Validation of the Spanish Version of the Forgotten Joint Score in Total Hip Arthroplasty
Sebastian Carvajal1,6*, Julian Brañes2,6, Joaquín Domínguez3, Guillermo Elias2, Angel Bravo1, Sebastián León2, Rodrigo Olivares1,6, Alex Kremer1, Maximiliano Barahona4, Rodrigo Wulf2,4,6, Alvaro Martinez2,6, Cristian Barrientos1,4,5
1Orthopaedic Department at Hospital del Salvador, Santiago, Chile
2Orthopaedic Department at Hospital Clinico San José, Santiago, Chile
3Orthopaedic Department at Hospital San Borja Arrarian, Santiago, Chile
4Orthopaedic Department at Hospital Clinico Universidad de Chile, Santiago, Chile
5Orthopaedic Department at Clinica Santa María, Santiago, Chile
6Orthopaedic Department at Clinica Bupa Santiago, Santiago, Chile
*Corresponding Author: Sebastián Carvajal Fuentes, Orthopaedic Department at Hospital Salvador, Santiago, Chile.
Received: 16 July 2025; Accepted: 23 July 2025; Published: 30 July 2025
Article Information
Citation: Sebastian Carvajal, Julian Brañes, Joaquín Domínguez, Guillermo Elias, Maximiliano Barahona, Rodrigo Wulf, Cristian Barrientos. Validation of the Spanish Version of the Forgotten Joint Score in Total Hip Arthroplasty. Journal of Orthopedics and Sports Medicine. 7 (2025): 366-372.
View / Download Pdf Share at FacebookAbstract
Objective: To translate, culturally adapt, and validate the Forgotten Joint Score (FJS) into Spanish for use in patients who have undergone total hip arthroplasty (THA).
Methods: The FJS was translated and culturally adapted following international guidelines. A cross-sectional validation study was conducted in two Chilean institutions. Patients who underwent THA for primary osteoarthritis between 2018 and 2019 were recruited. The Spanish FJS and the validated Spanish version of the Oxford Hip Score (OHS) were administered to assess reliability and validity. Internal consistency was measured using Cronbach’s alpha. Test-retest reliability was assessed using the intraclass correlation coefficient (ICC), Lin’s concordance correlation coefficient (CCC), and the Bradley-Blackwood test. Construct validity was evaluated through Spearman’s correlation with the OHS.
Results: A total of 241 patients completed the first round, and 184 completed the second round. The Spanish FJS showed excellent internal consistency (Cronbach’s alpha = 0.967 and 0.977 for the first and second rounds, respectively). Test-retest reliability was strong (ICC = 0.84; CCC = 0.84), with no significant difference between rounds (p = 0.52). Construct validity was supported by a moderate negative correlation with the OHS (rho = -0.64 and -0.65 for rounds one and two, respectively). Ceiling and floor effects were low across both instruments.
Conclusion: The Spanish version of the FJS is a valid and reliable patientreported outcome measure for assessing satisfaction and joint awareness following THA. Its inclusion in clinical practice and national registries is strongly recommended for Spanish-speaking populations.
Keywords
<p>Joint replacement surgery; Forgotten joint score; Total hip arthroplasty; Spanish-speaking patients; Cronbach's alpha</p>
Article Details
1. Introduction
The primary goal of joint replacement surgery is to alleviate pain, restore functionality, and ultimately improve the quality of life [1]. With advancements in surgical techniques and implant quality, there has been a notable improvement in implant survival rates over the past few decades. Consequently, patient expectations regarding surgical outcomes have increased, along with life expectancy. Surgical outcomes have traditionally been assessed through radiology and clinical evaluations, which are often outdated and not directly comparable [2]. However, the use of specific, modern questionnaires in recent years has enabled the comparison and accurate interpretation of results in this new era [3].
Patient-reported outcome measures (PROMs) are questionnaires completed by patients to assess the results of their intervention. These allow for the comparison and quantification of changes during follow-up. Currently, PROMs are the gold standard for comparing clinical outcomes, as they focus on the patient's perspective rather than the treating physician's opinion [4].
PROMs included in national registries must be culturally adapted and validated, as results may vary due to different cultural interpretations [5].
