and 155 (64%) traveled long distance and 86 (36%) traveled short distance. Travel distance ranged from 2 to 443 miles, with a median distance of 59 ± 37 miles. Table 1 summarizes preoperative characteristics in short versus long distance travel patients. On univariate analysis, there were no differences between patients, including RUCA designation, mean age and proportion of those aged ³ 65 years, sex, comorbidities, PFTs, and ASA class ³ 3. Comparisons of intra- and postoperative factors are presented in Table 2. Univariate analysis revealed a significant difference between short and long distance travel patients in regard to the operating surgeon, with long distance patients being more likely to have been operated on by surgeon A or B vs. C (38.1% and 44.5% vs. 16.8% respectively, P = .014). Long distance travel patients were also significantly more likely to have undergone an unnecessary repeat CXR after final CT removal as compared to short distance travel patients (38.7% vs 23.3%, P = .015). No other differences in intraoperative factors or postoperative outcomes between short and long distance travel patients were identified. Of note, two patients died within 30 days of surgery and both were long distance travel patients. One had metastatic esophageal cancer complicated by esophageal perforation and lung abscess. The other had metastatic lung cancer with recurrent pleural effusions.
3.2 Perioperative characteristics stratified by incidence of a repeat final CT removal CXR
To investigate factors other than travel distance that may have been associated with undergoing an unnecessary repeat CXR after final CT removal, we compared pre- and perioperative characteristics between patients (Table 3). In total, 161 (67%) patients underwent a standard single CXR whereas 80 (33%) underwent an unnecessary repeat CXR. Regarding preoperative factors, patients were more likely to have an unnecessary repeat CXR based on long distance travel (P = .015), RUCA designation (P = .014), and ASA class ³ 3 (P < .001). In addition, patients in the unnecessary CXR group were more likely to have higher rates of open surgery (P < .001), surgeon A or B (P = .002), longer CT duration (P = .013), a non-normal CXR result (P = .008), a grade 3 or 4 CD complication (P = .004), and longer length of stay (P < .001). There were no differences between groups with regard to age ³ 65 years, sex, comorbidities, PFTs, procedure type, readmission rates, or mortality. Of note, no procedural interventions (eg reinsertion of a CT) were required in any patient. Other non-procedural interventions (eg diuresis, increased pulmonary toilet, transition of CT water seal system to suction, etc) were inconsistently recorded and thus unable to be tracked.
3.3 Multivariable modeling
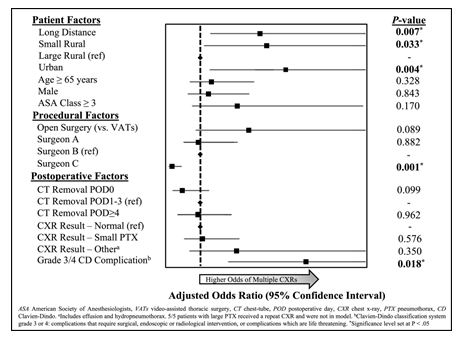
Table 4 summarizes the results of our multivariable analysis. On modeling, long distance travel significantly increased the odds of undergoing an unnecessary repeat CXR as compared to short distance travel (Odds Ratio (OR) 2.80; 95% Confidence Interval (CI) 1.32 to 5.97) (Figure 2). When assessing for rurality (RUCA designation) and its impact on having an unnecessary repeat CXR, we set large rural as reference. Adjusting for other factors, our model found that patients remained significantly more likely to undergo an unnecessary CXR if they were from a small rural location (OR 2.93; CI 1.09 to 7.87) and/or from an urban location (OR 3.25; CI 1.46 to 7.22). Figure 3 graphically depicts this finding and the geospatial relationship of patients who underwent an unnecessary repeat CXR in the context of both travel distance and access to care. Our model also revealed that having a grade 3 or 4 post-operative complication significantly increased the odds of undergoing an unnecessary CXR (OR 4.91; CI 1.31 to 18.40) while conversely, being operated on by surgeon C significantly lowered the odds (OR 0.17; CI 0.06 to 0.48). The receiver operating characteristic statistic for the model demonstrated good discrimination (0.81).
