Outpatient COVID-19 Pneumonia in elderly Patients in Kazakhstan
Essetova GU, Idrissova LR*, Muminov TA
Department of pulmonology, Kazakh national medical university named after S.D. Asfendiarova, Almaty, Kazakhstan
*Corresponding author: Idrissova LR, Department of pulmonology, Kazakh national medical university named after S.D. Asfendiarova, Almaty, Kazakhstan.
Received: 19 July 2022; Accepted: 26 July 2022; Published: 02 August 2022
Article Information
Citation: Essetova GU, Idrissova LR, Muminov TA. Outpatient COVID-19 Pneumonia in elderly Patients in Kazakhstan. Fortune Journal of Health Sciences 5 (2022): 446-453
View / Download Pdf Share at FacebookAbstract
Background: COVID pneumonia is difficult to manage in elderly patients over 65 years of age. The aim of the study was to determine the clinical features of the course of COVID pneumonia in a cohort of patients over 65 years old.
Materials and Methods: We observed patients with community-acquired pneumonia, of whom PCR positive for COVID were 33 patients, mean age 67.6 ± 12 years, men – 11, women – 22; 16 patients had no confirmed virus (COVID PCR negative), mean age 65.5 ± 8.2 years, 7 women and 9 men.
Examination results: In the group of COVID patients, the disease more often proceeded according to the type of bilateral polysegmental pneumonia according to CT data, with severe monocytosis, c thrombocytosis and transient increase in creatinine, which required the appointment of intensive anticoagulant therapy. Arterial hypertension was observed in the majority of people. In the control group (PCR -), pneumonia proceeded predominantly as bronchopneumonia, saturation indices were approximately the same in both groups. COVID patients had significantly higher levels of monocytes, blood platelets, CRP, creatinine levels, including arterial hypertension was more common.
Conclusion: COVID pneumonia in elderly patients proceeds as multisegmented bilateral pneumonia with moderate disseminated intravascular coagulation syndrome, which is well controlled due to complex therapy with anticoagulants and antibiotics.
Keywords
<p>COVID, pneumonia, elderly</p>
Article Details
1. Background
The pandemic of the new coronavirus infection is accompanied by a high incidence of community-acquired pneumonia (CAP) [1].
The severity of the condition is connected, both by the viral pneumonia itself, and by the addition of a secondary infection, with community-acquired infection with pneumococcus, mycoplasma pathogens. Viral lung damage in coronavirus pneumonia is accompanied by the following features: acute onset of the disease with pneumonia, without prior bronchitis, which quickly becomes polysegmental, often bilateral lung lesions [2]. The severity of the condition is enhanced by the phenomena of disseminated intravascular coagulation (DIC), which can lead to the development of multiple organ failure due to ischemia [3].
In Kazakhstan, according to the data of the Ministry of Health of the Republic of Kazakhstan, which is confirmed by the WHO, 39104 cases of COVID pneumonia, of which 29182 recovered, 409 died, the mortality rate is 1.04% [4]. The aim of this study was to study the features of the clinical course of community-acquired COVID infection in elderly adults (≥ 65 years) on an outpatient basis.
2. Research Materials and Methods
Analyzed 49 cases of pneumonia, COVID-19 status was confirmed by PCR. Research methods: all patients underwent a general clinical study, including saturation, complete blood count, biochemical study, coagulation tests, as well as determination of respiration and hemodynamic parameters. All patients underwent multispiral computed tomography in dynamics, at admission and at discharge. The evaluation of the clinical data of patients was approved by a Local Ethical Commission of the KazNMU named after S.D. Asfendiyarov (#968 from 23/10/20).
Results are presented as mean ± standard deviation (m ± SD), significance was determined by Student's t test or ANOVA, where p≤0.01 was considered significant.
3. Results and Discussion
Table 1 presents data on the studied cohort of patients. There were 49 patients under observation in the hospital, of which 33 were positive for COVID PCR, the average age was 67.6 ± 12 years, men - 11 women - 22, designated as group 1 – main studied. In 16 patients, the virus was not confirmed (COVID PCR negative), the average age was 65.5 ± 8.2 years, 7 women and 9 men, designated as group 2 - control.
