Understanding Pediatric Cholelithiasis: A Clinical Review
Dr. Maria Rogalidou, MD, PhD*
Division of Gastroenterology & Hepatology, First Department of Paediatrics National and Kapodistrian University of Athens 'Aghia Sophia' Children's Hospitall, Athens, Greece
*Corresponding author: Dr. Maria Rogalidou, Division of Gastroenterology & Hepatology, First Department of Paediatrics National and Kapodistrian University of Athens 'Aghia Sophia' Children's Hospitall, Athens, Greece.
Received: 17 September 2025; Accepted: 23 September 2025; Published: 13 October 2025
Article Information
Citation: Maria Rogalidou, Understanding Pediatric Cholelithiasis: A Clinical Review. Archives of Clinical and Biomedical Research. 9 (2025): 396-402.
View / Download Pdf Share at FacebookAbstract
Cholelithiasis is a common gastrointestinal disorder in adults but remains relatively uncommon in children and adolescents. However, advances in diagnostic imaging—particularly ultrasonography—have led to increased detection rates in pediatric populations. While the condition occurs with similar frequency in both sexes during early childhood, a higher prevalence in females is observed after puberty.
Beyond hemolytic disorders, the underlying pathophysiology of gallstone and biliary sludge formation in children is not fully understood. Gallstone formation is associated with hemolytic diseases, hepatobiliary disorders, ileal diseases, previous abdominal surgeries, malabsorption syndromes, cystic fibrosis, obesity, certain medications, family history of gallstones, and, in many cases, idiopathic origins.
Pediatric cholelithiasis may be asymptomatic or present with non-specific gastrointestinal symptoms. When symptomatic, clinical manifestations are typically related to complications such as cholecystitis, cholangitis, common bile duct obstruction, and pancreatitis, presenting with abdominal pain, fever, jaundice, and vomiting.
There is no established indication for pharmacologic treatment in asymptomatic cases; Ursodeoxycholic acid may be beneficial in select patients, but complete gallstone resolution is rare, and recurrence after discontinuation is common. Symptomatic cholelithiasis generally warrants surgical intervention, with laparoscopic cholecystectomy being the preferred approach. Notably, prophylactic laparoscopic cholecystectomy is recommended in asymptomatic patients with sickle cell anemia due to their increased risk of complications. Surgical management may also be considered for other patients with long-standing asymptomatic cholelithiasis.
Conclusion: Although pediatric cholelithiasis remains relatively rare, its recognition is increasing. A comprehensive approach—including risk factor assessment, imaging, and individualized treatment—is essential for effective management and prevention of complications.
Keywords
<p>Cholelithiasis in children and adolescents; Gallbladder; Cholecystitis; Cholecystectomy</p>
Article Details
1. Introduction
Cholelithiasis is rare in childhood, although in recent years there has been an increase in its incidence in children, this can partly be attributed to the increased diagnostic capacity with the use of imaging methods, especially ultrasound [1]. The first description of cholelithiasis in a child was made by Gibson in 1734, while the first systematic discovery was made by Potter in 1928 [2]. Despite the rarity of the condition in infancy and childhood, cholelithiasis has also been described during intrauterine life as well as in newborns [3]. Many studies reported that the disease in children can be symptomatic or asymptomatic (17-50%) and the prognosis for simple cholelithiasis is good [4-8]. It is estimated that the average time between the discovery of asymptomatic cholelithiasis and the development of symptoms is over ten years.
2. Definitions
Cholelithiasis: Presence of gallstones (accumulations of solid material) in the biliary system, usually in the gallbladder.
Biliary sludge: It is formed from deposits of cholesterol crystals and calcium salts which are embedded in the mucus of the bile ducts.