|
Short Distance (n=86) N(%) |
Long Distance (n=155) N(%) |
P value |
|
|
Age (mean ± SD) |
61 ± 17 |
61 ± 13 |
.960 |
|
Age ≥ 65 |
45 (52.3) |
68 (43.9) |
.208 |
|
Male |
46 (53.5) |
79 (51.0) |
.708 |
|
RUCA Designation |
.539 |
||
|
Small Rural |
45 (52.3) |
79 (51.0) |
|
|
Large Rural |
29 (33.7) |
46 (29.7) |
|
|
Urban |
12 (14.0) |
30 (19.4) |
|
|
Comorbidity |
|||
|
HTN |
39 (45.3) |
66 (42.6) |
.678 |
|
DM |
19 (22.1) |
29 (18.7) |
.529 |
|
Obesity |
24 (27.9) |
35 (22.6) |
.357 |
|
COPD |
19 (22.1) |
37 (23.9) |
.754 |
|
Cardiac History* |
9 (10.5) |
25 (16.1) |
.226 |
|
CKD |
3 (3.5) |
5 (3.2) |
ns. |
|
Preoperative PFTs |
|||
|
FEV1 % Predicted (median ± SD) |
74 ± 22 |
77 ± 20 |
.396 |
|
DLCO % Predicted (median ± SD) |
82 ± 22 |
83 ± 22 |
.583 |
|
ASA Class ≥ 3 |
72 (83.7) |
125 (80.6) |
.554 |
|
RUCA Rural-Urban Commuting Area Codes, HTN hypertension, DM diabetes mellitus, COPD chronic obstructive pulmonary disease, CKD chronic kidney disease, PFT pulmonary function test, FEV1 forced expiratory volume in 1 second, DLCO diffusion lung capacity for carbon monoxide, ASA American Society of Anesthesiologists |
|||
|
*Cardiac history: coronary artery disease, myocardial infarction, and congestive heart failure |
|||
Table 1: Preoperative characteristics stratified by travel distance.
|
Short Distance (n=86) N(%) |
Long Distance (n=155) N(%) |
P value |
|
|
Surgical Procedure |
.704 |
||
|
Lung |
51 (59.3) |
105 (67.7) |
|
|
Pleura |
15 (17.4) |
18 (11.6) |
|
|
Mediastinum |
13 (15.1) |
22 (14.2) |
|
|
Esophagus |
6 (7.0) |
7 (4.5) |
|
|
Diaphragm |
2 (2.3) |
2 (1.3) |
|
|
Open Surgery |
13 (15.1) |
13 (8.4) |
.107 |
|
Operating Surgeon |
.014 |
||
|
Surgeon A |
26 (30.2) |
59 (38.1) |
|
|
Surgeon B |
32 (37.2) |
69 (44.5) |
|
|
Surgeon C |
29 (33.7) |
26 (16.8) |
|
|
CT Removal Day |
.324 |
||
|
POD 0 |
14 (16.3) |
13 (8.4) |
|
|
POD 1-3 |
53 (61.6) |
99 (63.9) |
|
|
POD 4 |
20 (23.3) |
24 (15.5) |
|
|
CXR Result* |
.774 |
||
|
Normal |
40 (46.5) |
61 (39.4) |
|
|
Small PTX |
36 (41.9) |
74 (47.7) |
|
|
Large PTX |
2 (2.3) |
3 (1.9) |
|
|
Other |
9 (10.5) |
16 (10.3) |
|
|
Repeat Post-CT Removal CXR |
20 (23.3) |
60 (38.7) |
.015 |
|
Grade 3 or 4 CD Complication† |
8 (9.3) |
11 (7.1) |
.543 |
|
Need for bronchoscopy |
3 |
3 |
|
|
Required new CT |
1 |
3 |
|
|
Anastomotic stricture/breakdown |
2 |
3 |
|
|
Shock requiring pressors |
2 |
1 |
|
|
AKI requiring dialysis |
1 |
1 |
|
|
Respiratory failure |
3 |
1 |
|
|
Pneumonia requiring ICU |
1 |
2 |
|
|
Arrythmia requiring ICU/procedure |
0 |
3 |
|
|
LOS (days, median ± SD) |
2 ± 3 |
