Beta-Blockers and Antidepressants: Contributions to Municipal Wastewaters from Hospitals and Residential Areas
Edward A McBean1,2, Hamid Salsali3, Munir A Bhatti2*, Jinhui Jeanne Huang1
1Sino-Canada R&D Centre on Water and Environmental Safety, Nankai University, Tianjin, China
2School of Engineering, University of Guelph, Ontario, Canada
3EnvPower, Waterloo, Ontario, Canada
*Corresponding Author:Munir A Bhatti, School of Engineering, University of Guelph, N1G 2W1 Guelph, Ontario, Canada, Tel: (1)519-591-0720;
Received: 11 May 2018; Accepted: 16 August 2018; Published: 15 October 2018
Article Information
Citation: Edward A McBean, Hamid Salsali, Munir A Bhatti, Jinhui Jeanne Huang. Beta-Blockers and Antidepressants: Contributions to Municipal Wastewaters from Hospitals and Residential Areas. Journal of Environmental Science and Public Health 2 (2018): 144-159.
View / Download Pdf Share at FacebookAbstract
Emerging contaminants in wastewater are of increasing concerns due to identification of previously undetected chemicals now being identified in wastewater treatment plant (WWTP) effluents, and subsequently, in surface waters. This paper provides monitoring results for selected beta-blockers (atenolol, sotalol, metoprolol, and propranolol) and antidepressants (venlafaxine, o-desmethylvenlafaxine, citalopram, desmethyl citalopram and carbamazepine) hospitals and residential neighborhoods in three different cities of Ontario, Canada. The average concentrations of compounds studied were determined for atenolol, metoprolol, propranolol and sotalol from the hospitals were 1291 ng/L, 848 ng/L, 71 ng/L and 274 ng/L respectively. The average observed concentrations of venlafaxine, o-desmethyl venlafaxine, citalopram and desmethyl citalopram from the hospitals were 1756 ng/L, 2878 ng/L, 650 ng/L and 356 ng/L respectively. The results show significant variability in the concentrations of beta-blockers and antidepressants from hospital to hospital. Results comparing these hospital effluents to wastewater treatment plant influents show that hospitals, on average, contributed 0.87% of the total load for the indicated emerging contaminants, with a range from hospitals varying between 0.25% and 1.79%. The findings also include the effects of short hospital stays indicate patients taking pharmaceuticals at home, as being evident from the monitoring results. Ninety-five percent upper confidence limits for individual beta blockers and anti-depressants are provided, as computed from available technical literature and monitoring results from this research, as a means of providing reasonable upper bounds on the magnitudes of the individual compounds.
Keywords
Emerging contaminants; Pharmaceuticals; Beta-blockers; Antidepressants; Municipal wastewater; Hospitals; Residential neighborhoods; Sewerage system; Source load allocation; Characterization of wastewater
Article Details
1. Introduction
Emerging contaminants such as pharmaceuticals and personal care products are receiving increased attention as researchers study their occurrence in the environment and their effects on living organisms [1-9]. In a search to find the point(s)-of-entry for these contaminants into the natural environment, scientists are routinely led to municipal wastewater treatment plant effluents. To improve the understanding of the source characteristics of these compounds within the overall wastewater system, this research focused on two classes of pharmaceuticals, namely beta-blockers and antidepressants, and from two different source types i.e., hospitals and residential areas. Beta-blockers and antidepressants are medications prescribed by medical professionals to treat a variety of conditions as discussed below.
Beta-blockers, or beta-adrenergic blocking agents, are a class of pharmaceuticals first developed in the late 1950s. One of the most commonly used beta-blockers is propranolol, which revolutionized the treatment of angina [10]. Beta-blockers are designed to inhibit the action of beta-adrenergic receptors that are part of the central nervous system. When these receptors are hindered, the result is a dilation of blood vessels, slowing of the heart rate, and opening of bronchi in the lungs [11]. Beta-blockers are therefore known to have an antihypertensive effect and are used to treat individuals with high blood pressure as well as to treat patients after heart attacks. The four beta-blockers considered in this study are atenolol, sotalol, metoprolol, and propranolol.