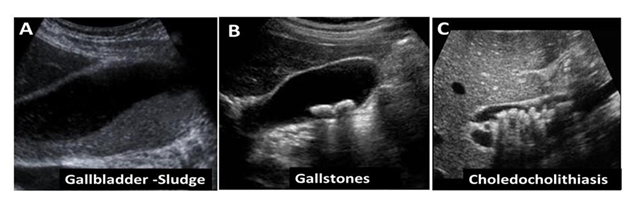
Choledocholithiasis: presence of one or more gallstones in the common bile duct. Ultrasound Images of cholelithiasis appears in Figure 1
3. Epidemiology
The incidence of cholelithiasis depends on age, sex, race, genetic and geographic factors as it is reported in many studies [9-12]. Epidemiological studies suggest that genetic factors may be involved in the occurrence of cholelithiasis and individuals with the ABCB4 mutation are more likely to develop cholelithiasis [11]. The incidence of cholelithiasis and biliary sludge in children varies and ranges from 1.9% and 1.46% respectively [4]. Children younger than 26 months of age constitute 10% of all cases of cholelithiasis in childhood. Cholelithiasis occurs with equal frequency in both sexes in early childhood, while after puberty it appears to be more common in girls. In a study of 305 children with sickle cell disease, the 19.7% had gallstones and 16.4% had biliary sludge, and also that the incidence of gallstones increases with age and is associated with higher serum bilirubin levels [13]. Biliary sludge can be a precursor to gallstones, with 65.7% of children with sludge developing gallstones on follow-up. Underlying diseases such as hemolytic diseases, history of parenteral nutrition, Wilson's disease, cystic fibrosis, and medication usually coexist, while after puberty some studies reported that other factors are also involved such as obesity, with its dramatic increase in recent years in children, and pregnancy [10,11]. The reported incidence of fetal gallstones is approximately 0.45%, typically appearing around 34.7 weeks of gestation (range: 22–38 weeks) [3]. Predisposing factors for fetal cholelithiasis include both maternal and fetal conditions. Maternal factors associated with prenatal gallstone formation include type 1 diabetes mellitus, sepsis, and exposure to certain medications such as ceftriaxone, furosemide, and prostaglandin E2. Fetal risk factors include Rh or ABO incompatibility, trisomy 21, oligohydramnios, and intrauterine growth restriction (IUGR) [3,7,12].
4. Pathophysiology
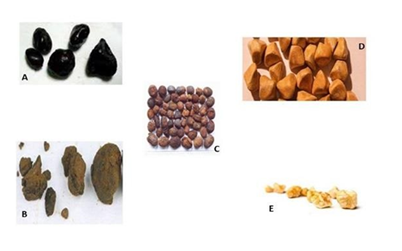
The five main components of bile are water, bilirubin, cholesterol, bile pigments, and phospholipids. The initial process for the formation of gallstones begins with the precipitation of the insoluble primary components of bile, mainly cholesterol, bile pigments, and calcium salts as it is reported in a number of studies [10,14]. An imbalance in bile components such as cholesterol, lecithin, and bile salts leads to the formation of gallstones, as an increase in cholesterol also increases the rate of its crystallization and creates favorable conditions for their formation. Gallstones can be black, cholesterol (yellow), calcium carbonate, protein, and brownish (Figure 2).
Usually one type of stone occurs at a given time. Black gallstones constitute 48% of stones in children and are formed when the composition of the bile is supersaturated with calcium bilirubinate and calcium salts of indirect bilirubin. Black stones usually occur in chronic hemolytic diseases and after parenteral nutrition. Stringer et al. [15] reported that calcium carbonate stones, which are rare in adults, occur more frequently in children and constitute 24% of gallstones in childhood and are the only ones that can be seen on plain abdominal radiography [1]. Cholesterol gallstones develop when bile becomes supersaturated with cholesterol due to an imbalance—typically excess cholesterol and decreased bile salts or phospholipids—leading to cholesterol precipitation and stone formation. Cholesterol stones are the most common stones in adults but account for about 21% of gallstones in children [16]. Coffee stones are rare, comprising approximately 3% of gallstones in children. They typically form due to bile stasis and infection within the bile ducts. These stones are composed of calcium bilirubinate, calcium salts, and fatty acids, and are more commonly located within the biliary tree rather than the gallbladder. Protein stones account for about 5% of pediatric gallstones. Microlithiasis refers to the presence of gallstones measuring less than 3 mm in diameter. These stones form within the intrahepatic or extrahepatic bile ducts, may cause biliary colic, cholecystitis, or pancreatitis, and can persist even after cholecystectomy [17].