2 ± 4 |
.892 |
|
Readmission |
7 (8.1) |
14 (9.0) |
.814 |
|
Mortality |
0 (0.0) |
2 (1.3) |
.549 |
|
CT chest-tube/thoracostomy tube, POD postoperative day, CXR chest x-ray, PTX pneumothorax, CD Clavien-Dindo, AKI acute kidney injury, ICU intensive care unit, LOS length of stay |
|||
|
*Initial post-CT removal CXR †Clavien-Dindo classification system grade 3 or 4: complications that require surgical, endoscopic or radiological intervention, or complications which are life threatening. |
|||
Table 2: Intra- and postoperative characteristics stratified by travel distance.
|
Single CXR (n=161) N(%) |
Repeat CXR (n=80) N(%) |
P value |
|
|
Age (mean ± SD) |
60 ± 16 |
64 ± 12 |
.021 |
|
Age ≥ 65 |
70 (43.5) |
43 (53.8) |
.132 |
|
Male |
82 (50.9) |
43 (53.8) |
.680 |
|
Long Distance (≥ 50 miles) |
95 (60.0) |
60 (75.0) |
.015 |
|
RUCA Designation |
.014 |
||
|
Small Rural |
76 (47.2) |
48 (60.0) |
|
|
Large Rural |
60 (37.3) |
15 (18.8) |
|
|
Urban |
25 (15.5) |
17 (21.3) |
|
|
Comorbidity |
|||
|
HTN |
66 (41.0) |
39 (48.8) |
.253 |
|
DM |
28 (17.4) |
20 (25.0) |
.164 |
|
Obesity |
37 (23.0) |
22 (27.5) |
.442 |
|
COPD |
34 (21.1) |
21 (26.3) |
.371 |
|
Cardiac History* |
20 (12.4) |
14 (17.5) |
.286 |
|
CKD |
5 (3.1) |
3 (3.8) |
ns. |
|
Preoperative PFTs |
|||
|
FEV1 % Predicted (median ± SD) |
77 ± 22 |
77 ± 19 |
.815 |
|
DLCO % Predicted (median ± SD) |
83 ± 21 |
82 ± 18 |
.424 |
|
ASA Class ≥ 3 |
124 (77.0) |
76 (95.0) |
<.001 |
|
Surgical Procedure |
.182 |
||
|
Lung |
105 (65.2) |
51 (63.8) |
|
|
Pleura |
23 (14.3) |
10 (12.5) |
|
|
Mediastinum |
26 (16.1) |
9 (11.3) |
|
|
Esophagus |
5 (3.1) |
8 (10.0) |
|
|
Diaphragm |
2 (1.2) |
2 (2.5) |
|
|
Open Surgery |
9 (5.6) |
17 (21.3) |
<.001 |
|
Operating Surgeon |
.002 |
||
|
Surgeon A |
53 (32.9) |
32 (40.0) |
|
|
Surgeon B |
61 (37.9) |
40 (50.0) |
|
|
Surgeon C |
47 (29.2) |
8 (10.0) |
|
|
CT Removal Day |
|
|
.013 |
|
POD 0 |
38 (23.6) |
7 (8.8) |
|
|
POD 1-3 |
101 (62.7) |
56 (70.0) |
|
|
POD 4 |
22 (13.7) |
17 (21.3) |
|
|
CXR Result† |
.008 |
||
|
Normal |
75 (46.6) |
26 (32.5) |
|
|
Small PTX |
73 (45.3) |
37 (46.3) |
|
|
Large PTX |
0 (0.0) |
5 (6.3) |
|
|
Other |
13 (8.1) |
12 (15.0) |
|
|
Grade 3 or 4 CD Complication‡ |
7 (4.3) |
12 (15.0) |
.004 |
|
Need for bronchoscopy |
2 |
4 |
|
|
Required new CT |
1 |
3 |
|
|
Anastomotic stricture/breakdown |
2 |
3 |
|
|
Shock requiring pressors |
1 |
2 |
|
|
AKI requiring dialysis |
0 |
2 |
|
|
Respiratory failure |
2 |
2 |
|
|
Pneumonia requiring ICU |
2 |
1 |
|
|
Arrythmia requiring ICU/procedure |
0 |
3 |
|
|
LOS (days, median ± SD) |
