Addressing Challenges and Exploring Prospects in Childhood Cancer Care in Cameroon
Andreas Frambo*, 1, Berthe Sabine Esson Mapoko2, 9, Valirie Ndip Agbor3, Joseph Nkfusai4, Sophie De Chazal5, Nyemb Mbog Grace10, Armelle Kamdem10, Glenn M. Afungchwi6, 7, Francine Tchintseme7, Emily Kobayashi5, Ousmane Diaby11, Angelle Hermine Pondy2, 10, Paul Ndom2, 9, Yauba Saidu1, 8
1Clinton Health Access Initiative, Yaoundé, Cameroon
2Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon
3Nuffield Department of Population Health, University of Oxford, Oxford, UK
4Faculty of Health Sciences, University of Buea, Cameroon
5Clinton Health Access Initiative, Boston, USA.
6Faculty of Health Sciences, The University of Bamenda, Cameroon
7Mbingo Baptist Hospital, Bamenda Cameroon
8Institute for Global Health, University of Siena, Siena, Italy
9National Committee for the Fight Against Cancer, Yaoundé Cameroon
10Mother and Child Center, Chantal Biya Foundation, Yaoundé Cameroon.
11Faculty of Economics and Management Sciences, University of Ngaoundere, Cameroon.
*Corresponding author: Andreas Frambo, Senior Program Manager, Non-Communicable Diseases and Essential Medicines Clinton Health Access Initiative Yaoundé, Cameroon.
Received: 06 January 2024; Accepted: 16 January 2024; Published: 05 March 2024
Article Information
Citation: Andreas Frambo, Berthe Sabine Esson Mapoko, Valirie Ndip Agbor, Joseph Nkfusai, Sophie De Chazal, Nyemb Mbog Grace, Armelle Kamdem, Glenn M. Afungchwi, Francine Tchintseme, Emily Kobayashi, Ousmane Diaby, Angelle Hermine Pondy, Paul Ndom, Yauba Saidu. Addressing Challenges and Exploring Prospects in Childhood Cancer Care in Cameroon. Fortune Journal of Health Sciences. 7 (2024): 105-111.
View / Download Pdf Share at FacebookAbstract
Background: Childhood cancers is the sixth cause of global cancer burden. Indeed, 90% of these cases occur in low- middle-income countries (LMICs), where mortality can be 4-5 folds higher compared to high income settings. In addition, many LMICs lack pediatric oncology data for policy and resource prioritization. In this paper, we describe the state of pediatric cancer care and treatment in Cameroon.
Procedure: We conducted cross-sectional survey in July 2020, enabling data collection from the two hospitals providing pediatric oncology services including treatment type, human resource, disease type, diagnostic capacity, treatment dropout, disclosure, and data management.
Result: Both surveyed hospitals offered pediatric chemotherapy and palliative care services. However, neither offered nuclear medicine nor radiotherapy services. Human resources were grossly insufficient in both hospitals with one pediatric hemato-oncologist, one medical oncologist, one resident pediatric oncologist, one pediatric surgeon, and 14 oncology nurses. About 40% (18/45) of staff had received formal oncology training. In both settings, there was limited capacity for case finding, diagnosis and counselling. Burkitt’s lymphoma, (39, 23%) was the main childhood cancer type. Nearly 30% of eligible patients for chemotherapy, did not receive their treatment. Amongst those who received, 19% dropped out, mainly due to lack of funds to continue treatment sessions. Data collection and transmission tools varied per facility with no defined schedule for data reporting.
Conclusions: Several factors negatively impact optimal pediatric cancer care and treatment in Cameroon. We identified inadequate human resource capacity, limited case finding and diagnostic capacity, significant treatment dropout rates due to high treatment costs, and lack of harmonized data systems. Taking a systematic approach to addressing these health system components, especially through the development and implementation of a pediatric cancer national strategy has the potential to enhance case finding and treatment outcomes of pediatric cancer patients in Cameroon.