Antidepressants are a class of pharmaceuticals that affect neurotransmitters, the chemicals that nerves within the brain use to communicate with each other. Examples of neurotransmitters include serotonin, dopamine and norepinephrine. It is thought that an imbalance in these neurotransmitters is the cause of depression and also may play a role in anxiety. Antidepressants are believed to work by inhibiting the release, or affecting the action of, neurotransmitters. The antidepressant compounds evaluated in this study are venlafaxine, o-desmethylvenlafaxine, citalopram, desmethyl citalopram and carbamazepine. Venlafaxine is a serotonin-norepinephrine reuptake inhibitor (SNRI) prescribed for the treatment of depression, depression with associated symptoms of anxiety, generalized anxiety disorder, social anxiety disorder and adult panic disorder. O-desmethylvenlafaxine, a major active metabolite of venlafaxine, also functions as an SNRI. It is also synthetically produced (desvenlafaxine) and was approved by Health Canada in 2009 for treatment of depression. Citalopram is a selective serotonin reuptake inhibitor (SSRI) prescribed for the management of depression as well as treating obsessive-compulsive disorder, panic disorder, premenstrual dysphoric disorder, anxiety disorder and post-traumatic stress disorder. Desmethyl citalopram, an active metabolite of citalopram, also functions as an SSRI. Carbamazepine is used to treat seizures and nerve pain such as trigeminal neuralgia and diabetic neuropathy. The above-named compounds were selected from a review of the technical literature, as representatives of these two types of sources in relation to beta-blockers and antidepressants(e.g. anti-depressants as reported in the Great Lakes by Metcalfe et al. [12] as venlafaxine, o-desmethyl venlafaxine, citalopram, desmethyl citalopram, fluoxetine, norfluoxetine, o-desmethyl venlafaxine, bupropion, sertraline, desmethyl sertraline, and paroxetine, by Spongberg et al. [13] as carbamazepine and beta-blocker as reported by Lee as acebutolol, atenolol, sotalol, metoprolol, and propranolol.
Once in the natural environment, these compounds interact with aquatic organisms where beta-blockers and antidepressants have been found in the tissues of fish [14-15]. The emerging contaminant types referred to above have been found in wastewater treatment influents around the world [1-3, 16-17] although there have been only a relatively few studies which have attempted to classify the sources of these pharmaceuticals. Of the work that has been done to classify the sources of pharmaceutical contaminants, hospitals have been a primary focus. The intense issue of contributions from hospital sources from within city environs has been assessed in recent studies [8-9, 18-23], which demonstrate great interest in the need for source control. As it turns out, the results from hospitals and residential areas vary widely from location to location. The average predicted with audit data (Caboolture, Queensland, Australia) showed that atenolol and metoprolol from hospital effluents were reported to account for source load allocations of 0.6% and 2.3% of the total loading in the WWTP influent respectively. Similarly, citalopram, and venlafaxine and hospitals were found to be 1.6%, and 2%, respectively [24].
The aim of the study is to improve characterization of the sources of these compounds being released into wastewaters to help decision makers assess alternative removal strategies of pharmaceuticals. Assessments of findings as a result of the sampling undertaken in this study are described below and comparisons provided to data reported in the technical literature.
2. Methods
Monitoring results from three different municipalities in southwestern Ontario were obtained and will be referred to as cities A, B, and C. The sewers referred to herein carry only sanitary flows, and are not combined sewers.
2.1 Sampling protocols
The sampling locations were selected to best study the sources of pharmaceuticals into municipal wastewater sewerage systems. Hospitals and residential neighbourhoods were chosen at locations from where beta-blockers and antidepressants enter into the wastewater network (not combined sewers). Sampling was completed using 24-hour composites, with five samples taken for hospitals A, B and C, two samples were obtained from Residential Area A, and ten samples were taken from Residential Area B. As well, five samples were obtained from influent to City-B wastewater treatment plant and three samples were taken from influent to City-C wastewater treatment plant, to characterize concentrations in wastewater.
2.2 Sampling locations
Samples were obtained from manholes carrying just hospital wastewater, from manholes servicing residential neighborhoods, and from the inlets to wastewater treatment plants, where all samples were collected by municipal staff. At each location, three liters of sample were collected and split into two amber glass bottles and one HDPE bottle before they were stored at 4oC until analysis. Analytical work was completed at the Worsfold Water Quality Centre at Trent University. Table 1 describes the sampling locations within each city.