2 ± 3 |
5 ± 4 |
<.001 |
|
Readmission |
15 (9.3) |
6 (7.5) |
.638 |
|
Mortality |
2 (1.2) |
0 (0.0) |
.549 |
|
RUCA Rural-Urban Commuting Area Codes, HTN hypertension, DM diabetes mellitus, COPD chronic obstructive pulmonary disease, CKD chronic kidney disease, PFT pulmonary function test, FEV1 forced expiratory volume in 1 second, DLCO diffusion lung capacity for carbon monoxide, ASA American Society of Anesthesiologists CT chest-tube/thoracostomy tube, POD postoperative day, CXR chest x-ray, PTX pneumothorax, CD Clavien Dindo, AKI acute kidney injury, ICU intensive care unit, LOS length of stay |
|||
|
*Cardiac history: coronary artery disease, myocardial infarction, and congestive heart failure |
|||
|
†Initial post-CT removal CXR ‡Clavien-Dindo classification system grade 3 or 4: complications that require surgical, endoscopic or radiological intervention, or complications which are life threatening. |
|||
Table 3: Perioperative characteristics stratified by single vs. a repeat post-chest tube (CT) removal chest x-ray (CXR).
|
Covariates |
Repeat CXR OR [95% CI] |
P value |
|
Patient Factors |
||
|
Long Distance |
2.80 [1.32 — 5.97] |
.007 |
|
Small Rural |
2.93 [1.09 — 7.87] |
.033 |
|
Large Rural |
reference |
|
|
Urban |
3.25 [1.46 — 7.22] |
.004 |
|
Age ≥ 65 |
1.39 [0.72 — 2.70] |
.328 |
|
Male |
1.07 [0.55 — 2.08] |
.843 |
|
ASA Class ≥ 3 |
1.99 [0.75 — 5.29] |
.170 |
|
Procedural Factors |
||
|
Open surgery (vs. VATs) |
2.47 [0.87 — 6.99] |
.089 |
|
Surgeon A |
0.95 [0.47 — 1.93] |
.882 |
|
Surgeon B |
reference |
|
|
Surgeon C |
0.17 [0.06 — 0.48] |
.001 |
|
Postoperative Factors |
||
|
CT Removal POD 0 |
0.44 [0.16 — 1.17] |
.099 |
|
CT Removal POD 1-3 |
reference |
|
|
CT Removal POD ≥ 4 |
0.98 [0.40 — 2.39] |
.962 |
|
CXR Result – Normal |
reference |
|
|
CXR Result – Small PTX |
1.22 [0.61 — 2.46] |
.576 |
|
CXR Result – Othera |
1.71 [0.56 — 5.27] |
.350 |
|
Grade 3/4 CD Complicationb |
4.91 [1.31 — 18.40] |
.018 |
|
ASA American Society of Anesthesiologists, VATs video-assisted thoracic surgery, CT chest-tube, POD postoperative day, CXR chest x-ray, PTX pneumothorax, CD Clavien-Dindo, OR odds ratio aIncludes effusion and hydropneumothorax. 5/5 patients with large PTX received a repeat CXR and were not in model. bClavien-Dindo classification system grade 3 or 4: complications that require surgical, endoscopic or radiological intervention, or complications which are life threatening. |
||
Table 4: Multivariable Analysis of Factors Associated with undergoing a repeat post-chest tube (CT) removal chest x-ray (CXR) (n=236).