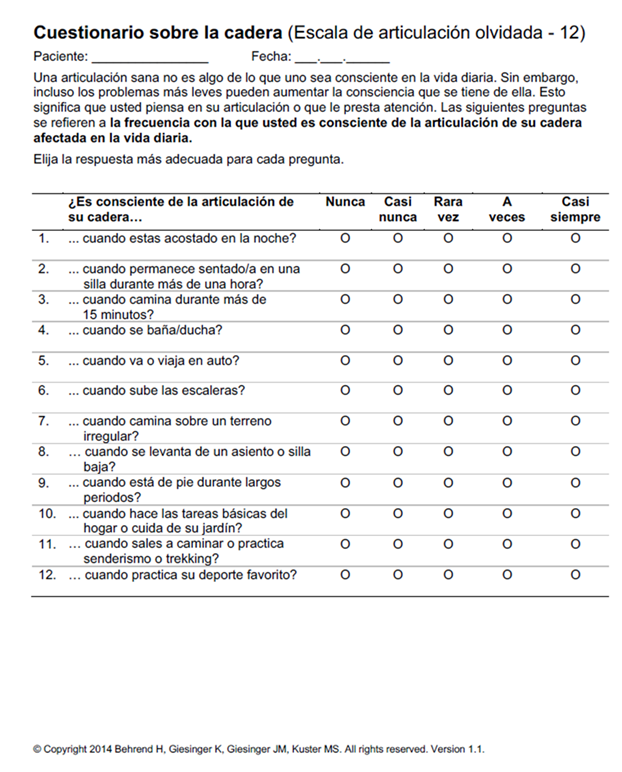
The Forgotten Joint Score (FJS) was introduced in 2012 as a novel concept to assess whether patients can forget about their recent total hip arthroplasty (THA) surgery during daily activities. According to the authors, this is the ultimate goal of patient satisfaction [6,7]. This 12-item score (raw score range 0–100) was designed to enhance the ability to distinguish between good and excellent results, reducing the ceiling and floor effects. Various studies and reviews have demonstrated that the FJS has good construct validity, test-retest reliability, and strong discriminatory power, making it particularly useful for patients with a high level of function and active use of their hip arthroplasty [8-10].
To our knowledge, the FJS has not been validated in Spanish, and we believe its use could be highly beneficial for evaluating Spanish-speaking patients. This is particularly important considering the large Spanish-speaking population undergoing joint replacement surgery [11].
The main objective of this study is to translate, culturally adapt, and validate the Spanish version of the Forgotten Joint Score for patients who have undergone total hip arthroplasty [12].
2. Methods
This study was approved by our institutional ethics review board, and informed consent was obtained from all patients prior to their participation.
The original Forgotten Joint Score (FJS) was translated into Spanish, culturally adapted, and its psychometric properties were evaluated. The translation and adaptation process adhered to established guidelines, under the supervision and approval of the Chief Translation and Licensing Officer for the Forgotten Joint Score, who validated the Spanish version and provided the scoring instructions (Translation and Licensing Officer Forgotten Joint Scores, www.forgotten-joint-score.pro) [13,14].
The translation process began with a forward translation of the FJS into Spanish, performed by two native Spanish-speaking translators fluent in English. This was followed by a back-translation into English by two native English-speaking translators fluent in Spanish. A consensus meeting was then held, involving three experts in total hip arthroplasty (THA), the four translators, and two medical students. The original English version was compared with the back-translated version to ensure consistency and identify discrepancies. Any clinical or linguistic issues in the Spanish version were addressed during this session. The final Spanish version was subsequently pilot-tested with 30 randomly selected patients who had previously undergone THA to assess its comprehensibility [15].
A cross-sectional study design was used to collect data from two institutions that employed the same uncemented prosthesis and surgical team. Patients were included if they were 18 years or older and had undergone hip replacement due to primary osteoarthritis between January 1, 2018, and December 31, 2019. All procedures involved a posterior hip approach and a non-constrained primary prosthesis (Corail® uncemented hip stem, Pinnacle® uncemented cup; DePuy Synthes, Warsaw, IN). Patients were excluded if they had hip fractures, required revision surgeries, experienced infections, had bilateral hip replacements, or presented with language barriers or cognitive impairments [16,17].