Keywords
<p>pediatric cancer, treatment access, data management, Cameroon</p>
Article Details
1. Introduction
Survival from childhood cancers has improved tremendously over the last five decades [1]. Indeed, about 80% of childhood cancers can be successfully treated in high-income settings with good access to modern treatments and supportive care. Unfortunately, about 90% of children at risk of childhood cancer each year reside in developing countries, with limited availability and accessibility to technical platforms for early diagnosis and management of childhood cancers [2-5]. Since children depend on their parents or carers, their symptoms might be overlooked, leading to delayed diagnosis, misdiagnosis, and late treatment initiation, eventually leading to poor patient outcomes [6]. In addition, children are often neglected in cancer control programs, partly because of a paucity of data on childhood cancer risk and survival [7]. In 2019, pediatric cancers represented the sixth leading cause of the global burden of cancers and the ninth leading cause of global childhood disease burden [1]. Despite representing only 1% of global cancer cases diagnosed yearly, childhood cancers are associated with disproportionately high disability-adjusted life-years (DALYs) because children have a longer life expectancy. For instance, over 80% of the 11.5 million DALYs attributed to childhood cancers in 2019 occurred in LMICs [1]. In Cameroon, childhood cancers account for 1 to 2% of all cancers, and malignant hemopathies like acute lymphoid leukemia (ALL) and acute myeloid leukemia (AML) represent about 50% of childhood cancer cases. Although 90% of these cancers are curable, over 80% of patients seek care at an advanced stage of the disease, leading to high mortality rates of up to 40% [8]. For example, data from the Yaoundé population-based cancer registry estimates an incidence of childhood cancers of 125/1,000,000 children, with approximately 1552 incident cases of childhood cancers expected to occur annually [9]. Despite this incidence level, in 2018, the pediatric oncology unit of the Mother and Child Centre of the Chantal Biya Foundation [MCC/CBF] (The Reference Pediatric Hospital located in Yaoundé, Cameroon) recorded only 150 new cases of childhood cancer, representing below 10% of the expected number, which is likely an underestimation of the true value.
Data on the management of childhood cancers in Cameroon are warranted for policy implementation and prioritization of expenditures. Therefore, this study sought to investigate the key obstacles to optimal pediatric cancer care in the two functional oncology services in Cameroon. Specifically, we aimed to describe pediatric cancer service availability, human resource capacity involved in pediatric cancer care, treatment completion, patient education and disclosure as well as data management system for pediatric cancers.
2. Methods
This cross-sectional descriptive study was conducted in July 2020 in Cameroon. Cameroon is a bilingual and multicultural Central African country, with about 28 million inhabitants in 2022 across the countries 10 administrative regions [10]. The country’s healthcare system has a pyramidal structure, organized into three levels: i) the peripheral (operational) level, which is at the base of the pyramid. It consists of an extensive network of district hospitals (DH), sub-divisional hospitals (CMA) and Integrated Health Centers (IHC), which are spread across the country’s 10 regions [11].; ii) the intermediate level, which consists primarily of regional hospitals (RH) and Regional Hospital Centres (RHC), whose technical platforms are higher than that for district hospitals; iii) the central level, which is at the top of the pyramid. It consists of specialized reference hospitals, including General Hospitals (GH) and Central Hospitals (CH) as well as well as administrative structures that are responsible for developing, regulating, and coordinating health strategies. Figure 1 shows the distribution of these facilities across the countries 10 regions. Of the nearly 6,000 facilities in the country, just two hospitals provide oncology services for pediatric patients. These include the Mother and Child Centre of the Chantal Biya Foundation (MCC/CBF) located in Yaoundé in the capital City and the Mbingo Baptist Hospital (MBH), located in the Northwest region, about 360 km from the capital city of Bamenda. The MCC/CBF is a state-owned referral and teaching hospital and research center and offers mainly chemotherapy and palliative care for the management of childhood cancers while The MBH is a faith-based referral hospital and a teaching center, which offers chemotherapy, surgery and palliative care services for both childhood and adult cancers patients.