Model adjusted for patient factors (travel distance, rural designation, advanced age (≥ 65 years), sex, American Society of Anesthesiologists (ASA) class ≥ 3, procedural factors (operative approach, operating surgeon), and postoperative factors (postoperative day of CT removal, CXR result from the initial post-CT removal film, and complications).
4. Discussion
In this analysis of 241 thoracic surgery inpatients at a rural center, long distance travel (>50 miles) independently increased the odds of having an unnecessary pre-discharge repeat CXR after final CT removal. This finding persisted despite adjustment for patient and peri-procedural differences. Our study highlights that in a rural setting, thoracic surgery patients who travel long distances for care may be treated differently and experience resource overutilization more often than those who reside closer to the treating institution. Previous authors have demonstrated disparity in surgical care secondary to increased travel distance, such as inappropriate workup in cancer staging, worsened cancer outcomes, and increased length of stay [2, 8-12]. However in thoracic surgery, there is a paucity of data investigating travel distance and its impact on postoperative management. We focused on a practice pattern that occurs prior to discharge - ordering of a CXR after final CT removal. Our standard practice is to order a routine single film on all patients regardless of clinical status, but many asymptomatic patients go on to have an unnecessary repeat film. This can lead to delays in discharge, increased cost and radiation exposure, and often times additional testing that ultimately does not change care.
There is no consensus on how to manage a radiographic abnormality in an otherwise asymptomatic patient after CT removal, as some findings are expected or felt to have minimal clinical significance [3-6, 19-23]. This management uncertainty may further be amplified in remote areas of the country, where patients live several hours from a hospital and are potentially isolated if an issue arises. When we asked providers why they were ordering unnecessary repeat CXRs on asymptomatic patients, they felt it may objectively demonstrate pathology in patients who could not reliably express early signs of clinical distress. While this may be true, our data showed that no procedural interventions took place after either the initial film or a repeat film. On regression modeling, there was no increased odds of getting a repeat film despite having a radiographic abnormality (other than a large pneumothorax, which for statistical reasons could not be included in the model). There were also no univariate differences in 30-day readmission or mortality between patients with a single versus a repeat CXR. Therefore, obtaining a repeat film was likely less influenced by concern for actual progression of an abnormal finding, but instead on potential concern for the impact of other factors such as travel distance. While a theoretical risk of decompensation after CT removal in asymptomatic patients exists, we question if a CXR reliably predicts this or if this risk is different for a patient traveling long versus short distance. Ultimately, our data does not support a differential CXR management strategy for asymptomatic patients after final CT removal.
In addition to long distance travel, our data revealed three other factors independently associated with undergoing an unnecessary repeat CXR after final CT removal. Rural designation (RUCA classification) and having a postoperative complication were associated with an increased likelihood, and operation by a particular surgeon decreased it. Rural designation was included in our analysis to reduce confounding, as some long distance locations were actually in urban areas. However, our data indicate that actual travel distance to our hospital may be of greater importance than an area’s population density. Other authors have similarly noted limited usefulness of the RUCA classification system in clinical study [24]. We found that patients from a small rural area had increased odds of undergoing a repeat CXR, which was expected as these areas were long distance and had limited access to care. Surprisingly, patients from urban locations also had an increased odds for an unnecessary repeat CXR. Upon closer review, we discovered that most urban locations were long distance and had limited access to specialized inpatient thoracic surgery care. If an urban patient elected to have thoracic surgery at our institution rather than locally, this likely represented a preference toward our institution.
