Influence of Stress on the Physiological and Psychological Well-Being of Medical Students, As Measured By Heart Rate Variability and the Perceived Stress Scale
Mark Miller, Matthew Miller, Samuel Weldon, Nathaniel Cintron, Cade Kelleher, Santiago Lorenzo*
Lake Erie College of Osteopathic Medicine, Bradenton, FL
*Corresponding author: Santiago Lorenzo, Lake Erie College of Osteopathic Medicine, 5000 Lakewood Ranch Blvd. Bradenton, FL
Received: 02 October 2022; Accepted: 10 October 2022; Published: 07 November 2022
Article Information
Citation: Mark Miller, Matthew Miller, Samuel Weldon, Nathaniel Cintron, Cade Kelleher, Santiago Lorenzo. Influence of Stress on the Physiological and Psychological Well-Being of Medical Students, As Measured By Heart Rate Variability and the Perceived Stress Scale. Fortune Journal of Health Sciences 5 (2022): 560-566.
View / Download Pdf Share at FacebookAbstract
Background: It is well documented that stress poses a serious challenge to students’ health in medical school. The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring the perception of stress. Heart rate variability (HRV) may provide an objective measure of the physiologic index of stress in medical students. This study investigated the impact of one semester of medical school on HRV and PSS in first-year medical students.
Methods: Forty-eight first-year medical students at the Lake Erie College of Osteopathic Medicine, Bradenton campus were recruited for a prospective observational study from January through December of 2021. HRV analysis via electrocardiogram was performed alongside PSS administration at the beginning, as well as at the end of a medical school semester. Paired t-tests were performed to assess HRV via SDNN, RMSSD, and PSS scores. Pearson Correlation analysis was performed to investigate correlations between HRV indices and PSS results.
Results: By the end of the academic semester, students presented with increased PSS scores compared to the beginning of the academic semester (12.674 ± 0.750 vs 20.587 ± 1.004, P < 0.001). There were also statistically significant decreases in HRV post semester as measured by SDNN (108.16 ± 13.86 vs 56.36 ± 4.07, P < 0.001) as well as RMSSD (127.43 ± 21.71 vs. 61.55 ± 34.92, P < 0.001). Pearson Product Moment Correlation was performed and revealed a statistically significant inverse relationship between percent changes in PSS compared to percent changes in SDNN (R-value -0.334, P = 0.0287) as well as percent changes in RMSSD (R-value -0.369, P = 0.0149).
Conclusion: These results demonstrate that first-year medical students are experiencing significant levels of stress after an entire academic semester. This study demonstr
Keywords
<p>Heart Rate Variability, Perceived Stress Scale, Medical Education</p>
Article Details
1. Background
For decades, it has been recognized that the stress of medical school poses a serious challenge to students’ health [1-5]. Medical students have consistently reported rates of psychological stress [6-7] and depression [3-4] that are significantly higher than those in the same age cohort in the general population. Not surprisingly, the stress experienced by first-year medical students has been reflected in their health habits, with reports of decreased physical activity and sleep, along with declining general health [8-9]. The stress experienced by medical students is a likely contributor to burnout, which has been associated with less altruistic professional views [10], as well as increased thoughts of dropping out of school [11].
In addition to mental effects, stress also has a significant physical impact on medical students and its long-term effects on humans are well-documented [12, 13]. Individuals who experience chronic stress are at increased risk for conditions such as cardiovascular disease and metabolic dysregulation [12, 14-15]. As previously mentioned, the stress experienced by medical students can lead to changes in their diet, decreased sleep quality, as well as decreased participation in recreational activities [8, 9]. This presents an area of research that has only been explored on a limited basis to date. Previous studies in medical students have indicated HRV changes in the shorter term concerning mainly pre-, intra-, and post-exam circumstances [16, 17]. Yoo et. al. [16] performed HRV measurements during examinations and revealed that performance during examinations was directly correlated with increased HRV indices, indicating that students who demonstrated lower levels of stress on HRV performed better during examinations. Hammond et al. [17] demonstrated in a similar intra-examination HRV measurement experiment that HRV indices were notedly increased during examinations, and this finding persisted regardless of the year of academic study. The goal of this study is to expand upon these findings and investigate whether these intra-examination findings are noted throughout the duration of an entire academic semester.