2.1 Study procedure and data collection
The questionnaire we used for the study was developed by adapting questions from different questionnaires including, the Impact Assessment for improving outcomes of cancer strategies developed by the government of the United Kingdom. The adapted questionnaire was jointly reviewed and validated in stakeholder meeting at the national committee for the fight against cancer prior to data collection. The final questionnaire and pilot testing had sections to collect information on pediatric cancer service availability (chemotherapy, radiotherapy, nuclear medicine), human resource capacity, case finding and diagnosis, chemotherapy treatment completion, patient education and disclosure of status as well as data management. Following administrative authorization from Cameroon’s Ministry of Health (MOH), we deployed trained data collectors to the MCC/CBF, who used the approved questionnaire to collect the required data; however, due to security risks in the North-West Region, these data collectors could not visit the MBH. As a result, we sent a copy of the tool to two of the co- authors of this paper (GMA and FT) electronically, who in turned leveraged it to collect the necessary data. To understand reasons for drop-out, families identified as loss to follow-up were contact traced through phone calls and their reason for discontinuing treatment was recorded.
2.2 Data management and analysis
Data collected were transferred to a secure database, cleaned, and analysed using Microsoft Excel 2016®. Frequencies and percentages were used to summarize categorical variables and the output of this analysis is presented in text, figures, and tables.
3. Results
3.1 Common pediatric cancers
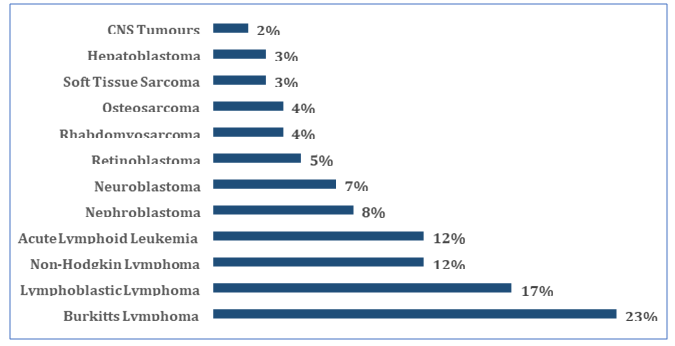
Data from the surveyed hospitals reported that 169 cases of pediatric cancers were diagnosed in 2019 and required chemotherapy. Figure 1 shows the frequency of the reported cancers in both hospitals. As illustrated, commonest cancer types in both hospitals diagnosed and treated in 2019 included Burkitt’s lymphoma (39, 23%), Lymphoblastic lymphoma (29, 17%), non-Hodgkin lymphoma (20, 12%), and acute lymphoid leukemia (20, 12%). Other cancers, including nephroblastoma, neuroblastoma, and retinoblastoma, among others were also identified but their frequencies were low, lower than 10% (Fig 1).
Table 1: Distribution of health facilities in Cameroon by type and by region
|
Region |
GH |
CH |
RHC |
RH |
DH |
CMA |
IHC |
Total |
|
AD |
0 |
0 |
1 |
1 |
12 |
17 |
154 |
185 |
|
CE |
2 |
8 |
0 |
1 |
49 |
95 |
1,429 |
1,584 |
|
ES |
0 |
0 |
1 |
1 |
21 |
21 |
220 |
264 |
|
EN |
0 |
0 |
1 |
3 |
30 |
27 |
384 |
445 |
|
LT |
2 |
2 |
0 |
2 |
53 |
78 |
1,159 |
1,296 |
|
NO |
1 |
0 |
1 |
1 |
16 |
9 |
287 |
315 |
|
NW |
0 |
0 |
1 |
1 |
30 |
32 |
346 |
410 |
|
OU |
0 |
0 |
1 |
1 |
35 |
68 |
727 |
832 |
|
SU |
0 |
1 |
1 |
1 |
13 |
34 |
260 |
310 |
|
SW |
0 |
0 |
1 |
2 |
32 |
26 |
276 |
337 |
|
Total |
5 |
11 |
8 |
14 |
291 |
407 |
5,242 |
5,978 |
AD-Adamawa; CE-Center; ES-East; EN-Extreme North; LT-Littoral; NO-North; NW-Northwest; OU-West; SU-South; SW-Southwest; GH-General Hospital; CH-Central Hospital; RHC-Regional Hospital Center; RH-Regional Hospital. CMA-Sub-divisional Hospital; IHC-Integrated Health Center
3.2 Cancer service capacity
Both facilities offered pediatric chemotherapy and palliative care services. Whereas MBH offered surgery for pediatric cancers needing surgical treatment, the MCC/ often referred this category of patient to a surgeon or a special hospital, subject to the type of surgery required. In addition, neither of the facilities offered nuclear medicine nor radiotherapy service at the time of the survey. However, it’s worth noting that MBH has engaged rehabilitation works to restore its radiotherapy services.