From an initial pool of 520 eligible patients, medical records were reviewed to extract sociodemographic and clinical data, including sex, age, surgery date, surgical protocol, phone number, and email address. A total of 300 patients met the selection criteria, and efforts to contact them began in June 2020, ensuring a minimum follow-up period of one year post-THA. Of these, 241 patients provided informed consent (digitally or verbally) and completed the FJS and the Oxford Hip Score (OHS). The OHS, a widely used and validated tool in Spanish, served as the reference instrument [18]. It consists of 12 items assessing functional outcomes, with scores ranging from 12 to 60, where lower scores indicate better outcomes. Patients were asked to complete the OHS again 14 days after the initial response. A total of 184 patients returned the second round of responses.
The Forgotten Joint Score (FJS-12) uses a 5-point Likert scale and consists of 12 equally weighted items that evaluate the awareness of the artificial joint during daily activities. Responses range from "Never" (0) to "Mostly" (4), and the total raw score ranges from 0 (worst condition) to 100 (best condition). The FJS is recognized for its high test-retest reliability, low ceiling effect, and strong construct validity for hip and knee arthroplasty. An additional question regarding awareness of the hip during sexual activity was included in the Spanish version but was not factored into the final scoring.
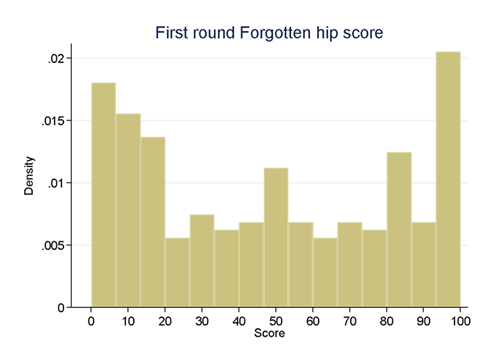
Categorical variables were summarized as absolute and percentage frequencies, while continuous variables were expressed as medians, ranges, and interquartile ranges (IQR). Histograms were generated to illustrate the distribution of scores. Internal consistency was evaluated using Cronbach's alpha, with a coefficient greater than 0.75 indicating acceptable reliability. Factor analysis was conducted, retaining factors with eigenvalues greater than 1. The ceiling effect was calculated as the percentage of patients achieving the maximum score, and the floor effect reflected the percentage obtaining the minimum score.
Test-retest reliability was assessed by comparing scores from the initial and follow-up responses. Intraclass correlation coefficients (ICC), Lin’s concordance correlation coefficients (CCC), and the Bradley-Blackwood F-test were used to evaluate reliability. ICC and CCC values above 0.75 were considered acceptable, while a p-value greater than 0.15 in the Bradley-Blackwood F-test confirmed concordance between the two sets of responses.
Spearman’s correlation coefficient (rho) was calculated between the OHS and the Spanish-adapted FJS to assess construct validity. A rho value greater than 0.6 was interpreted as indicative of good correlation.
3. Results
In the first round, 241 patients completed the FJS. The median age was 66 years (range, 23–89; IQR, 58–73), and 152 patients (63.07%) were female. The median FJS was 48 (range, 0–100; IQR, 15–81) (Figure 1).
In the second round, 184 patients responded. The median age was 66 years (range, 23–87; IQR, 56–73), and 124 (67.4%) were female. The median FJS was 62 (range, 0–100; IQR, 13–86).
Cronbach’s alpha indicated excellent internal consistency, with coefficients of 0.9667 (first round) and 0.9769 (second round). Factor analysis identified a single factor with an eigenvalue of 9.24, explaining 72% of the variance. This factor was strongly correlated with items 1 to 11 but less so with items 12 and 13 (Table 1).
Test-retest reliability was robust: ICC = 0.84 (95% CI, 0.79–0.88), CCC = 0.84 (95% CI, 0.79–0.89), and the Bradley-Blackwood test returned a p-value of 0.52, confirming concordance.