There are different approaches to assess degree of stress on an individual. The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring the perception of stress with established acceptable psychometric properties [18-21]. The PSS has been previously administered to assess the levels of medical student stress, which were found to be significantly higher than those in the same age cohort in the general population [22-24]. Heart rate variability (HRV) can be defined as the variation in the time interval between consecutive heartbeats and can be measured as RR interval variation [25]. It has been suggested that HRV reflects the capacity of the body to deal with ongoing demands [27]. There is an established inverse relationship between psychological stressors and HRV [28-30]. Decreases in HRV have also been associated with increased risk for cardiovascular disease [31-32], obesity [33], and anxiety [34]. Thus, it has been postulated that HRV may serve as a biomarker for future screening of physiological and psychological health [36]. Measuring the HRV in medical students and tracking it throughout an entire semester would provide an objective measure of the physiologic index of stress.
It has been previously demonstrated that both short-term psychological stress [37] and increases in perceived stress [38] have negative influences on HRV. The results from previous studies suggest that the stress experienced by medical students [1-7], coupled with changes in student health habits [8-9] has the potential to negatively impact HRV [28-33]. Though HRV has been shown to correlate with both physiological and psychological health [25-27], studies have yet to assess the combined effects of stress on the PSS and HRV in medical students during an entire academic semester. Therefore, the purpose of this study is to investigate the influence of stress on the physiological and psychological health of first-year medical students, as it correlates to changes in HRV and PSS. We hypothesized that one semester of medical school will increase PSS scores and decrease HRV values as measured by the standard deviation of RR intervals (SDNN) and the square root of the mean of the sum of the squares of differences between adjacent RR intervals (RMSSD).
2. Methods
2.1 Study Design and Timeline
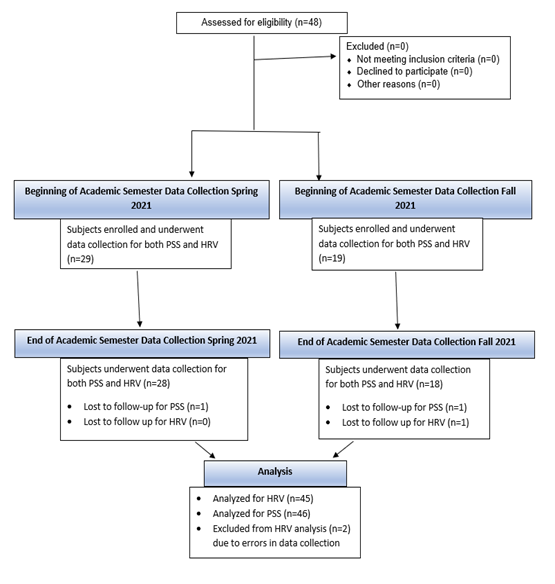
This study was approved by the Institutional Review Board, and it was conducted from January to December 2021 as a project within the Lake Erie College of Osteopathic Medicine, Bradenton campus. Two cohorts of subjects were gathered during the study. The initial cohort (n = 29) was during the Spring 2021 academic semester. The final cohort (n = 19) was during the Fall 2021 academic semester (Figure 1). Both cohorts completed PSS and HRV measurements at the start of the academic semester (during the first week) and within 1 week from the end of the semester.
2.2 Participants
First-year medical students were recruited via an email announcement to the entire class. Before participation, each volunteer gave written informed consent as set forth by the Declaration of Helsinki. All protocols were approved by the Institutional Review Board of Lake Erie College of Osteopathic Medicine. Forty-eight first-year medical students (15 men, 33 women), aged 21 to 28 years old, completed the protocol. The subject’s privacy was protected by subject number assignment and all identifying information was under lock and key in the principal investigator’s office. As the entire pool of possible research subjects was enrolled in medical school, data from previous PSS studies with similarly aged cohorts that were representative of the normal population were utilized for comparison purposes [18-21].
2.3 Perceived Stress Scale
Subjects completed the PSS questionnaire at the start of the semester and then completed the same questionnaire following the completion of their academic semester. This questionnaire was given to the subjects directly after completion of the electrocardiogram (ECG) recording. The PSS has been widely used and has been validated in prior studies [18-21]. We utilized the PSS as a quantitative measure of perceived stress in order to correlate with changes in HRV.