3.3 Human resource capacity
Table 2 shows the distribution of human resources for pediatric cancer in the two hospitals. We enumerated one pediatric hemato-oncologist, one surgical oncologist, and one medical oncologist in the surveyed hospitals. However, there were pediatric residents working in the hemato-oncology unit of MCC/CBF whom we did not include as specialists, given their schedule at the unit. In addition, the Groupe Franco Africaine d’Oncologie Pédiatrique (GFAOP) offers an 18-month training course in paediatric oncology. At the time of the assessment, one of the current residents had completed this paediatric oncology course. Therefore, there were three pediatric oncologists for an expected 1552 incident cases of childhood cancers annually. Furthermore, about 40% (18/45) of staff involved in pediatric oncology have received formal training in pediatric oncology. All surveyed hospitals had psychosocial support personnel, including chaplains, teachers, trained nurses, and volunteer staff who supported the clinicians to provide psychotherapy to patients and their families.
Table 2: Distribution of human resources involved in pediatric cancer care in two pediatric cancer hospitals in Cameroon.
|
Staffing |
MCC/CBF |
MBH |
Total |
|
Trained health care workers (Specialists) |
|||
|
Oncology Nurse |
4 |
10 |
14 |
|
Surgical oncologists |
0 |
1 |
1 |
|
Pediatric Hemato-Oncologist |
1 |
0 |
1 |
|
Medical Oncologist |
0 |
1 |
1 |
|
Residents |
1 |
0 |
1 |
|
Subtotal |
6 |
12 |
18 |
|
Other HCW involved in cancer care |
|||
|
Nurse |
10 |
10 |
20 |
|
General Practitioners |
2 |
1 |
3 |
|
Data Clerks |
0 |
2 |
2 |
|
Medical Secretary |
1 |
1 |
2 |
|
Subtotal |
13 |
14 |
27 |
3.4 Average cost of chemotherapy pre-treatment
We assessed the average cost of chemotherapy, focusing on the cost incurred during pre-treatment workup, by combining data on the cost of pre-treatment work-up2, as these were the only consistent data available across the two sites. Table 3 summarizes the approximate cost of the different components of pre-treatment work-up. Overall, the average cost for pre-treatment work-up was ~28,408 FCFA (US $46), ranging from ~23,500 FCFA (US $38) to ~64,950 FCFA (US $105). We did not obtain reliable data on the cost of pediatric chemotherapy sessions as these varied per case and per cancer type.
Table 3: Cost of pre-treatment work-up (103 FCFA)
|
Variable |
Min (USD*) |
Max (USD) |
Average (USD) |
|
Pre-treatment Laboratory Investigations |
|||
|
Complete Blood Count |
3.5 (5.7) |
6.9 (11.2) |
5.3 (8.6) |
|
SGOT |
1.0 (1.6) |
4.0 (6.5) |
2.5 (4.0) |
|
SGPT |
1.0 (1.6) |
4.0 (6.5) |
2.5 (4.0) |
|
Creatinine |
2.0 (3.2) |
2.5 (4.0) |
2.3 (3.7) |
|
Electrolytes |
2.0 (3.2) |
11.5 (18.6) |
6.8 (11.0) |
|
Glycemia |
1.0 (1.6) |
2.5 (4.0) |
1.8 (2.9) |
|
X-Ray |
6.0 (9.7) |
8.5 (13.8) |
7.3 (11.8) |
|
Ultrasound |
7.0 (11.3) |
25.0 (40.5) |
16.0 (25.9) |
USD = United States Dollar; SGOT = Serum glutamic oxaloacetic transaminase; SGPT = Serum glutamic pyruvic transaminase. Conversion from FCFA to USD was done at https://www1.oanda.com/currency/converter/ on 27 December 2022.