City |
Sampling location |
A |
Residential Area (800,000 inhabitants), Hospital (250 beds) |
B |
Two Residential Areas (712,575 inhabitants), Hospital (1200 beds), Treatment Plant Influent (Inflow (293 ML/day) |
C |
Hospital (250 beds), Treatment Plant Influent (Inflow (87.5 ML/day) |
Table 1: Sampling Locations.
2.3 Analysis
The samples were filtered, acidified, and then extracted using Waters Oasis MCX solid phase extraction cartridges. The extracts were subsequently preconditioned with acetone, methanol, and dilute sulphuric acid before being eluted from the cartridge with ammonium hydroxide in methanol. They were then evaporated to almost dryness and reconstituted in methanol. ?-Blockers and antidepressants were extracted from water samples using the method described in Metcalfe et al. [12]. Samples of 500 mL were decanted, adjusted to pH 2.5 to 3 with H2SO4, spiked with isotopically labelled standards and extracted using Waters Oasis MCX cartridges (6cc, 150 mg). Cartridges were conditioned with 6 mL of acetone, 6 mL of methanol and 6 mL of milli-Q water at pH 2.5 to 3. Samples were passed through the cartridges at a rate of approximately 5 mL/min. Analytes were eluted using three aliquots of 5% NH4OH in methanol. For Quality Analysis and Quality Control, a laboratory blank for each sample batch and at least one duplicate from each sample set from the same sampling location was tested. Also, surrogate standards were added to each sample to monitor and corrected for any potential loss during sample analysis.
3. Results
At each sampling location, the concentrations of beta-blockers and antidepressants were characterized. Figures 1 to 4 show the concentrations of each compound at the various source locations. The box plots (a.k.a. box and whisker diagram) follow standardized protocols based on the five numbers: summary: minimum, first quartile, median, third quartile, and maximum. In the simplest box plot, the central rectangle spans the first quartile to the third quartile (the interquartile range or IQR). A segment inside the rectangle shows the median and "whiskers" above and below the box show the locations of the minimum and maximum.
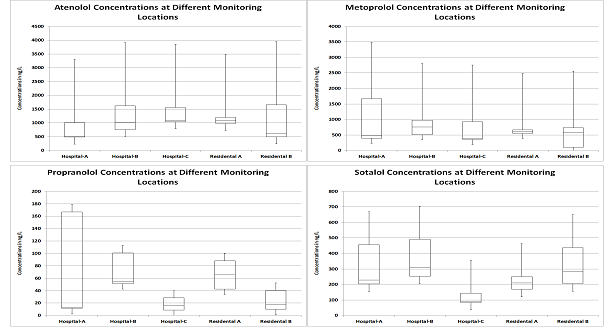
Figure 1(a): Atenolol Concentrations at Different Monitoring Locations (top left); (b): Metoprolol Concentrations at Different Monitoring Locations (top right); (c): Propranolol Concentrations at Different Monitoring Locations (bottom left); (d): Sotalol Concentrations at Different Monitoring Locations (bottom right).
4. Discussion
4.1 Source concentrations
The beta-blocker concentrations as seen in Figures 1(a), 1(b), 1(c) and 1(d) show where atenolol concentrations range from 236 ng/L to 3300 ng/L, metoprolol concentrations range from 220 ng/L to 3,490 ng/L, propranolol concentrations range 2.5 ng/L to 234 ng/L and sotalol concentrations range from 49 ng/L to 920 ng/L in hospital effluents and in the residential areas, atenolol concentrations range from 325 ng/L to 2480 ng/L, metoprolol concentrations range from 84 ng/L to 959 ng/L, propranolol concentrations range from 4.2 ng/L to 127 ng/L, and sotalol concentrations range from 18 ng/L to 750 ng/L.