5. Etiology
Cholelithiasis in children can be due to a variety of causes related to predisposing factors as shown in table 1 but can also be idiopathic. A number of studies reported that he incidence of cholelithiasis in children with sickle cell anemia is almost twice that of the general population while hemolytic diseases appear to be responsible for 20-40% of all cholelithiasis in children [18,19]. A fairly common cause of biliary sludge, mainly but also cholelithiasis, is the administration of ceftriaxone, which in most cases is transient and known by the term "pseudolithiasis" [20]. In recent years, a number of studies reported that there has been an increase in the incidence of cholelithiasis in childhood, which can be partly attributed to the widespread use of ultrasound [14,15], but also to the increase in childhood obesity [21-23].
Current research has highlighted genetic factors contributing to cholelithiasis in children. The (TA)7/(TA)7 promoter genotype of the UGT1A1 gene has been associated with an increased risk of gallstone formation in otherwise healthy children [24]. Family history plays a significant role, with children from families with cholelithiasis having 24.7 times higher odds of developing the condition [25]. The genetic predisposition, along with environmental factors, influences the pathogenesis of cholelithiasis in pediatric populations [26]. In children with sickle cell anemia, specific polymorphisms in genes involved in bilirubin metabolism, such as UGT1A1, SLCO1A2, and SLCO1B1, have been linked to an increased risk of gallstone formation [27]. Understanding these genetic factors can lead to earlier diagnosis and more effective management of cholelithiasis in children.
6. Clinical Presentation
In most cases, patients are asymptomatic and the diagnosis is made during imaging for another reason. However, cholelithiasis can present mainly with acute or chronic abdominal pain in the right hypochondrium, dyspeptic complaints and nausea. In the initial differential diagnosis for acute abdominal pain localized to the right hypochondrium, we should also consider other conditions such as cholecystitis, pancreatitis, retrocaecal appendicitis, while for chronic abdominal pain, duodenal ulcer, bile duct cyst, and gallbladder dyskinesia. When complications of the disease occur, other symptoms may coexist such as jaundice, nausea, vomiting, fever, and a positive Murphy sign. Also, depending on the underlying disease, there may be corresponding symptoms.
7. Laboratory Testing: Investigation
It is important for pediatric patients to also investigate the existence of underlying diseases that are associated with the occurrence of cholelithiasis in childhood as mentioned in the etiology. The predisposing factors of cholelithiasis in children appears in Table 1.
|
Conditions |
Diseases |
|
Hemolytic diseases |
Sickle cell anemia, thalassemias, hereditary spherocytosis, G6PD deficiency, pyruvate kinase deficiency, autoimmune hemolytic anemia |
|
Abdominal surgeries |
Ileal removal |
|
Short bowel |
|
|
Liver and biliary diseases |
Chronic liver disease, cirrhosis, gallbladder cyst |
|
Bowel diseases |
Crohn's disease, Ulcerative Colitis, Celiac disease, malabsorption syndromes, |
|
Metabolic diseases |
Wilson's disease, bile salt metabolism disorders |
|
Genetic diseases |
Progressive familial intrahepatic cholestasis (PFIC), Cystic fibrosis |
|
Down syndrome |
|
|
Gilbert's disease |
|
|
Disorders related to the body Weight |
Obesity, sudden weight loss, prolonged fasting |
|
Low calorie diet |
|
|
Parenteral nutrition |
Table 1: Predisposing Factors for Cholelithiasis in children.