3.5 Treatment dropout
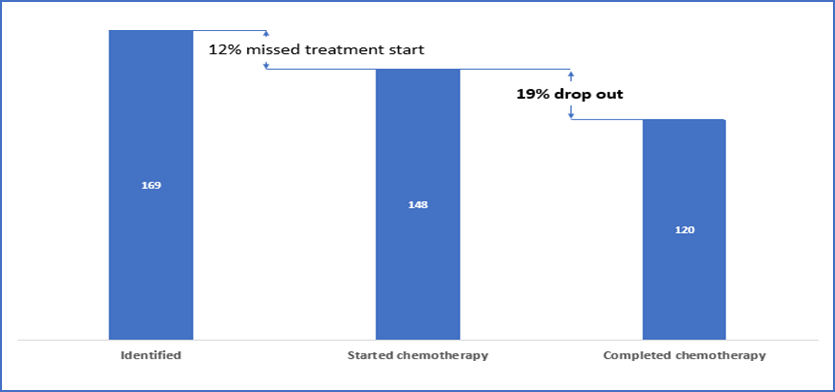
We considered treatment dropout as treatment discontinuation for at least four weeks consecutively [12]. Of the 169 cancer cases requiring chemotherapy, 148 (88%) initiated chemotherapy. However, among those that started chemotherapy, 28 did not complete the required number of sessions, corresponding to a treatment dropout rate of 19%. In total, about 30% of patients with pediatric cancer, who were eligible for chemotherapy, did not receive treatment. Figure 2 illustrates the pediatric chemotherapy cascade for the two hospitals.
3.6 Primary reasons for treatment abandonment
Among the 28 children that did not complete the required number of sessions, we probed further to identify primary reasons Table 4 illustrates the primary reasons for treatment abandonment among the children that started chemotherapy. As illustrated, the leading reason was insufficient funds to pay for chemotherapy sessions (11, 39%). We were not able to get in touch with 9 families and so their reasons for treatment abandonment were not identified.
Table 4: Primary reasons for not completing chemotherapy sessions among pediatric cancer patients
|
Reasons for chemotherapy treatment abandonment |
n |
% |
|
Insufficient funds to pay for treatment package |
11 |
39% |
|
Other unspecified family decision |
5 |
18% |
|
Preference for other treatment plans (e.g herbalist, traditionalist etc) |
3 |
11% |
|
Unknown reasons (could not get in touch with family) |
9 |
32% |
|
28 |
3.7 Patient status disclosure and follow-up
Oncologists and oncology nurses were mostly responsible for disclosing cancer status to patients and their families in both sites as illustrated in Table 5. Other staff, including residents, psychosocial support staff and chaplains, were occasionally involved in the disclosure process; however, we could not ascertain whether these staff have received training on disclosure of cancer status.
Table 5: Staff that conduct pediatric cancer status disclosure
|
Staff |
MBH |
MCC/FCB |
|
Oncologist |
Yes |
Yes |
|
Residents |
Yes |
Yes |
|
Oncology nurse |
Yes |
No |
|
Chaplains |
Yes |
No |
|
Medical Secretary |
No |
Yes |
MBH = Mbingo Baptist Hospital
MCC/CBF = Mother and Child Centre/Chantal Biya Foundation
3.8 Data Systems
Both sites had at least one data collection tool, including a cancer service register, monthly reporting forms, and a cancer registry. However, data collection tools were not harmonized, and there was no data reporting scheme for pediatric cancer in both sites.