All the selected beta blockers (atenolol, metoprolol, propranolol and sotalol) were detected in all the samples from the three hospitals. The maximum concentrations observed for atenolol and metoprolol were 3,300 ng/L and 3,490 ng/L, and both were observed in hospital-A while for the propranolol and sotalol, the maximums were 234 ng/L and 920 ng/L, and both were observed in hospital-B. Among the beta blockers, the average concentrations detected for atenolol were 1106, 1408 and 1360 ng/L for hospital-A, hospital-B and hospital-C, respectively. The average concentrations detected for metoprolol were 1253, 703 and 587 ng/L for hospital-A, hospital-B and hospital-C, respectively. The average concentrations detected for propranolol were 75, 110, and 27 ng/L for hospital-A, hospital-B and hospital-C, respectively. The average concentrations detected for sotalol were 343, 157 and 121 ng/L for hospital-A, hospital-B and hospital-C respectively. Generalizing the results from the above findings, the metoprolol, atenolol, and sotalol concentrations are similar across the range of monitoring locations suggesting that no location was consistently a distinct point source of beta-blockers to wastewaters. Due to the long-term nature of use of beta-blocker prescriptions for conditions such as hypertension, individuals are likely to consume a large percentage of beta-blockers at home, leading to similar concentrations in residential effluent.
Of the antidepressants studied, as shown in Figures 2(a), 2(b), 3(a), 3(b) and 4, venlafaxine and o-desmethyl venlafaxine show the highest concentrations at hospital A. Residential area A shows the second highest concentration whereas all monitoring locations in Residential Areas B and C are much lower. Citalopram and desmethyl citalopram exhibit more consistent concentrations across the range of monitoring locations with hospital A recording the highest levels.
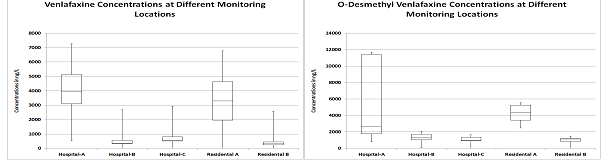
Figure 2: (a): venlafaxine Concentrations at Different Monitoring Locations (left); (b): O-desmethyl venlafaxine Concentrations at Different Monitoring Locations (right).
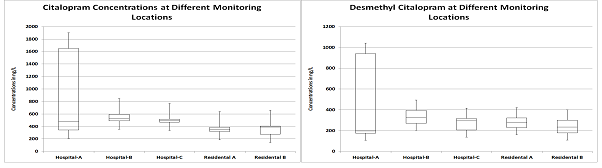
Figure 3: (a): Citalopram Concentrations at Different Monitoring Locations (left) and Figure (b): desmethyl citalopram Concentrations at Different Monitoring Locations (right).
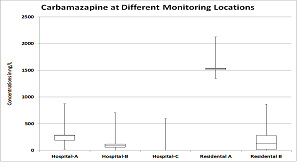
Figure 4: Carbamazepine Concentrations at Different Monitoring Locations.
In the antidepressant class, venalfaxine, o-desmethyl venlafaxine, citalopram and desmethyl citalopram were detected in all the samples from the three hospitals while carbamazepine has 100% detection rate in hospital-A and hospital-B and 20% detections in hospital-C. O-Desmethyl venlafaxine has the highest concentration of 11,700 ng/L in hospital-A. The maximum concentrations of venalfaxine, citalopram, desmethyl citalopram and carbamazepine were 7.260 ng/L, 1,900 ng/L, 1,041 ng/L and 873 ng/L and all from hospital A. The average concentrations detected for venlafaxine were 3,998, 543 and 727 ng/l for hospital-A, hospital-B and hospital-C respectively. The average concentrations detected of o-desmethyl venlafaxine were 5.671, 1,647, and 1,316 ng/l hospital-A, hospital-B and hospital-C respectively. The average concentrations detected of citalopram were 917, 538 and 494 ng/l for hospital-A, hospital-B and hospital-C, respectively. The average concentrations of desmethyl citalopram detected were 491, 329 and 249 ng/l for hospital-A, hospital-B and hospital-C, respectively. The average concentrations of carbamazepine detected were 331, 234 and 18 ng/l for hospital-A, B and C respectively.