Table 1: Comparison COVID-19 positive and COVID-19 negative patients
|
Group 1 |
Group 2 |
|||
|
PCR COVID positive status |
33 |
100% |
0 |
0% |
|
Number of patients |
33 |
100% |
16 |
100% |
|
Age |
67.6±12 |
65.5±8.2 |
||
|
Gender F (M) |
22 (11) |
66.7% (33.3%) |
7(9) |
47% (53%) |
|
CT polysegmental bilateral |
||||
|
pneumonia |
28 |
84.80% |
7 |
43.75% |
|
CT Bronchopneumonia |
0 |
0 |
9 |
56.25% |
|
Arterial hypertension |
23 |
69.7%* |
8 |
50% |
|
Ischemic heart disease |
11 |
33.30% |
8 |
50% |
|
Type 2 diabetes |
7 |
21.20% |
2 |
12.50% |
|
Hospitalization (days) |
22.4±14,6 |
16±11 |
||
Among 33 COVID-positive patients with signs of acute pneumonia, in 28 (84.8%) confirmed by spiral computed tomography revealed polysegmental bilateral pneumonia. It should be noted that they have comorbid pathology, in 23 of 33 (69.7%) patients arterial hypertension (AH) was noted, in 11 (33.3%) ischemic heart disease (IHD), diabetes mellitus (DM type 2) - 7 (21.2%) sick. The duration of hospitalization in COVID-positive patients was 22.4±14.57 days and in COVID-negative patients 16±11 days. Among 16 COVID-negative patients with pneumonia, according to CT of the lungs, 7 patients (43.75%) confirmed polysegmental bilateral pneumonia, and 9 (56.25%) - bronchopneumonia. Table 2 shows the saturation data according to pulse oximetry and hemodynamic data, including heart rate, respiration rate (RR), blood pressure (BP), body temperature and serum hemoglobin.
Table 2: Hemodynamics and respiration in pneumonia patients with or without COVID-19
|
Group 1 |
COVID positive |
Group 2 |
Control |
|
|
Measurement 1 (a) |
Measurement 2 (b) |
Measurement 1 © |
Measurement 2 (d) |
|
|
Saturation (%) |
93.2±2.78 |
97.34± 1.47%* |
87.88±6.87 |
96.38±1.74 |
|
Heart rate (beats per min) |
89.3± 7.6 |
99.94 ±31.18 |
||
|
Respiration rate (per minute) |
20.03± 2,35 |
21.8± 3.97 |
||
|
Body temperature (t°C) |
36.86±0.67 |
36.95±0.86 |
||
|
Haemoglobin (g/l) |
130.79±16.8 |
126.71±16 |
146.3 ±20.26 |
135.6±16.6 |
*p < 0.05 between a и b
In patients with confirmed COVID, the average saturation values were 93.2±2.78%, and at discharge significantly increased to 97.34±1.47%. At admission, the patients were found to have shortness of breath, number of respiration movements per minute 20.03±3.04 per minute, which was accompanied by tachycardia up to 89.84±7.6 beats/min. The body temperature was sub- febrile, 36.86±0.67 °C. Serum hemoglobin level is 130.79±16.8 g/l, and at discharge 126.71±16 g/l. In patients with negative COVID, the mean saturation values were 87.88±6.87%, and at discharge it significantly increased to 96.38 ± 1.74%. At admission, the patients were found to have shortness of breath, 21.03±3.97, which was accompanied by tachycardia up to 99.94±31.18 beats/min. The body temperature was subfebrile, 36.95±0.86 ° C. Serum hemoglobin level was 146.3±20.26 g / l, and at discharge 135.6±16.6 g /L. The difference between the groups was insignificant (p≤0.01), except for the saturation index. Table 3 presents the data of the general blood test (GBT). It is noteworthy that at admission, patients with COVID infection had leukocytosis of 8.9±2.65 x 109 per ml, which significantly decreased to 7.31±4.05 x 109 (p≤0.01), monocytosis 8.26±2.81%, which decreased from 4.82±2.31% after 8-10 days.