4. Discussion
This study describes the current state of pediatric cancer services in Cameroon, and suggests the need for considerable expansion in reach, type, and specialization of services provided. Nearly two-thirds of current staff in pediatric oncology services have not received prior pediatric oncology capacity building. Pediatric chemotherapy pre-treatment investigations are expensive for the average Cameroonian family. As a result, about 30% of children with cancer abandoned treatment. In addition, the overburdened oncologists were required to conduct patient education and disclosure of cancer status, sometimes in combination with caregivers or parents. Regarding data management, data collection tools were available but not harmonized at cancer sites, and there was no systematic data reporting scheme for pediatric cancer data. The fact that just two of the nearly 6,000 facilities in Cameroon are offering pediatric oncology services, is an appalling finding, which further re-iterates the negligence that these categories of patients with curable cancers face. To us, this is clarion call to action to address this unmet need for pediatric cancer patients- both to the government and the international donor committee.
These findings suggest that pediatric cancer services in Cameroon need serious and urgent expansion and modernization, which lends support to findings from most parts of Africa. Only about 71% of countries in Africa had a functional national cancer control programme, with substantial variations in cancer services within countries [13]. Therefore, the need to address these service capacity gaps is imminent as these will enable investments in cancer control to prevent premature death. This can be done in a phased approach, progressively expanding pediatric chemotherapy services to targeted regional hospitals and similar structures across the nation, creating and integrating regional cancer control units under the leadership of regional delegations of public health. At the health district level, community health workers need to be trained to identify early warning signs and rapidly detect suspected cases through simple gestures. Adequate human resource capacity is critical for effective and holistic cancer management. However, surveyed cancer treatment centers lacked the human capacity for optimal pediatric cancer care. Furthermore, the University system does not produce sufficient oncologists to match the escalating burden of this disease. Nearly two-thirds of staff involved in pediatric oncology service had not undertaken specialty training in this domain, suggesting the need to design and roll out several human resource interventions for cancer control in the country. This may involve instituting a system for periodically training key staff, including pediatric oncologists, pediatric oncology surgeons, and oncology nurses. Another entails strengthening the capacity of existing staff by rolling out training on the early detection of common cancers and building their capacity on essential concepts of chemotherapy and palliative care. Improving the quality of health personnel in pediatric treatment facilities can play a great role in children’s treatment outcomes [14]. This should include incorporating palliative into all childhood cancer treatment facilities to meet the multidisciplinary needs of children and their families as well as proven approaches to disclose information to patients and their families The latter is important because poor management of information of the disclosure process can result into complications, grief, and poor mental health in children and their surviving families [15]. It is also important to implement systems to provide newly recruited staff with skills to support cancer care and treatment effectively and rapidly. Furthermore, there is a need for continuous human resource gaps assessments and addressing training and retraining needs.
In this assessment, Burkitt lymphoma was reported as the most treated pediatric cancer, representing nearly one-quarter of all pediatric cancer patients in Cameroon. This highly aggressive and fast-growing tumour has been previously described as the most common childhood cancer, especially in tropical African countries where malaria is holoendemic [16]. Recent evidence suggests a strong association between malaria and Burkitt lymphoma [16, 17]. However, whether this association is causal remains uncertain, partly because data on the epidemiology of Burkitt lymphoma in sub-Saharan Africa are rare even from the most affected countries like Malawi, Uganda, Nigeria, and Cameroon. In addition, over 80% of Burkitt lymphoma is associated with the Epstein-Barr virus, and Burkitt lymphoma is predominant in boys and children aged 5-9 years.