In symptomatic disease, depending on the clinical picture and symptoms, an initial laboratory test should be sent in order to investigate the existence of cholestasis or inflammation. Specifically: Complete blood count, ESR, CRP, transaminases, γGT, alkaline phosphatase, total and direct bilirubin, amylase, lipase & urine examination. In simple cholelithiasis, all tests should be normal, however, finding abnormal values may indicate obstruction, inflammation, or both. The diagnosis of the disease is made using ultrasound (Figure 2), an examination with high sensitivity and specificity for its detection, but also capable of giving us other information about possible complications, e.g. cholecystitis, pancreatitis. Other imaging tests such as plain radiography, scintigraphy, and cholangiopancreatography may help in the overall approach or provide complementary information. Plain radiography has no overall role in the detection of cholelithiasis with the exception of calcium carbonate stones, however it can be helpful in the case of ileus from gallstones or the detection of free air sub-diaphragmatically. Scintigraphy after the use of cholecystokinin or a fatty meal may be a useful test for demonstrating gallbladder filling and bile excretion, especially when gallbladder dyskinesia is suspected. In children with complicated cholelithiasis, additional investigation of the anatomy of the biliary tree with magnetic resonance cholangiopancreatography (MRCP) should be performed or endoscopic retrograde cholangiopancreatography (ERCP) which can also be therapeutic by decongesting the bile ducts in case of bile duct stones [28]. ERCP in pediatric patients has similar success and complication rates as in adults, however, ERCP in children should be performed in specialized centers with extensive experience [29].
8. Complications of Gallstone Disease
Choledocholithiasis, Bile duct obstruction, Cholecystitis, Cholangitis, Pancreatitis, Hepatitis, Ileus from gallstone
9. Management
In contrast to adults, for whom clear guidelines for the treatment of cholelithiasis exist, there is no standardized approach to managing pediatric cholelithiasis at the national or international level— likely due to a lack of evidence-based studies [30]. In symptomatic patients, laparoscopic cholecystectomy is recommended, which is a safe and effective procedure in children with a low rate of postoperative complications. In acute cholecystitis, monitoring for 1-2 weeks is recommended (stones may pass) [31]. In cases of complications, immediate cholecystectomy is recommended. In asymptomatic patients, initial testing to exclude underlying causes is recommended, followed by regular clinical and ultrasound monitoring14. In infants, spontaneous dissolution of gallstones is most often observed [14]. Surgical intervention is not recommended in asymptomatic pediatric patients with cholelithiasis. An exception is patients with sickle cell anemia and asymptomatic cholelithiasis for whom laparoscopic cholecystectomy is recommended early in order to avoid any complications of cholelithiasis that occur more frequently in these patients [31-33]. Laparoscopic cholecystectomy is also a treatment option in older children with asymptomatic cholelithiasis who have received several years of follow-up without regression of the gallstones [16]. A recent systematic review and meta-analysis of pediatric cases undergoing laparoscopic cholecystectomy (LC), showed that LC is a safe and well-tolerated procedure in children, with complication rates comparable to those reported in adult populations. The most common indications for LC in the pediatric group were cholelithiasis, cholecystitis, and biliary dyskinesia [34].
Conservative treatment of cholelithiasis can be done with the administration of ursodeoxycholic acid, which appears to be associated with clinical improvement; Pediatric patients were administered ursodeoxycholic acid at a dose of 25 mg/kg/day over a median duration of thirteen months [5]. The treatment led to the resolution of clinical symptoms in 83.7% of patients. However, complete dissolution of gallstones was achieved in only 7.2% of cases, and recurrence occurred in 50% of those who initially responded. Notably, all participants completed the course of therapy without experiencing any adverse effects. However, a recent study suggested that Ursodeoxycholic acid (UDCA) should not be used routinely in the pediatric population, particularly in infants. Its use may be considered in symptomatic children who have contraindications to surgery or when there is a need to alleviate clinical symptoms [35]. Ursodeoxycholic acid (UDCA) may be considered in children undergoing rapid weight loss (e.g., post-bariatric surgery or very low-calorie diets) to prevent gallstones; its use in such pediatric contexts mirrors adult protocols in populations at increased risk for developing or relapsing cholelithiasis still is recommended [26,36].