Spearman’s correlation demonstrated moderate alignment between the OHS and the Spanish-adapted FJS. In the first round, rho = -0.64 (p < 0.0000), and in the second round, rho = -0.6519 (p < 0.0000) (Table 2).
|
First round |
Second round |
|||||
|
Forgotten hip score |
N |
MEDIAN |
IQR |
N |
MEDIAN |
IQR |
|
Q1 |
241 |
2(0 a 4) |
0 a 4 |
184 |
1(0 a 4) |
0 a 3 |
|
Q2 |
241 |
2(0 a 4) |
0 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q3 |
241 |
2(0 a 4) |
0 a 4 |
184 |
1(0 a 4) |
0 a 4 |
|
Q4 |
241 |
2(0 a 4) |
0 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q5 |
241 |
2(0 a 4) |
0 a 4 |
184 |
1(0 a 4) |
0 a 4 |
|
Q6 |
241 |
2(0 a 4) |
1 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q7 |
241 |
3(0 a 4) |
1 a 4 |
184 |
2(0 a 4) |
1 a 4 |
|
Q8 |
241 |
2(0 a 4) |
1 a 4 |
184 |
1(0 a 4) |
0 a 4 |
|
Q9 |
241 |
2(0 a 4) |
1 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q10 |
241 |
2(0 a 4) |
1 a 4 |
184 |
2(0 a 4) |
1 a 4 |
|
Q11 |
241 |
2(0 a 4) |
1 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q12 |
241 |
2(0 a 4) |
0 a 4 |
184 |
2(0 a 4) |
0 a 4 |
|
Q13 |
203 |
0(0 a 4) |
0 a 2 |
150 |
1(0 a 4) |
0 a 2 |
|
Alpha |
13 |
0.9667 |
13 |
0.9769 |
||
Abbreviation: Q=Question; N=Number; IQR= Interquartile range
Table 1: Summarise every question of the Spanish adaptation of Forgotten joint score in both rounds.
|
Characteristic |
S-A Forgotten Hip score |
OHS |
|
|
ROUND 1 |
N |
241 |
241 |
|
Median (range) |
48 (0 to 100) |
7 (0 to 44) |
|
|
IQR |
15 to 81 |
2. to 19 |
|
|
Ceiling effect |
5.8% |
12.4% |
|
|
Floor effect |
7.1% |
0% |
|
|
ROUND 2 |
N |
184 |
184 |
|
Median (range) |
62 (0 to 100) |
8 (0 to 41) |
|
|
IQR |
13 to 86 |
3. to 16 |
|
|
Ceiling effect |
7.1% |
14.1% |
|
|
Floor effect |
4.9% |
0% |
Abbreviation: S-A=Spanish-adapted; OHS= Oxford hip score; IQRr= interquartile range
Table 2: Summary of satisfaction scores from the Spanish adaptation of the Forgotten Joint Score and the Oxford Hip Scale in rounds 1 and 2.
Figure 1: histogram of the score distribution of the forgotten hip score in the first round.
4. Discussion
This study provides a validated and culturally adapted Spanish version of the Forgotten Joint Score (FJS) for patients undergoing total hip arthroplasty (THA). The instrument demonstrated excellent internal consistency, high test-retest reliability, and acceptable construct validity, supporting its use among Spanish-speaking populations.
Before employing a PROM, a rigorous process of translation and cultural adaptation is essential to ensure its relevance across different populations [19]. Our work adheres to this principle and contributes a new tool for Spanish speakers, addressing a previously unmet need.
PROMs have become central to evaluating surgical outcomes, shifting the focus from clinician-based assessments to the patient’s lived experience [20,21]. The FJS, in particular, stands out due to its ability to capture subtle differences in patient satisfaction, especially among those who achieve excellent clinical results. Its low ceiling and floor effects enhance its discriminatory power, making it superior in this regard compared to other PROMs [22].
Recent research suggests that PROMs should be interpreted cautiously and strictly within the scope for which they were developed [23-25]. Moreover, as Gagnier et al. [2] emphasize, no single PROM can capture all dimensions of outcome, which highlights the value of having multiple validated tools. Our study expands this toolkit, especially since existing Spanish PROMs have not adequately assessed the dimension of "joint awareness" or satisfaction in a culturally sensitive way.
One of the strengths of the FJS is its practicality: it is free to use and easily administered via paper, phone, or email. Additionally, the concept of “forgetting” the joint replacement — the basis of the FJS — reflects an advanced stage of recovery. This notion has become increasingly relevant, as patients today expect more than pain relief; they aspire to return to an unrestricted lifestyle.
Originally developed by Behrend et al. [8], the FJS has been translated into multiple languages and applied beyond hip and knee arthroplasty, owing to its conceptual appeal. We found no major issues during the translation and cross-cultural adaptation process, supporting its transferability to other Spanish-speaking regions. Given the large and growing population of Spanish speakers worldwide [11], we believe this version will be a valuable addition to the available PROMs.