We found a high abandonment rate for pediatric cancer treatment of about 30%. Specifically, about 12% of children who needed chemotherapy did not get it, and approximately 20% of those on chemotherapy did not complete the required treatment sessions. High treatment abandonment rates have been reported in sub-Saharan African countries ranging from 15-60%. The reasons for treatment abandonment are multifactorial, including a high cost of care, poor awareness, long distances to treatment centers, absence of health insurance coverage, the high toxicity of treatment, long chemotherapy sessions, absence of social support, and fear of the unknown [18-20]. Inequities in treatment options are a major factor in the disparity in treatment between developed and developing, yet this is under-researched and receives little attention when reporting the Sustainable Development Goals [21]. In addition, treatment abandonment rates are associated with failure and poor survival rates [19]. Therefore, there is a need to improve access to chemotherapy by harmonizing protocols, upgrading the technical platforms of specialised structures, ameliorating forecasts, and strengthening financial resource mobilization for procuring cancer products.
Cancer status was mostly disclosed by already overburdened oncologists and oncology nurses in most instances, despite the availability of staff who could handle patients’ status disclosure if empowered with the appropriate training. Organizing capacity-building sessions on status disclosure for relevant hospital staff and community health workers could go a long way to improve pediatric cancer patient education, tracking and follow-up.
Data collection and reporting are critical for informed decision-making for enhanced health services. Although both surveyed facilities had data collection tools, data collection was not harmonized in terms of tools for collection and time for collection. In addition, there was no scheme in place for reporting pediatric cancer data to regional and central levels for policymaking. This significantly hinders research and development, warranting developing a harmonized national data collection tool with selected variables and indicators. In addition, the said indicators could be customized into the national health information software 2 (DHIS2). Furthermore, the data tools could be leveraged in the long term to build a functional pediatric cancer registry.
We found that optimal pediatric oncology care in Cameroon is compromised by limited-service availability and inadequate human resource capacity. In addition, a high proportion of children eligible for chemotherapy abandoned treatment due to high cost of treatment package. Furthermore, the lack of harmonization of data collection tools and the absence of a standard data reporting mechanism hinders informed decision-making. To address all these needs, stakeholders need to develop a national strategy for pediatric cancer care. Our study suggests an urgent need to expand pediatric oncology case identification services and build human resource capacity on treatment initiation, patient education and tracking to minimize dropout rates. In addition, harmonizing pediatric cancer data collection tools and designing a reporting scheme will facilitate the creation of a pediatric cancer registry. Furthermore, synchronizing pediatric cancer data with the national health system software will increase the visibility of pediatric cancer burden across the nation. Once the data has been collected and centralised, sufficiently equipped technical teams must be put into action to develop interventions with a high public health impact. Finally, there is imminent need for the creation of a nation cancer institute which will bring together cancer specialists (oncologists, radiologists, surgeons etc) in a common technical platform.
Conflict of Interest
All authors declare no conflict of interest. We do not have any reason why any colleagues/authors should not be reached out to review this article prior to publication.
Acknowledgment
All activity related cost in this assessment including travels and meetings was achieved throught generous funding from the UBS Optimus Foundation.
All authors have each contributed significantly to develop and review the manuscript as follows:
Conception and design: YS, AF, EK, SDC
Data collection: BSEM, NMG, AK
Data analysis and interpretation: AF, BSEM, JN
Manuscript writing: AF, VN, BSEM,
Manuscript revision: AF, BSEM, VN, JN, NMG, AK, GM, FT, OD, EK, AHP, PN, YS
All the authors approved the final version of the manuscript.
References
- Force LM, Abdollahpour I, Advani SM, Agius D, Ahmadian E, Alahdab F, et al. The global burden of childhood and adolescent cancer in 2017: an analysis of the Global Burden of Disease Study 2017. The Lancet Oncology 20 (2019): 1211-25.
- WHO Global Report on cancer: Setting priorities, investing wisely and providing care for all (2021). Available at https://www.who.int/publications/i/item/9789240001299
- Union for International Cancer Control (UICC) Global Cancer Data: GLOBOCAN 2018 | UICC (2018). Available at https://www.uicc.org/news/global-cancer-data-globocan-2018
- Weaver MS, Yao AJJ, Renner LA, Harif M, Lam CG. The prioritisation of paediatrics and palliative care in cancer control plans in Africa. Br J Cancer 112 (2015): 1845-56.