Table 3:Laboratory data: blood counts and blood biochemisrty
|
Groups |
Group 1 |
COVID + |
Group 2 |
Control |
|
|
Number of patients |
n=32 |
n=15 |
|||
|
Measurements |
Units |
Measurement 1a |
Measurement 2b |
Measurement 1c |
Measurement 2d |
|
Haemoglobin |
g/L |
130.79±16.8 |
126.71±16 |
146.3 ±20.26 |
135.6±16.6 |
|
Erythrocytes |
109/L |
4.46±0.5 |
4.28±0.66 |
4.91±0.69 |
4.52±0.7 |
|
Leucocytes |
103/L |
8.26±2.81 |
4.82±2.31* |
10.11±4.14 |
11.11±3.48¶ |
|
Monocytes |
% |
8,9±2,65 |
7.31±4.05* |
7.72±7.16 |
8.25±5.13 |
|
Lymphocytes |
% |
23.075±14.38 |
22.31±11,89 |
16.41±11,43 |
20.93± 12.59 |
|
ESR |
mm/h |
18.89± 11,31 |
19.61± 13,33 |
24.71±17.91 |
21.55±16.5 |
|
Thrombocytes |
109/L |
311.32±108,6 |
197.36±76.09* |
258.41±73.95 |
289.21±75.91¶ |
|
CRP |
mg/L |
42.945±47.2 |
12.46±14.36* |
65.84±60.57 |
34.11±31.51* |
|
Blood protein |
mmol/L |
62.72±9.06 |
63.82±12.62 |
66.74± 17.91 |
56.13 ±19.72 |
|
Urea |
mmol/L |
6.855±2.77 |
6.35±2.73 |
5.84 ±2.19 |
6.45± 2.47 |
|
Creatinine |
mmol/L |
91.31±23.67 |
72.01±17.87* |
72.83± 21.51 |
64.64 ±19.9 |
|
Prothrombin time |
seconds |
14.42±2.54 |
13.36±1.61 |
27.90± 29.06 |
20.97± 17.2*¶ |
|
Prothrombin index |
% |
90,7 ±18.7 |
95.2± 14.4 |
83.97 ±35.02 |
107.73 ±28.39 |
|
Glucose |
mg% |
7.3 ±2.5 |
7.17± 4.87 |
7.75±3.49 |
7.98±5.00 |
*p < 0,05 between и b, ¶*p < 0,05 between a, B и c, d
In the control group without COVID, leukocytosis was 10.11±4.14 x 109/ ml, which is significantly higher than in patients of the first group, and at discharge 11.11±3.48 x 109/ ml, which is explained by the resolution stage. Monocytosis was higher in patients with COVID pneumonia than in the control, 8.9±2.6% and 7.72±7.16%, respectively. At discharge in patients of the first group, monocytosis significantly decreased by 7.31±4.05%, and in patients of the control group it remained high at 8.25±5.13%. This indicates the pleocytosis observed in sepsis in the group of COVID-positive patients, C-reactive protein (CRP) in most patients during hospitalization was high and significantly decreased at discharge, 42.95±47.2 mmol/L and 12.46±14.36 mmol/L (p≤0.05). In the group of COVID-negative patients with CRP, there were 65.84±60.57 and 34.11±31.51 mmol/L (p≤0.05) pneumonia [5].
The patients showed a tendency to an increase in the level of creatinine, which decreased at discharge, 91.31±23.67 mmol/L and 72.01±17.87 mmol/L (p≤0.01), respectively, in the first group, and 72.83±21.51 mmol/L and 64.64±19.9 mmol/L, in the control group. In patients of the first group, the prothrombin time at hospitalization was 14.42±2.54 sec., and at discharge 13.36±1.61 sec., which in patients of the control group was 27.90±29.06 sec. and 20.97±17.2 sec., respectively (difference between groups p≤0.01). This may indicate a thrombotic orientation in patients with COVID, in the absence of such in the control group.
It is possible that this fact was responsible for the rapid recovery of the initially lower oxygen saturation in patients with COVID with the standard treatment of community-acquired (non- COVID pneumonia). Platelets were increased in patients with COVID 311.32 ± 108.6 x 109 per liter at the beginning and decreased at discharge 197.36 ± 76.09 x 109 per liter. In the control group at admission 258.41 ± 73.95 and 289.21 ± 75.91 x 109 per liter at discharge.
In general, this may be a consequence of kidney overload, due to the accompanying COVID-19 lesion of the vascular wall and thickening of the blood, since the platelet level in most patients was elevated upon admission. Probably, the patients had transient changes in blood flow in the renal arteries, as a manifestation of disseminated intravascular coagulation (DIC) syndrome. At the end of treatment, platelets decreased, which is a consequence of the use of direct and indirect anticoagulants.
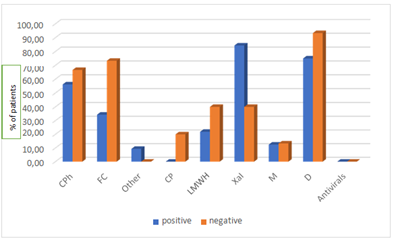
Diagram 1 presents an analysis of the therapy. The absence of antiviral treatment is noteworthy, although blood counts indicate a predominantly viral lesion in viral pneumonia. In patients with pneumonia (PCR negative), antibiotics agents, as cephalosporins and fluoroquinolones were reliably used more often, and dexamethasone was prescribed reliably more often, most likely in the complex treatment of the bronchitic component of bronchopneumonia. Patients with PCR- positive COVID pneumonia were significantly more likely to receive Hageman factor inhibitors.
CPh - cephalosporin, PC - fluoroquinolones, others, others, CP - carbopenicillins, NIG - low molecular weight heparins, Xa - Hageman factor inhibitors, M - methylprednisolone, DM – dexamethasone. Positive – COVID PCR positive, negative – COVID PCR negative.