2.4 Heart Rate Variability Recording and Analysis
The recommendations of the Task Force on HRV were followed for recording short-term HRV [38]. Subjects were instructed to refrain from heavy physical activity for 24 hours and from consumption of alcohol or caffeine for at least 12 hours prior to the recording. Subjects presented to the study appointment in minimal, loose clothing, and after emptying their bladder. The subjects sat comfortably while the HRV recording procedure was explained to them. This enabled them to become accustomed to the environment with dim lighting in a thermoneutral room environment. Bioharness (Zephyr, USA), a portable, wireless data acquisition system for electrocardiography was then applied [39]. After ten minutes of supine rest, a lead II ECG was acquired at a rate of 200 samples/second for 10 minutes in a supine resting position.
After excluding the artifacts and ectopics from the RR interval series given by the Bioharness, a stable five-minute RR interval series was chosen and analyzed with Kubios HRV Version 2.0 software for HRV (Bio-signal analysis Group, Finland) [40-42] (Figure 3). HRV analysis software analyzes the RR interval time-domain components, and the results are given as standard deviation of RR intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent RR intervals (RMSSD). These methods have been validated in previous studies [43-44], and the results obtained from these methods have been proven to be a reliable method to determine HRV [44].
2.5 Statistical Analysis
The PSS and HRV data were recorded, and statistical analyses (paired t-tests) were performed on Sigma Plot (Systat Software, Inc., Chicago, IL) to assess SDNN, RMSSD, and PSS scores. A value of P < 0.017 was considered statistically significant after applying the Bonferroni correction for three comparisons.
3. Results
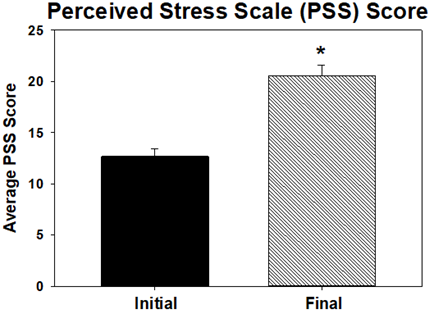
Forty-six out of 48 total subjects’ PSS scores were analyzed. Two subjects failed to complete a final PSS questionnaire. Therefore, these two subjects were not included in the subsequent analysis. Forty-five out of 48 total subjects were analyzed for HRV. One subject failed to complete a final ECG and two subjects’ initial ECGs were collected incorrectly by study staff. By the end of the academic semester, students presented with increased PSS scores (20.587 ± 1.004) compared to the beginning of the academic semester (12.674 ± 0.750; P < 0.001; Figure 2).
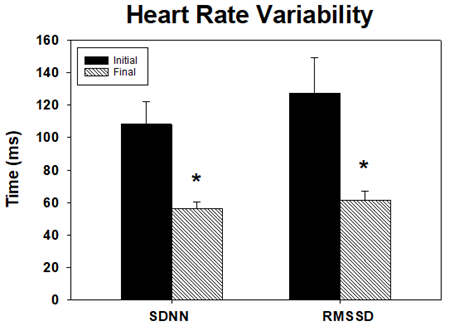
At the beginning of the academic semester, students presented significantly higher SDNN (108.16 ± 13.86) as well as RMSSD (127.43 ± 21.71) values compared to end of semester values (SDNN;56.36 ± 4.07; RMSSD;61.55 ± 34.92; all P < 0.001; Figure 3).
Pearson Product Moment Correlation was performed and revealed a statistically significant inverse relationship between percent changes in PSS compared to percent changes in SDNN (R-value -0.334, P = 0.0287), as well as percent changes in RMSSD (R-value -0.369, P = 0.0149).
4. Discussion
The purpose of this study was to investigate the influence of stress on the physiological and psychological health of first-year medical students, as it correlates to changes in HRV and PSS. We observed that one semester in medical school resulted in a statistically significant increase in the PSS as well as a statistically significant decrease in HRV indices.
Generally, increased stress leads to a shift in the autonomic nervous system. This results in an increase in sympathetic output and a subsequent decrease in parasympathetic tone [26]. This is reflected in HRV via decreased SDNN and RMSSD parameters [25, 27]. At the end of the academic semester, the students in our study exhibited a significant decrease in these HRV indices as hypothesized (Figure 3). Previous studies in medical students have indicated similar HRV changes in the shorter term concerning mainly pre-, intra-, and post-exam circumstances [16, 17]. To our knowledge, this is the first study to assess the effects of an entire semester on PSS and HRV values in medical students. The findings within this study expand upon the previous findings noted in earlier studies by demonstrating that these patterns are present throughout the academic semester and are not limited to intra-examinational times. While it is well documented that students experience stress, the findings in this study demonstrate a modality to quantify this stress with an objective tool, such as HRV.