10. Lifestyle Modifications in Pediatric Cholelithiasis
Lifestyle interventions play a crucial role in the prevention and management of cholelithiasis in children:
- Dietary Modifications: It is recommended to reduce the consumption of fatty foods and to manage body weight, particularly in cases of obesity. This approach has been associated with a decreased risk of gallstone formation in both children and adults [17,21,26]
- Physical Activity: Increased physical activity has been shown to lower the incidence of cholelithiasis, particularly in adults, and is encouraged in children as part of a healthy lifestyle
- Avoidance of Rapid Weight Loss: Rapid weight loss, especially with very low-calorie diets (<800 kcal/day), increases the risk of gallstone formation and should be avoided in children, as in adults [26,36].
- Healthy Eating Patterns: Regular meals and a diet rich in fiber, calcium, and vitamin C, water—while limiting fatty, sugary, and fast foods—can help reduce bile lithogenicity and promote efficient gallbladder emptying [26].
- • Nutritional Support in Parenteral Nutrition (PN): In patients requiring PN, simultaneous enteral feeding is recommended whenever feasible, as it reduces biliary stasis and the risk of gallstone development. The use of modified lipid emulsions (e.g., SMOF lipids containing soy oil, medium-chain triglycerides, olive oil, and fish oil) instead of pure soy-based lipid emulsions may further decrease gallstone formation and has been associated with stone resolution in some cases [26].
- • Medication Review: The use of certain medications—such as estrogens, oral contraceptives, ceftriaxone, octreotide, and cyclosporine—may increase bile Avoidance or cautious use of these agents is advisable in children at risk for cholelithiasis.
11. Choledocholithiasis
The incidence of gallstone disease, and hence complications like choledocholithiasis (common bile duct stones, CBD stones), has been increasing in children [37]. In pediatric cholelithiasis cases, choledocholithiasis appears among the more frequent complications, along with cholecystitis and pancreatitis. In one study of 135 children having surgery for gallstones, ~64.4 % had complications; choledocholithiasis was among the common ones [38].
Several recent studies have aimed to define risk factors or build prediction tools to identify which children with gallstones are likely to have choledocholithiasis.
Risk score has been developed by a study (from 2010-2019 data) to reduce non-therapeutic ERCPs. Variables included: acute biliary pancreatitis, ascending cholangitis, elevated liver enzymes, bilirubin ≥2 mg/dL, US findings (dilated CBD, stone seen). High risk was ≥2 factors or ascending cholangitis; very high risk if 3 risk factors or ascending cholangitis. This allows better prediction [37].
In another study developed the Pediatric DUCT Score from a cohort of ~979 children undergoing cholecystectomy, ~22.7 % had confirmed CBD stones as shown by MRCP / ERCP / IOC [39].
They identified three independent predictive factors:
a. Common bile duct dilation ≥ 6 mm on ultrasound
b. Ultrasound showing choledocholithiasis
c. Total bilirubin ≥ 1.8 mg/dL
Risk stratification via number of these factors yields “low”, “intermediate”, “high”, “very high” risk; the model had specificity >78%, accuracy >76%, NPV >79%.
Prediction model using machine learning / multivariate logistic regression on ~316 pediatric patients: key variables: ALT, total bilirubin, ALP, and CBD diameter by ultrasound. They set a threshold to get ≥90% specificity to avoid unnecessary ERCPs. The model had ~71.5% accuracy, PPV ~71.4%, NPV ~72.1% [40].
12. Diagnostic Approach for Choledocholithiasis
Ultrasound remains a first-line imaging tool, particularly to look for CBD dilation, visualization of stones, etc. It is included in all the prediction tools.