Due to the severity of the clinical course, as well as the prevention of bacterial complications against the background of COVID, as well as in the group without confirmed COVID, the patients were prescribed several antibacterial drugs of different pharmacological groups, namely cephalosporins, fluoroquinolones, and carbopinems. All patients underwent anticoagulant therapy, fccjrding to approved clinical protocol, with two groups of agents, direct and indirect, as low molecular weight heparins and factor Xa inhibitors.
4. Conclusion
The presented sample of patients with confirmed COVID-19 pneumonia by PCR and CT methods consisted mainly of elderly women with concomitant pathology in the form of hypertension, ischemic heart disease, less often type 2 diabetes. Clinical and laboratory data in the groups were similar at admission. Initially, blood leukocytosis and saturation were lower in the control group (COVID-negative), but later on saturation quickly returned to normal, primarily under the influence of effective antibacterial therapy. But the leukocytosis was still retained (after 10 days). Clotting values (prothrombin time) were higher in patients with confirmed COVID, which required more intensive antithrombotic therapy. In general, in the studied cohort of patients over 65 years old, women (%) with background pathology predominated. With confirmed COVID, the severity was due to an increased tendency to coagulation, with a moderate general inflammatory syndrome (leukocytosis).
And in non- COVID patients, the severity is due to the general inflammatory syndrome against the background of the bacterial nature of the process, with a lesser tendency to hypercoagulability. There were no unfavorable outcomes or transfers to mechanical ventilation in the study cohort. Our data are consistent with literature data [7] that women have a more favorable outcome of COVID with timely massive anticoagulant therapy. In general, their disease was difficult, with the development of polysegmental pneumonia, moderate disseminated intravascular coagulation syndrome was noted, however, against the background of complex therapy with anticoagulants and antibiotics, the disease was controlled, which made it possible to avoid vascular accidents and the development of multiple organ failure.
List of abbreviations:
AH – arterial hypertension; BP - blood pressure; CAP - community-acquired pneumonia; CPh - cephalosporin, DIC - disseminated intravascular coagulation; DM type 2 - diabetes mellitus; DM – dexamethasone; IHD - ischemic heart disease, CP – carbopenicillins; NA – non applicable; NIG - low molecular weight heparins; M – methylprednisolone; KazNMU – Kazakh national medical university; PCR – polymerase chain reaction; PC – fluoroquinolones; RR respiration rate Xa - Hageman factor inhibitors.
Declarations
Ethics approval and consent to participate. All human data analysis was done under the Approval of the Local Ethical Commission of the KazNMU named after S.D. Asfendiyarov (#968 from 23/10/20). Consent for publication. Authors agree with the publishing policy of the Pneumonia as stated in the Editorial Policy.
Availability of data and Materials
Authors will provide any additional data and materials as following the Editorial Policy of Pneumonia.
Competing interests:
Authors declare no competing interest issues either financial and non-financial.
Funding:
GE, LI, TM were supported by a grant of Ministry of Science of Kazakhstan (N00 AP09561834) granted towards TM.
Authors contributions:
GE collected and analyzed the data, LI analyzed the data and wrote the paper, TA provided the grant support, corrected the paper and analyzed the data.
Acknowledgements:
The authors thank KazNMU named after S.D. Asfendiarov for support in the studies.
References
- Popova A, Yu, et al. Features of Etiology of Community-Acquired Pneumonia Associated with COVID-19. Problemy Osobo Opasnykh Infektsii [Problems of Particularly Dangerous Infections] 4 (2020): p99.
- Amy H Attaway, Rachel G Scheraga, Adarsh Bhimraj, Michelle Biehl, Umur Hatipoglu. Severe covid-19 pneumonia: pathogenesis and clinical BMJ 372 (2021): n4.
- Hidesaku Asakura, Haruhiko Ogawa. COVID-19-associated coagulopathy and disseminated intravascular coagulation Int J Hematol 7 (2020): 1–13.
- Nguyen P-Y, Chen XJ and Kunasekaran M. Rise in pneumonia cases of unknown aetiology in Kazakhstan in June 2020: a rapid analysis. Global Biosecurity 2 (2020).
- Joshua David Farkas. The complete blood count to diagnose septic shock. J Thorac Dis 12 (2020): S16–S21.
- Pickering JW, Ralib AM, Endre ZH. Combining creatinine and volume kinetics identifies missed cases of Acute Kidney Injury following Cardiac Arrest // Critical Care 17 (2013): R7.
- Cristina Mussini, Alessandro Cozzi-Lepri, Marianna Menozzi, Marianna Meschiari, Erica Franceschini, et al. Covid-19 Working Group (MoCo19). Better prognosis in females with severe COVID-19 pneumonia: possible role of inflammation as potential mediator Clin Microbiol Infect 27 (2021): 1137-1144.


 Impact Factor: * 6.2
Impact Factor: * 6.2 Acceptance Rate: 76.33%
Acceptance Rate: 76.33%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 