Despite promising validation results, our average FJS scores (48 and 62 in the first and second rounds, respectively) were lower than the threshold of 73.96 suggested by Rosinsky et al. [26] to define a successful outcome at one year postoperatively. Several cultural factors may explain this discrepancy. In Chile, and possibly in other Latin American contexts, “forgetting” a surgery may be interpreted negatively, both by patients and surgeons. Patients are often reminded of their joint replacement during follow-ups, and are consistently educated about postoperative care. Consequently, constant awareness of the prosthesis may not reflect dissatisfaction or poor outcomes, but rather a cultural emphasis on vigilance.
Patient participation was high in the first round (80.3%) and slightly lower in the second (63.7%), which may reflect digital illiteracy in part of the population [27]. Nevertheless, test-retest reliability remained strong. Although our average FJS score was lower than those in other studies, our Oxford Hip Score (OHS) results confirmed good clinical outcomes, supporting the construct validity of the Spanish FJS.
While the correlation between FJS and OHS was moderate (rho ≈ -0.65), this was expected, as the two instruments measure different constructs. The OHS primarily evaluates pain and function, whereas the FJS focuses on awareness and satisfaction. Yeo et al. [28] have also questioned the suitability of the OHS for assessing satisfaction, reinforcing our rationale for introducing the FJS [29,31].
An additional question (n° 13) regarding sexual activity was included based on patient interest (as reported by Nunley et al. [32]) but was excluded from the final score to maintain comparability with the original instrument [6]. Nevertheless, its inclusion highlighted an important area of concern that may warrant further exploration in future PROM development.
This study has limitations. The COVID-19 pandemic limited face-to-face evaluations, and many patients had limited digital literacy, affecting response rates. Clinical outcomes such as range of motion were not assessed, though this aligns with the methodology of the original FJS validation. Lastly, follow-up was limited to a minimum of one year; although this is consistent with validation studies, longer-term data would be valuable for further research.
5. Conclusion
The Spanish-adapted version of the Forgotten Joint Score (FJS) is a reliable, valid, and culturally appropriate instrument for evaluating outcomes after total hip arthroplasty in Spanish-speaking populations. It demonstrated excellent internal consistency, high test-retest reliability, and acceptable construct validity when compared with an established instrument. Unlike traditional measures that focus solely on pain or function, the FJS offers a more nuanced view of patient satisfaction and joint awareness. Its ease of use and relevance to modern patient expectations make it a valuable addition to the set of available PROMs. We recommend its inclusion in clinical practice and joint replacement registries across Spanish-speaking countries.
References
- Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet 370 (2007): 1508-19.
- Gagnier JJ, Huang H, Mullins M, et al. Measurement properties of patient-reported outcome measures used in patients undergoing total hip arthroplasty: a systematic review. JBJS Rev 6 (2018): e2.
- Longo UG, Ciuffreda M, Candela V, et al. Hip scores: A current concept review. Br Med Bull 131 (2019): 81-96.
- Vega JF, Spindler KP. Types of scoring instruments available. In: Musahl V, Karlsson J, Hirschmann MT, Ayeni OR, Marx RG, Koh JL, et al., editors. Basic Methods Handbook for Clinical Orthopaedic Research. Berlin, Heidelberg: Springer (2019).
- Siljander MP, McQuivey KS, Fahs AM, et al. Current trends in patient-reported outcome measures in total joint arthroplasty: a study of 4 major orthopaedic journals. J Arthroplasty 33 (2018): 3416-21.
- Behrend H, Giesinger K, Giesinger JM, et al. The "forgotten joint" as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27 (2012): 430-6.e1.
- Kang S. Assessing responsiveness of the EQ-5D-3L, the Oxford Hip Score, and the Oxford Knee Score in the NHS patient-reported outcome measures [published correction appears in J Orthop Surg Res 16 (2021): 115.
- Adriani M, Malahias MA, Gu A, et al. Determining the validity, reliability, and utility of the Forgotten Joint Score: A systematic review. J Arthroplasty 35 (2020): 1137-44.
- Thompson SM, Salmon LJ, Webb JM, et al. Construct validity and test-retest reliability of the Forgotten Joint Score. J Arthroplasty 30 (2015): 1902-5.