Our reports of stress levels at the start of the semester (as indicated by PSS scores) are similar to scores obtained by previous studies in similarly aged cohorts [18-21]. Our end-of-semester results, however, demonstrate PSS scores that are greater than one standard deviation above the mean found in previous studies [18-21]. This difference was found to be statistically significant compared with the beginning of semester values (Figure 2). This substantial increase in perceived student stress is of utmost importance as mental health is becoming a pressing challenge in the lives and well-being of medical students.
While using PSS as a quantitative measure of perceived stress is undoubtedly beneficial due to its low cost and ease of administration, it is a subjective measure and relies on self-reporting. Objective methods to measure stress can be helpful to use alongside these traditional subjective measurements. An additional aim of this study was to investigate how HRV can be used to objectively measure stress levels. Our study revealed a statistically significant inverse correlation between PSS scores and HRV indices. This inverse relationship between stress and HRV has been described in previous studies [28-30, 44]. However, we were unable to find any previous literature describing this trend with the PSS, or this trend applied to medical students. Simultaneous assessment of HRV parameters and PSS scores presents a unique opportunity to measure the stress of medical students objectively while maintaining the low cost and ease of administration from the PSS survey.
Through investigating the relationship between HRV and PSS, it becomes possible to evaluate the well-being of medical students from a more holistic view by incorporating both subjective and objective data. The use of HRV provides an opportunity for medical schools to objectively “check in” on their students, and measure how the curriculum may be affecting their overall well-being. Upon viewing consistent decreases in HRV, schools can utilize this data to identify students who may be at increased risk of stress-related problems and provide them with options for extra support and counseling. Assessment of HRV creates the freedom to be proactive about student mental and physiological health and provides medical schools with another tool to objectively assess the levels of stress and possible burnout experienced by students.
5. Limitations
The present study would have benefitted from a larger number of participants, and from different medical schools. That said, our reported results are clear and showed a statistical difference in the PSS and HRV after one semester of medical school. Another possible challenge in the current study is the different data collection times between the two cohorts. Unfortunately, COVID precautions guidelines did not allow for entire data to be collected at the same time. That said, we are very confident in the results obtained as our comparison analyses between Spring and Fall cohorts showed no statistical differences, which highlights the consistency of our findings and that the observed results apply to the entire first year of medical school. Moreover, the course load in the Fall and Spring semesters of the first year of this medical school curriculum is remarkably very similar.
6. Conclusion
To our knowledge, this is the first study to report that, after an entire semester of medical school, there is a statistically significant increase in PSS and a subsequent decrease in HRV in first-year medical students. Through assessments of PSS scores and HRV during an entire academic semester in first-year medical students, this study demonstrates that the rigors of medical school have negative psychological and physiological effects on students. The strong evidence of simultaneous psychological and physiological deterioration in medical students illustrates the need for medical schools to improve their student wellness initiatives and mental health monitoring. To embody the holistic approach to healthcare, the mental and physical well-being of medical students should continue to be addressed. Further research is needed to elucidate the relationship between certain lifestyle/study habits and their effects on stress intensification or mitigation.
Declarations
Competing Interests:
None reported.
Funding:
Grant #: J2020.08
Name of Funding Organization:
Lake Erie College of Osteopathic Medicine and Lake Erie Consortium for Osteopathic Medical Training
Amount Awarded: $4,939.46
Title of Project: Influence of stress on the psychological and physiological wellbeing of first-year medical students, as measured by Heart Rate Variability and the Perceived Stress Scale.
Funding Distribution:
this grant was utilized to purchase Bioharness electrocardiogram monitors as well as for subject compensation.
Ethical Approval:
This study was approved by the Lake Erie College of Osteopathic Medicine International Review Board (Protocol 27-120). All protocols were approved by the Institutional Review Board of Lake Erie College of Osteopathic Medicine.
Informed Consent:
All patients/participants in this study provided written informed consent that was approved by the Lake Erie College of Osteopathic Medicine Institutional Review Board prior to participation. The Lake Erie College of Osteopathic Medicine institutional guidelines regarding the practice of ethical research were followed per the approved study protocol.
Consent for Publication:
Not Applicable.