Having a postoperative complication also increased the odds for undergoing a repeat CXR, though it is important to note the limitations of this finding in a retrospective study. All complications during an admission, irrespective of when the final CT was removed, were included in analysis. The majority of patients had their final CT removed on the day of discharge, but some had it removed several days prior. Any CXR ordered within 24 hours after final CT removal in an asymptomatic patient was classified as an unnecessary repeat x-ray, even though it may have been ordered for a reason unrelated to the CT removal process and during a workup for an unrelated concern (eg new-onset arrhythmia, development of pneumonia, etc). We were unable to reliably determine indications for a CXR and often the indication listed was ‘post-thoracic surgery, evaluate for change’. Therefore, this finding may represent anxiety towards patients who had already experienced a complication prior to final CT removal, biasing providers to order an unnecessary repeat CXR in an effort to avoid another complication. Alternatively, this may represent a limitation of retrospective study design, which ultimately justifies its inclusion in the model to adjust for differences in complication rates that are likely independent of other risk factors such as travel distance and rural designation. Only one factor decreased the odds of undergoing an unnecessary repeat CXR, operation by a particular surgeon. CXR orders were managed by the same team of thoracic surgery providers (surgical residents and advanced practice providers) who covered all of the surgeons. Therefore, differences seen based on the operating surgeon may indicate surgeon specific preferences. However, determining surgeon preference by retrospective review is challenging. To address this, future studies will assess provider intent when ordering a repeat CXR.
Our findings should be viewed in the context of several limitations. This is a single center, retrospective review in a rural location. Our results may not be generalizable to a broader patient population or urban setting. RUCA codes were used to classify rurality, which has been shown to have limited utility in medical research [24]. We were not able to capture qualitative factors involved in the decision making between a patient and clinician. Additionally, we were unable to reliably determine why a repeat CXR was ordered or if a postoperative complication warranted a CXR during its workup in the monitored 24 hour period, potentially over-estimating the influence of our modeled factors on behavior. Despite these limitations, a previously unreported non-clinical factor of long distance travel was found to be independently associated with higher utilization of CXRs on post-thoracic surgery inpatients at a rural institution. Healthcare efficiency and appropriate utilization of resources is becoming increasingly important. Unrecognized bias may lead to disparity in care and create barriers to discharge that prolong hospitalization. In the rural environment, long travel distance is a prominent factor that impacts decision-making and discharge planning in thoracic surgery patients. Awareness of these types of biases can lead to the development of more evidence-based care and increased efficiency of healthcare delivery. Based on our findings we have taken steps to critically evaluate our postoperative pathways to decrease unnecessary CXRs.
5. Conclusion
Long distance travel is an independent factor that is associated with overutilization of pre-discharge CXRs in thoracic surgery inpatients at a rural institution. In a remote setting, patients who travel long distances for care may be treated differently than those who reside closer. Awareness of this potential bias may improve the efficiency of postoperative care pathways, decreasing cost and radiation exposure at rural institutions.
References
- Porter ED, Fay KA, Hasson RC, Millington TM, Finley DJ, Phillips JD. Routine Chest X-Rays After Thoracic Surgery Are Unnecessary. J Surg Res 250 (2020): 188-192.
- Katharine L Jackson, Robert E Glasgow, Britani R Hill, Mary C Mone, Bradford Sklow, Courtney L Scaife, et al. Does travel distance influence length of stay in elective colorectal surgery?. Dis Colon Rectum 56 (2013): 367-373.
- McGrath E, Ranstrom L, Lajoie D, McGlynn L, Mooney D. Is a Chest Radiograph Required After Removal of Chest Tubes in Children?. J Pediatr Heal Care 31 (2017): 588-593.
- Daniel G French, Michael Dilena, Simon LaPlante, Farid Shamji, Sudhir Sundaresan, James Villeneuve, et al. Optimizing postoperative care protocols in thoracic surgery: Best evidence and new technology. J Thorac Dis 8 (2016): S3-S11.