Where venlafaxine concentrations range from 320 ng/L to 7260 ng/L, o-desmethyl venlafaxine concentrations range from 672 ng/L to 11,700, citalopram concentrations range from 210 ng/L to 1900 ng/L, desmethyl citalopram concentrations range from 88 ng/L to 1040 ng/L, and carbamazepine concentrations from 8 ng/L to 873 ng/L. In residential areas, venlafaxine concentrations range from 59 ng/L to 5970 ng/L, o-desmethyl venlafaxine concentrations range from 554 ng/L to 6160 ng/L, citalopram concentrations range from 128 ng/L to 542 ng/L, desmethyl citalopram concentrations range from 105 ng/L to 368 ng/L, and carbamazepine concentrations range from 8 ng/L to 1547 ng/L. Overall, none of the pharmaceutical classes in this study show the same source characteristics across the two alternative source types. Variability is evident from one hospital to another, and from residential areas, indicating that no one sample location type contributes consistently more contaminant per litre than the others.
4.2 Hospital loadings
The total loading of each compound within hospital effluents was estimated as follows: using an average wastewater per hospital bed of 1350L/bed/day [9] the hospital loadings were calculated and compared to loading levels at the WWTP influents.
As seen in Table 2, contaminant loadings from the hospitals are responsible for less than 0.9% of the overall loading for the various pharmaceuticals in the wastewater treatment plant influent. The individual loadings of the compounds i.e. atenolol, sotalol, desmethyl citalopram, venlafaxine, O-desmethyl venlafaxine and carbamazepine were less than 1.0 % of the overall loading from both the hospitals (hospital-B and hospital-C). Hospital-B overall loading for metoprolol, propranolol and citalopram were less than 1.8% whereas in hospital C, the overall loading of these three compounds were less than 1%. Results show that hospitals in city-B, on average, contribute 0.87% of the total load with a range from a hospital varying between 0.25% and 1.79% while hospitals, on average, contribute 0.49% of the total load with a range from a hospital varying between 0.04% and 0.86% in city-C. The total loadings of all the nine selected compounds from hospital-B were 0.87% whereas for hospital-C was 0.49%.
Beta Blockers |
Hospital B Effluent |
WWTP B Influent |
Percent from Hospital, City B |
Hospital C Effluent |
WWTP C Influent |
Percent from Hospital, City C |
Atenolol |
2.28 |
251.55 |
0.91 |
0.46 |
64.93 |
0.71 |
Sotalol |
0.58 |
115.63 |
0.50 |
0.04 |
21.63 |
0.19 |
Metoprolol |
1.14 |
94.56 |
1.21 |
0.20 |
23.05 |
0.86 |
Propranolol |
0.18 |
9.95 |
1.79 |
0.01 |
2.00 |
0.46 |
Citalopram |
0.87 |
81.56 |
1.07 |
0.17 |
23.72 |
0.70 |
Desmethyl Citalopram |
0.53 |
62.28 |
0.86 |
0.08 |
16.91 |
0.50 |
Venlafaxine |
0.88 |
143.70 |
0.61 |
0.25 |
47.21 |
0.525 |
O-Desmethyl Venlafaxine |
2.67 |
370.56 |
0.72 |
0.44 |
112.06 |
0.40 |
Carbamazepine |
0.15 |
58.60 |
0.25 |
0.01 |
13.66 |
0.04 |
Table 2: Hospital Loadings and Percentages.
Ort et al. [24] reported that in the town of Caboolture, Queensland, Australia, beta- blockers (metoprolol and atenolol) contributed 4.1% and 1.8% respectively to the municipal wastewater treatment system and anti-depressants citalopram and venlafaxine contributed 4% and 2%, respectively, to the municipal waste water treatment system. As Ort et al. [24] report hospitals do not account for a disproportionate amount of total mass loading for the majority of pharmaceutical compounds found in municipal wastewater. Kleywegt et al. [9] reported that atenolol, metoprolol, propanolol, citalopram, and venlafaxine which were detected in hospital effluents, individually contributed less than 1 % of the total load to the receiving wastewater treatment plant in a large urban sewershed in Ontario, Canada. In a municipality such as City B where there are multiple hospitals, the loadings per bed as calculated for Hospital B were extrapolated over the 1200 hospital beds throughout the City to estimate the loading percentages due to hospitals, in general. This yielded values of 0.89% for all beta-blocker while antidepressants were 0.71%.