When suspicion is high (per risk scores/models), use of MRCP (magnetic resonance cholangiopancreatography), intraoperative cholangiography (IOC), or ERCP to confirm presence of stones.
The predictive tools are designed to reduce non-therapeutic ERCPs, i.e. avoid ERCP in children unlikely to have stones (since ERCP carries risks).
13. Treatment / Management of Choledocholithiasis
Options include:
- • ERCP for stone removal. Risks include complications (pancreatitis, infection, etc.). Used when diagnostic/imaging confirmation indicates stone
- • Laparoscopic common bile duct exploration (LCBDE or CBDE) – surgical removal during cholecystectomy or as stand-alone procedure. Some recent evidence supports doing a “surgery-first” approach in children in some settings. For example, a multi-institutional study comparing pediatric vs adult patients found LCBDE is highly successful in children and with no increased surgical complications compared to adults [41]
- • Combined approaches: sometimes ERCP first (if endoscope access possible etc.), sometimes intraoperative exploration. The choice may depend on resources, surgical/endoscopic expertise, risk to patient, size of stone(s), dilation, etc
14. Outcomes and Recommendations
Children who have higher risk (per the models) benefit by going directly to diagnostic or therapeutic modalities rather than waiting for delayed/chronic symptoms. Early identification helps reduce morbidity [37].
In the pediatric DUCT study, the risk stratification allows clinicians to select children who are very likely to have CBD stones, improving specificity and avoiding some unnecessary procedures [39].
The multi-institutional study (2018-2024) shows that in children, surgery (LCBDE) has at least as good clearance rates as adults, and complications are similar; also in children, when endoscopy first is attempted the complication rates may be higher. This suggests favoring surgery in institutions where that is feasible [41].
Choledocholithiasis is an increasingly recognized complication of pediatric gallstone disease, often presenting alongside pancreatitis or cholecystitis. Accurate risk stratification is essential to guide diagnosis and management while minimizing unnecessary procedures. Recent predictive models, such as the Pediatric DUCT Score, offer reliable tools based on ultrasound findings and laboratory markers to assess the likelihood of common bile duct stones. These tools support a targeted diagnostic approach—reserving MRCP, IOC, or ERCP for high-risk cases—thereby reducing the use of non-therapeutic ERCP, which carries procedural risks. Treatment options include ERCP and laparoscopic common bile duct exploration (LCBDE), with growing evidence favoring a surgery-first approach in children, especially in centers with surgical expertise.
15. Conclusion
Cholelithiasis in children and adolescents, although less common than in adults, has shown a rising incidence in recent years, largely due to improved diagnostic capabilities and the increasing prevalence of pediatric obesity. Although the condition is often asymptomatic and typically follows a benign course, screening for potential underlying diseases is essential. While symptomatic presentations and complications such as cholecystitis and pancreatitis necessitate timely diagnosis and appropriate management. Understanding the diverse etiological factors— including genetic predispositions, underlying systemic conditions, and lifestyle influences—is essential for individualized treatment. Conservative management with ursodeoxycholic acid may offer symptom relief in selected patients, although its efficacy in stone dissolution is limited. Laparoscopic cholecystectomy remains the definitive treatment for symptomatic cases and is also indicated in specific asymptomatic populations, such as patients with sickle cell anemia. A multidisciplinary approach that includes imaging, laboratory evaluation, and consideration of underlying conditions is crucial to optimize outcomes in pediatric cholelithiasis. Timely identification and stratified management of choledocholithiasis improve outcomes and reduce morbidity in pediatric patients.
Article Summary: This is a review article that gives a short review for Cholelithiasis in children & adolescents, targeting to give an update for pediatricians.
Contributors Statement Page: Dr Maria Rogalidou, MD, PhD, Consultant pediatric Gastroenterologist, conceptualized and designed the study, drafted the initial manuscript, and critically reviewed and revised the manuscript.