Availability of Data and Material:
The data for this study has been made publicly available at the following link. 10.6084/m9.figshare.19945385
Author Contributions:
All above authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; all above authors drafted the article or revised it critically for important intellectual content; all above authors gave final approval of the version of the article to be published, and all above authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments:
We would like to acknowledge and sincerely thank the LECOMT Support Grant group for funding this project. We would also like to thank the LECOM Bradenton Osteopathic Manipulative Medicine Department for allowing us to conduct data collection in their space.
References
- Slavin, Stuart J, et al. “Medical Student Mental Health 3.0.” Academic Medicine (89) (2014): 573–577.
- Hill, Monica R, et al. “In Their Own Words: Stressors Facing Medical Students in the Millennial Generation.” Medical Education Online 23 (2018): 1530558.
- Lloyd, Camille, and Nanette K. Gartrell. “Psychiatric Symptoms in Medical Students.” Comprehensive Psychiatry 25 (1984): 552–565.
- Vitaliano, Peter P, et al. “Medical Student Distress. A Longitudinal Study.” The Journal of Nervous and Mental Disease 177 (1989): 70–76.
- Dyrbye, Liselotte N, et al. “Burnout and Serious Thoughts of Dropping Out of Medical School: A Multi-Institutional Study.” Academic Medicine 85 (2010): 94–102.
- Sherina MS, et al. “Psychological Stress among Undergraduate Medical Students.” Med J Malaysia 59 (2004): 207–211.
- Firth J. “Levels and Sources of Stress in Medical Students.” Bmj 292 (1986): 1177–1180.
- Wolf TM, and Kissling GE. “Changes in Life-Style Characteristics, Health, and Mood of Freshman Medical Students.” Academic Medicine 59 (1984): 806–14.
- Ball, Susan and Amy Bax. “Self-Care in Medical Education.” Academic Medicine 77 (2002): 911–917.
- Dyrbye, Liselotte N, et al. “Relationship between Burnout and Professional Conduct and Attitudes among US Medical Students.” Jama 304 (2010): 1173.
- Dyrbye, Liselotte N, et al. “Burnout and Serious Thoughts of Dropping Out of Medical School: A Multi-Institutional Study.” Academic Medicine 85 (2010): 94–102.
- Saeid Golbidi, Jefferson C. Frisbee and Ismail Laher “Chronic stress impacts the cardiovascular system: animal models and clinical outcomes.” Am J Physiol Heart Circ Physiol 308 (2015): H1476-H1498.
- Balkishan Sharma, Rajshekhar Wavare, Ajit Deshpande, Richa Nigam and Ramkrishna Chandorkar. “A study of academic stress and its effect on vital parameters in final year medical students at SAIMS Medical College, Indore, Madhya Pradesh.” Biomedical Research 22 (2011).
- Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. American Heart Association Statistics Committee, and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 125 (2012): e2–e220.
- Gullette EC, Blumenthal JA, Babyak M, Jiang W, Waugh RA, Frid DJ, et al. Effects of mental stress on myocardial ischemia during daily life JAMA 277 (1997): 1521–1526.
- Hammoud S, Karam R, Mourad R, Saad I, Kurdi M. Stress and Heart Rate Variability during University Final Examination among Lebanese Students. Behav Sci 9 (2019): 3.
- Yoo HH, Yune SJ, Im SJ, Kam BS, Lee SY. Heart Rate Variability-Measured Stress and Academic Achievement in Medical Students. Med Princ Pract 30 (2021): 193-200.
- Roberti, Jonathan W., et al. “Further Psychometric Support for the 10-Item Version of the Perceived Stress Scale.” Journal of College Counseling 9 (2006): 135–147.
- Hewitt, Paul L, et al. “The Perceived Stress Scale: Factor Structure and Relation to Depression Symptoms in a Psychiatric Sample.” Journal of Psychopathology and Behavioral Assessment 14 (1992): 247–257.
- Lee, Eun-Hyun. “Review of the Psychometric Evidence of the Perceived Stress Scale” Asian Nursing Research 6 (2012) 121–127.
- Kallingappa, Prasadbudri, et al. “Assessment of Perceived Stress and Association with Sleep Quality and Attributed Stressors among 1st-Year Medical Students: A Cross-Sectional Study from Karwar, Karnataka, India.” Tzu Chi Medical Journal 30 (2018): 221.