- Bhakta N, Force LM, Allemani C, Atun R, Bray F, Coleman MP, et al. Childhood cancer burden: a review of global estimates. The Lancet Oncology 20 (2019): e42-53.
- Steliarova-Foucher E, Colombet M, Ries LAG, Moreno F, Dolya A, Bray F, et al. international incidence of childhood cancer, 2001-10: a population-based registry study. Lancet Oncol 18 (2017): 719-31.
- Gupta S, Howard SC, Hunger SP, Antillon FG, Metzger ML, Israels T, et al. Treating Childhood Cancer in Low- and Middle-Income Countries. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, editors. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank (2015).
- United Nations International Children Emergency Fund (UNICEF), Annual Report. UNICEF (2015). Available at https://www.unicef.org/reports/unicef-annual-report-2015
- International Agency for Research on Cancer. (IICC): International Incidence of Childhood Cancers Registry-specific tables. Available at https://iicc.iarc.fr/results/registry-specific-tables/
- The World Factbook Archives (2022). Available at https://www.cia.gov/the-world-factbook/countries/cameroon/
- Yauba Saidu, Jessica Gu, Budzi Michael Ngenge, Sangwe Clovis Nchinjoh, Amani Adidja, Nadege Edwige Nnang, Nkwain Jude Muteh, Vouking Marius Zambou, Clarence Mvalo Mbanga, Valirie Ndip Agbor, Diaby Ousmane, Andreas Ateke Njoh, Junie Flegere, Demba Diack, Owens Wiwa, Emanuel Montomoli Sue Ann Costa Clements and Ralf Clemens. The faces behind vaccination: unpacking the attitudes, knowledge, and practices of staff of Cameroon’s expanded program on Immunization. Human Resources for Health (2023) 21:88
- Mostert S, Arora RS, Arreola M, Bagai P, Friedrich P, Gupta S, et al. Abandonment of treatment for childhood cancer: position statement of a SIOP PODC Working Group. Lancet Oncol 12 (2011): 719-20.
- WHO | Regional Office for Africa Where does cancer care stand in Africa today?. Available at https://www.afro.who.int/news/where-does-cancer-care-stand-africa-today
- T Peter Kingham, Olusegun I Alatise, Verna Vanderpuye, Corey Casper, Francis A Abantanga, Thaim B Kamara, Olufunmilayo I Olapade, Muhammad Habeebu, Fatimah B Abdulkareem, and Lynette Denny. Treatment of cancer in sub-Saharan Africa - The Lancet Oncology 14 (2013):4 E158-E167
- Ulrika C Kreicbergs, Patrizia Lannen, Erik Onelov, Joanne Wolfe. Parental grief after losing a child to cancer: impact of professional and social support on long- term outcomes. Journal of Clinical Oncology 2007 Aug 1;25(22:3307-12.)
- Stefan C, Bray F, Ferlay J, Liu B, Maxwell Parkin D. Cancer of childhood in sub-Saharan Africa. Ecancermedicalscience 11 (2017): 755.
- Molyneux EM, Rochford R, Griffin B, Newton R, Jackson G, Menon G, et al. Burkitt’s lymphoma. The Lancet 379 (2012): 1234-44.
- Harif M, Traoré F, Hessissen L, Moreira C, Atteby J-J. Challenges for paediatric oncology in Africa. The Lancet Oncology 14 (2013): 279-81.
- Mirutse MK, Tolla MT, Memirie ST, Palm MT, Hailu D, Abdi KA, et al. The magnitude and perceived reasons for childhood cancer treatment abandonment in Ethiopia: from health care providers’ perspective. BMC Health Services Research 22 (2022): 1014.
- Mansell R, Purssell E. Treatment abandonment in children with cancer in Sub-Saharan Africa: Systematic literature review and meta-analysis. J Adv Nurs 74 (2018): 800-8.
- Wirtz VJ, Hogerzeil HV, Gray AL, Bigdeli M, de Joncheere CP, Ewen MA, et al. Essential medicines for universal health coverage. Lancet 389 (2017): 403-76.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 