Acknowledgments: None
Conflict of Interest Disclosures (includes financial disclosures): The author have no conflict of interest to declare.
Funding/Support: No funding was secured for this study.
References
- El-Karaksy H, El-Matary W, El-Sayed H, et al. Gallstones in Egyptian infants and children: risk factors, complications and outcome: a single center experience. Egypt Liver J 10 (2020): 1.
- Biliary Lithiasis in Children. In: Biliary Lithiasis. Springer (2011): 401-408.
- Schwab ME, Braun HJ, Feldstein VA, et al. The natural history of fetal gallstones: a case series and updated literature review. J Matern Fetal Neonatal Med 35 (2022): 4755-4762.
- Wesdorp I, Bosman D, de Graaff A, et al. Clinical presentations and predisposing factors of cholelithiasis and sludge in children. J Pediatr Gastroenterol Nutr 31 (2000): 411-417.
- Della Corte C, Falchetti D, Nebbia G, et al. Management of cholelithiasis in Italian children: a national multicenter study. World J Gastroenterol 14 (2008): 1383-1388.
- Poddar U. Gallstone disease in children. Indian Pediatr 47 (2010): 945-953.
- Debray D, Franchi-Abella S, Irtan S, et al. Cholelithiasis in infants, children and adolescents. Presse Med (2012).
- Bogue CO, Murphy AJ, Gerstle JT, et al. Risk factors, complications, and outcomes of gallstones in children: a single-center review. J Pediatr Gastroenterol Nutr 50 (2010): 303-308.
- Wyllie R, Hyams JS, Kay M. Pediatric gastrointestinal and liver disease. 5th ed. Philadelphia (PA): Elsevier (2016).
- Portincasa P, Moschetta A, Berardino M, et al. Impaired gallbladder motility and delayed orocecal transit contribute to pigment gallstone and biliary sludge formation in beta-thalassemia major adults. World J Gastroenterol 10 (2004): 2383-2390.
- Vegunta RK, Raso M, Pollock J, et al. Biliary dyskinesia: the most common indication for cholecystectomy in children. Surgery 138 (2005): 726-731.
- Goldman DA. Gallbladder, gallstones, and diseases of the gallbladder in children. Pediatrics Rev 41 (2020): 623.
- Al-Salem AH, Qaisruddin S. The significance of biliary sludge in children with sickle cell disease. Pediatr Surg Int 13 (1998): 14-16.
- Karami H, Kianifar HR, Karami S. Cholelithiasis in children: a diagnostic and therapeutic approach. J Pediatr Rev 5 (2017): 45-50.
- Stringer MD, Soloway RD, Taylor DR, et al. Calcium carbonate gallstones in children. J Pediatr Surg 42 (2007): 1677-1682.
- Kennedy M, Cuffari C. Pediatric gallstones (cholelithiasis). Medscape (2021).
- Bonfrate L, Wang DQ, Garruti G, et al. Obesity and the risk and prognosis of gallstone disease and pancreatitis. Best Pract Res Clin Gastroenterol 28 (2014): 623-635.
- Alonso MH. Gall bladder abnormalities in children with sickle cell disease: management with laparoscopic cholecystectomy. J Pediatr 145 (2004): 580-581.
- Curro G, Meo A, Ippolito D, et al. Asymptomatic cholelithiasis in children with sickle cell disease: early or delayed cholecystectomy? Ann Surg 245 (2007): 126-129.
- Prince JS, Senac MO. Ceftriaxone-associated nephrolithiasis and pseudolithiasis in a child. Pediatr Radiol 33 (2003): 648-651.
- Kaechele V, Wabitsch M, Thiere D, et al. Prevalence of gallbladder disease in obese children and adolescents: influence of the degree of obesity, sex, and pubertal development. J Pediatr Gastroenterol Nutr 42 (2006): 66-70.