- Mallick, Asimkumar, et al. “Assessing Perceived Stress in Medical Personnel: In Search of an Appropriate Scale for the Bengali Population.” Indian Journal of Psychological Medicine 35 (2013): 29.
- Mohammed, Emansameh, et al. “Predictors of Perceived Stress among Medical and Nonmedical College Students, Minia, Egypt.” International Journal of Preventive Medicine 10 (2019): 107.
- Task Force of the European Society Electrophysiology. “Heart Rate Variability.” Circulation 93 (1996): 1043–1065.
- Laborde, Sylvain, et al. “Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research – Recommendations for Experiment Planning, Data Analysis, and Data Reporting.” Frontiers in Psychology . 08 (2017).
- Young, Hayley, and David Benton. “We Should Be Using Nonlinear Indices When Relating Heart-Rate Dynamics to Cognition and Mood.” Scientific Reports 5 (2015).
- Delaney JPA and Brodie DA. “Effects of Short-Term Psychological Stress on the Time and Frequency Domains of Heart-Rate Variability.” Perceptual and Motor Skills 91 (2000): 515–524.
- Dishman, Rod K, et al. “Heart Rate Variability, Trait Anxiety, and Perceived Stress among Physically Fit Men and Women.” International Journal of Psychophysiology 37 (2000): 121–133.
- Taelman J, Vandeput S, Spaepen A, Van Huffel S. Influence of Mental Stress on Heart Rate and Heart Rate Variability. In: Vander Sloten J, Verdonck P, Nyssen M, Haueisen J. (eds) 4th European Conference of the International Federation for Medical and Biological Engineering. IFMBE Proceedings 22 (2009).
- Mäkikallio, Timo H, et al. “Fractal Analysis of Heart Rate Dynamics as a Predictor of Mortality in Patients with Depressed Left Ventricular Function after Acute Myocardial Infarction.” The American Journal of Cardiology 83 (1999): 836–839.
- Bigger JT, et al. “The Ability of Several Short-Term Measures of RR Variability to Predict Mortality after Myocardial Infarction.” Circulation 88 (1993): 927–934.
- Kim JA et al. “Heart Rate Variability and Obesity Indices: Emphasis on the Response to Noise and Standing.” The Journal of the American Board of Family Medicine 18(2005): 97–103.
- Chalmers, John A, et al. “Anxiety Disorders Are Associated with Reduced Heart Rate Variability: A Meta-Analysis.” Frontiers in Psychiatry 5 (2014).
- Mouridsen, Mette Rauhe, et al. “Modest Weight Loss in Moderately Overweight Postmenopausal Women Improves Heart Rate Variability.” European Journal of Preventive Cardiology 20 (2012): 671–677.
- Stein, Phyllis K., et al. “Caloric Restriction May Reverse Age-Related Autonomic Decline in Humans.” Aging Cell 11 (2012): 644–650.
- Young, Hayley A and David Benton. “Heart-Rate Variability.” Behavioural Pharmacology 29 (2018): 140–151.
- Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93 (1996): 1043–65.
- Tarvainen, Mika P, et al. “Analysis and Preprocessing of HRV—Kubios HRV Software.” ECG Time Series Variability Analysis (2017): 159–186.
- Niskanen J-P, Tarvainen MP, Ranta-aho PO, and Karjalainen PA. Software for advanced HRV analysis. Comp Meth Programs Biomed 76 (2004): 73-81.
- Sharma, Vivek Kumar. “Heart Rate Variability in Adolescents – Normative Data Stratified by Sex and Physical Activity.” Journal of Clinical and Diagnostic Research (2015).
- Baek, Hyun Jae, et al. “Reliability of Ultra-Short-Term Analysis as a Surrogate of Standard 5-Min Analysis of Heart Rate Variability.” Telemedicine and e-Health 21 (2015): 404–414.
- Kiecolt-Glaser JK, Habash DL, Fagundes CP, Andridge R, Peng J, Malarkey WB, et al. “Daily stressors, past depression, and metabolic responses to high-fat meals: a novel path to obesity.” Biol Psychiatry 77 (2015): 653-60.
- Cohen, S and Williamson G. "Perceived stress in a probability sample of the US In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology" (1988): 31-67.
- Britton DM, Kavanagh EJ, Polman RCJ. Validating a Self-Report Measure of Student Athletes' Perceived Stress Reactivity: Associations with Heart-Rate Variability and Stress Appraisals. Front Psychol 10 (2019): 1083.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 