- Whitehouse M, Patel A, Morgan J. The necessity of routine post thoracostomy tube chest radiographs in post-operative thoracic surgery patients. Surgeon 7 (2009): 79-81.
- Alessandro Brunelli, Egidio Beretta, Stephen D Cassivi, Robert J Cerfolio, Frank Detterbeck, Thomas Kiefer, et al. Consensus definitions to promote an evidence-based approach to management of the pleural space. A collaborative proposal by ESTS, AATS, STS, and GTSC. Eur J Cardiothorac Surg 40 (2011): 291-297.
- Medbery RL, Fernandez FG, Khullar O V. ERAS and patient reported outcomes in thoracic surgery: a review of current data. J Thorac Dis 11 (2019): S976-S986.
- Kathleen M Fairfield, Adam W Black, F Lee Lucas, Kimberly Murray, Erika Ziller, Neil Korsen, et al. Association Between Rurality and Lung Cancer Treatment Characteristics and Timeliness. J Rural Heal (2019).
- Wasif N, Chang Y-H, Pockaj BA, Gray RJ, Mathur A, Etzioni D. Association of Distance Traveled for Surgery with Short- and Long-Term Cancer Outcomes. Ann Surg Oncol 23 (2016): 3444-3452.
- Nader N Massarweh, Yi-Ju Chiang, Yan Xing, George J Chang, Alex B Haynes, Nancy You Y, et al. Association between travel distance and metastatic disease at diagnosis among patients with colon cancer. J Clin Oncol 32 (2014): 942-948.
- Kang R, Columbo JA, Trooboff SW, Servos MM, Goodney PP, Wong SL. Receipt of sentinel lymph node biopsy for thin melanoma is associated with distance traveled for care. J Surg Oncol 119 (2019): 148-155.
- Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L. Distance as a Barrier to Cancer Diagnosis and Treatment: Review of the Literature. Oncologist 20 (2015): 1378-1385.
- Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer 112 (2008): 909-918.
- Pierre A Clavien, Jeffrey Barkun, Michelle L de Oliveira, Jean Nicolas Vauthey, Daniel Dindo, Richard D Schulick, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250 (2009): 187-196.
- Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240 (2004): 205-213.
- University of Washington. Rural-Urban Commuting Area Codes (RUCAs). Rural Health Research Center (2019).
- University of Washington. Using RUCA data. Rural Health Research Center (2019).
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg 12 (2014): 1495-1499.
- Whitehouse M, Patel A, Morgan J. The Necessity of Routine Post Thoracostomy Tube Chest Radiographs in Post-Operative Thoracic Surgery Patients. Surgeon 7 (2009): 79-81.
- Graham R J, Meziane M A, Rice T W, Agasthian T, Christie N, Gaebelein K, et al. Postoperative portable chest radiographs: optimum use in thoracic surgery. J Thorac Cardiovasc Surg 115 (1998): 45-50.
- Bjerregaard LS, Jensen K, Petersen RH, Hansen HJ. Routinely obtained chest X-rays after elective videoassisted thoracoscopic surgery can be omitted in most patients; a retrospective, observational study. Gen Thorac Cardiovasc Surg 63 (2015): 465-471.
- Knudsen MR, Nyboe C, Hjortdal VE, Pilegaard HK. Routine postoperative chest X-ray is unnecessary following the Nuss procedure for pectus excavatum. Interact Cardiovasc Thorac Surg 16 (2013): 830-833.
- Leschber G, May CJ, Simbrey-Chryselius N. Do thoracic surgery patients always need a postoperative chest X-ray? Zentralbl Chir 139 (2014): S43-S49.
- Onega T, Weiss JE, Alford-Teaster J, Goodrich M, Eliassen MS, Kim SJ. Concordance of Rural-Urban Self-identity and ZIP Code-Derived Rural-Urban Commuting Area (RUCA) Designation. J Rural Health (2019).


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 