- Krawczyk M, Kułaga Z, Niewiadomska O, et al. Are children with gallstone disease more overweight? Results of a matched case-control analysis. Clin Res Hepatol Gastroenterol 47 (2023): 102204.
- Mehta S, Lopez ME, Chumpitazi BP, et al. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 129 (2012): e82-e88.
- Kitsiou-Tzeli S, Kanavakis E, Tzetis M, et al. Gilbert's syndrome as a predisposing factor for idiopathic cholelithiasis in children. Haematologica 88 (2003): 1193-1194.
- Shutova OV, Bahatska N. Genealogical characteristics of children and adolescents with cholelithiasis and their families. Zaporozhye Med J (2018).
- Zdanowicz K, Daniluk J, Lebensztejn DM, et al. The etiology of cholelithiasis in children and adolescents: a literature review. Int J Mol Sci 23 (2022): 13376.
- Chaouch L, Kalai M, Darragi I, et al. Genetic link with cholelithiasis among pediatric SCA Tunisian patients: examples of UGT1A1, SLCO1A2 and SLCO1B1. Hematology (2015).
- Dalton SJ, Balupuri S, Guest J. Routine magnetic resonance cholangiopancreatography and intraoperative cholangiogram in the evaluation of common bile duct stone. Ann R Coll Surg Engl 87 (2005): 469-470.
- Rocca R, Castellino F, Daperno M, et al. Therapeutic ERCP in pediatric patients. Dig Liver Dis 37 (2005): 357-362.
- Diez S, Müller H, Weiss C, et al. Cholelithiasis and cholecystitis in children and adolescents: does this increasing diagnosis require a common guideline for pediatricians and pediatric surgeons? BMC Gastroenterol 21 (2021): 186.
- Al-Salem AH, Issa H. Laparoscopic cholecystectomy in children with sickle cell anemia and the role of ERCP. Surg Laparosc Endosc Percutan Tech 22 (2012): 139-142.
- Al Hindi S, Al Aradi H, Mubarak M. Laparoscopic cholecystectomy in children with sickle cell disease: a simple modified technique. Asian J Endosc Surg 13 (2020): 514-518.
- Siddiqui S, Newbrough S, Alterman D, et al. Efficacy of laparoscopic cholecystectomy in the pediatric population. J Pediatr Surg 43 (2008): 109-113.
- Mattson A, Sinha A, Njere I, et al. Laparoscopic cholecystectomy in children: a systematic review and meta-analysis. Surgeon 21 (2023): e133-e141.
- Çakar S, Eren G, Erdur CB, et al. Cholelithiasis in infants: risk factors, management, and the role of ursodeoxycholic acid. Children (Basel) 11 (2024): 1553.
- Orłowska A, Socha P, Szychta M, et al. Management of gallstone disease in children. Pediatr Pol 98 (2023): 229-235.
- Capparelli MA, Alessandro PD, Questa HA, et al. Development of a risk score for choledocholithiasis in pediatric patients. Pediatr Surg Int 37 (2021): 1393-1399.
- Chamorro C, Arteaga P, Paredes C, et al. Cholelithiasis and associated complications in pediatric patients. Cir Pediatr 33 (2020): 172-176.
- Ignacio RC, Kelley-Quon LI, Ourshalimian S, et al. Pediatric DUCT Score: a highly specific predictive model for choledocholithiasis in children. J Am Coll Surg 236 (2023): 961-970.
- Cohen RZ, Tian H, Sauer CG, et al. Creation of a pediatric choledocholithiasis prediction model. J Pediatr Gastroenterol Nutr 73 (2021): 636-641.
- Dantes G, Rauh JL, Smith S, et al. Multi-institutional analysis of choledocholithiasis in pediatric vs adult patients. J Pediatr Surg 59 (2024): 161661.


 Impact Factor: * 5.8
Impact Factor: * 5.8 Acceptance Rate: 71.20%
Acceptance Rate: 71.20%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 