Given the above, the results indicate the current trend in the healthcare sector towards short hospital stays and early discharge times infers patients are taking pharmaceuticals at home, resulting in the pharmaceuticals being excreted into the wastewater system sourced from residential neighborhoods. The two selected classes of pharmaceuticals are not typically administered at a hospital: see for instance, the recent book by Verlichhi [25]-Hospital wastewater Characteristics, Management, Treatment and Environmental Risks, resulting in the hospitals loadings not being so high. The monitoring results of this study in relation to hospital wastewater from the technical literature for the selected beta-blockers and antidepressants are comparable as shown in Table 3, for atenolol of the beta-blockers group, and for venlafaxine for the antidepressants group.
Source of Data |
Atenolol |
Metaprolol |
Propranol |
Sotalol |
Venlafaxine |
Citalopram |
Carbamazepine |
Al Aukidy, et al. [26] |
- |
- |
- |
- |
- |
- |
82.5 |
Alrhmoun [27] |
1500 |
100 |
- |
2300 |
- |
- |
- |
Alrhmoun et al. [28] |
- |
- |
- |
- |
- |
- |
390 |
Boillot et al. [29] |
3400 |
25000 |
- |
- |
- |
- |
- |
Chonova et al. [23] |
2800 |
- |
1500 |
- |
- |
- |
300 |
Corre KSL, et al. [19] |
- |
- |
- |
- |
- |
- |
850 |
Cruz-Moratoa, et al. [30] |
- |
- |
- |
- |
- |
- |
441 |
DHI [31] |
- |
- |
- |
- |
484 |
- |
- |
Galletti et al. [32] |
- |
- |
- |
- |
- |
- |
956 |
Galletti, A. [33] |
5131 |
928 |
60 |
4751 |
- |
- |
956 |
Gomez et al. [34] |
3400 |
- |
1350 |
- |
- |
- |
40 |
Haq et al. [8] (Hospital-1) |
- |
417 |
- |
- |
643 |
- |
75 |
Haq et al. [8] (Hospital-2) |
- |
152 |
- |
- |
4570 |
- |
401 |
Klancar et al. [35] |
- |
- |
- |
- |
- |
- |
194 |
Kleywegt et al. [9] (Hospital-1) |
862 |
299 |
3.9 |
- |
366 |
201 |
295 |
Kleywegt et al. [9] (Hospital-2) |
2740 |
2230 |
68.4 |
- |
522 |
426 |
119 |
Kleywegt et al. [9] (Hospital-3) |
1420 |
393 |
43 |
- |
425 |
501 |
233 |
Kovalova et al. [18] |
2315 |
1325 |
116 |
700 |
811 |
- |
235 |
Lin et al. [36] |
- |
54 |
54 |
- |
- |
- |
- |
Mendoza et al. [37] |
- |
- |
- |
235 |
- |
- |
- |
Møller [38] |
- |
- |
- |
- |
2700 |
- |
129 |
Mullot et al. [39] |
3400 |
- |
- |
- |
- |
- |
- |
Nagarnaik et al. [40] |
3166 |
- |
- |
- |
- |
- |
- |
Nielsen et al. [41] |
180 |
3700 |
- |
- |
- |
- |
- |
Qarni et al. [42] |
730 |
- |
- |
- |
- |
- |
- |
Santos et al. [20] |
2628 |
59.9 |
98.9 |
89.1 |
545 |
- |
- |
Santos et al. [20] (Hospital-1) |
- |
- |
- |
- |
- |
110 |
- |
Santos et al. [20] (Hospital-2) |
- |
- |
- |
- |
- |
58.3 |
- |
Santos et al. [20] (Hospital-3) |
- |
- |
- |
- |
- |
196 |
- |
Santos et al. [20] (Hospital-4) |
- |
- |
- |
- |
- |
145 |
- |
Santos et al. [20] (General hospital ) |
- |
- |
- |
- |
- |
- |
771 |
Santos et al. [20] (Maternity hospital) |
- |
- |
- |
- |
- |
- |
2995 |
Santos et al. [20] (Pediatric hospital ) |
- |
- |
- |
- |
- |
- |
650 |
Sim et al. [43] |
- |
- |
- |
- |
- |
- |
1920 |
This Study (Hospital-1) |
1106 |
1253 |
1253 |
343 |
3998 |
917 |
331 |
This Study (Hospital-2) |
1408 |
703 |
708 |
357 |
519 |
538 |
234 |
This Study (Hospital-3) |
1360 |
587 |
704 |
121 |
582 |
494 |
18 |
Thomas et al. [44] |
- |
5811 |
- |
- |
- |
- |
- |
Verlicch et al. [45] |
- |
1100 |
85 |
5100 |
- |
- |
- |
Verlicchi et al. [45] (Hospital B (winter)) |
- |
- |
- |
- |
- |
- |
970 |
Verlicchi et al. [45] (Hospital B (summer)) |
- |
- |
- |
- |
- |
- |
730 |
Verlicchi et al. [46] |
5800 |
- |
- |
- |
- |
- |
|
Yuan et al. [21] |
- |
- |
- |
- |
- |
- |
88 |
Table 3: Average Hospital Waste Water Concentrations from Technical terature for the Selected Beta-Blockers and Antidepressants.