- Singh V, Bieganowski T, Huang S, et al. The Forgotten Joint Score patient-acceptable symptom state following primary total hip arthroplasty. Bone Jt Open 3 (2022): 307-13.
- Barahona M, Barrientos C, Martinez Á, et al. Mortality after hip or knee arthroplasty for osteoarthritis in Chile: A survival analysis. Medwave (2020).
- Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol 63 (2010): 737-45.
- Martín-Fernández J, Gray-Laymón P, Molina-Siguero A, et al. Cross-cultural adaptation and validation of the Spanish version of the Oxford Hip Score in patients with hip osteoarthritis. BMC Musculoskelet Disord 18 (2017): 205.
- Sánchez R, Echeverry J. Validación de escalas de medición en salud [Validating scales used for measuring factors in medicine]. Rev Salud Publica (Bogota) 6 (2004): 302-18.
- Wang D, Jones MH, Khair MM, et al. Patient-reported outcome measures for the knee. J Knee Surg 23 (2010): 137-51.
- Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics 45 (1989): 255-68.
- Zar JH. Spearman rank correlation. In: Encyclopedia of Biostatistics. John Wiley & Sons, Ltd; 2005. Online ISBN: 9780470011812.
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1 (1986): 307-10.
- Arias-de la Torre J, Puigdomenech E, Valderas JM, et al. Availability of specific tools to assess patient reported outcomes in hip arthroplasty in Spain. Identifying the best candidates to incorporate in an arthroplasty register. A systematic review and standardised assessment. PLoS One 14 (2019): e0214746.
- Brook EM, Glerum KM, Higgins LD, et al. Implementing patient-reported outcome measures in your practice: pearls and pitfalls. Am J Orthop (Belle Mead NJ) 46 (2017): 273-8.
- Hamilton DF, Giesinger JM, Giesinger K. It is merely subjective opinion that patient-reported outcome measures are not objective tools. Bone Joint Res 6 (2017): 665-6.
- Rolfson O, Bohm E, Franklin P, et al. Patient-reported outcome measures in arthroplasty registries. Acta Orthop 87 (2016).
- Fidai MS, Saltzman BM, Meta F, et al. Patient-reported outcomes measurement information system and legacy patient-reported outcome measures in the field of orthopaedics: a systematic review. Arthroscopy 34 (2018): 605-14.
- Kahlenberg CA, Nwachukwu BU, McLawhorn AS, et al. Patient satisfaction after total knee replacement: a systematic review. HSS J 14 (2018): 192-201.
- Pivec R, Johnson AJ, Mears SC, et al. Hip arthroplasty. Lancet 380 (2012): 1768-77.
- Rosinsky PJ, Chen JW, Lall AC, et al. Can we help patients forget their joint? Determining a threshold for successful outcome for the Forgotten Joint Score. J Arthroplasty 35 (2020): 153-9.
- Education at a Glance 2017: OECD Indicators. OECD Publishing, Paris (2017).
- Yeo MGH, Goh GS, Chen JY, et al. Are Oxford Hip score and Western Ontario and McMaster Universities Osteoarthritis index useful predictors of clinical meaningful improvement and satisfaction after total hip arthroplasty? J Arthroplasty 35 (2020): 2458-64.
- Kalairajah Y, Azurza K, Hulme C, et al. Health outcome measures in the evaluation of total hip arthroplasties—a comparison between the Harris hip score and the Oxford hip score. J Arthroplasty 20 (2005): 1037-41.
- Martín-Fernández J, Gray-Laymón P, Molina-Siguero A, et al. Cross-cultural adaptation and validation of the Spanish version of the Oxford Hip Score in patients with hip osteoarthritis. BMC Musculoskelet Disord 18 (2017): 205.
- Issa K, Pierce TP, Brothers A, et al. Sexual activity after total hip arthroplasty: a systematic review of the outcomes. J Arthroplasty 32 (2017): 336-40.
- Nunley RM, Nam D, Bashyal RK, et al. The impact of total joint arthroplasty on sexual function in young, active patients. J Arthroplasty 30 (2015): 335-40.}
Supplementary File:
“Appendix A: Spanish version of the Forgotten Joint Score”


 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 73.64%
Acceptance Rate: 73.64%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 