Given the above variabilities in Table 3, the following is evident: monitoring results show significant variability from one hospital to another. Some hospitals are 'Cancer' hospitals, for example, and hence this has substantial influence on which pharmaceuticals are being employed. To provide characterization of reasonable maximum average concentrations for hospitals, as derived from combinations of the technical literature and this study, concentration data were combined to estimate the 95% upper confidence limits of the concentrations for the various beta-blockers and antidepressants. The statistical software developed by USEPA (ProUCL) for environmental applications for data sets with, and without, non-detect, was utilized. The ProUCL software is based upon the philosophy that rigorous statistical methods can be used to compute estimates of population parameters and decision-making statistics including: the upper confidence limit (UCL) of the mean, the upper tolerance limit (UTL), and the upper prediction limit (UPL) to help decision-makers and project teams in making priority decisions. Version 5.0.00 of this software was used. The upper confidence limits (UCL) for the means were completed by using the appropriate distributions as listed in Table-4.
Analyte |
Recommendation for Use by ProUCL |
Concentration at Upper 95% Confidence Interval |
Atenolol |
Use 95% Approximate Gamma UCL |
3,005 |
Metoprolol |
Use 95% Adjusted Gamma UCL |
4,032 |
Propranolol |
Use 95% Chebyshev (Mean, Sd) UCL |
587 |
Sotalol |
Use 95% Adjusted Gamma UCL |
3,885 |
venlafaxine |
Use 95% Chebyshev (Mean, Sd) UCL |
2,729 |
Citalopram |
Use 95% Student's-t UCL |
513 |
Carbamazepine |
Use 95% Approximate Gamma UCL |
813 |
Table 4: 95% UCL for Each of the Beta-Blocker and Antidepressant for Hospitals.
5. Conclusion
Through monitoring of wastewater effluents from hospitals and residential neighborhoods for beta-blockers and antidepressants, the sources of pharmaceuticals in the wastewater at the treatment plant were assessed. It was found that both location types (hospitals and residential areas) within this study contributed relatively equally in terms of concentrations, to the overall loading of the selected pharmaceuticals in wastewaters. When the contributions due to hospitals were compared to the total loading for each compound in the influent to wastewater treatment plants, it was determined that hospitals account for, on average, 0.87%, with a range varying between 0.25% and 1.79% depending on the pharmaceutical, of the mass loadings to the wastewater treatment plant, indicating that health care centers are not straightforward point sources for beta-blockers and antidepressants in terms of inputs to the wastewater treatment system. Comparisons of the monitoring results from the technical literature with the findings from this study demonstrates substantial variability, indicating that no simple procedure will predict beta-blockers and antidepressant concentrations in hospital wastewaters. By aggregating available technical data, in combination with the findings from this study, 95% UCL for average concentration were determined, providing insights as to magnitudes of the individual beta-blockers and antidepressants.
Acknowledgments
We thank NSERC Discovery and the Ministry of Science and Technology, P.R. China (2016YFC0400709) for their research funding. We also thank the three municipalities for their cooperation in the completion of this study. Dan Shaver’s participation in this research is highly appreciated as well.
References
- Smyth SA, Lishman L, McBean E, et al. Fate of Polycyclic and Nitro Musks during Aerobic and Anaerobic Sludge Digestion. International Water Association Journal (2007).
- Smyth SA, Lishman L, McBean E, et al. Polycyclic and Nitro Musks in Canadian Municipal Wastewater: Occurrence and Removal in Wastewater Treatment. Water Quality Research Journal of Canada 42 (2007): 138-152.
- Smyth S, Lishman L, McBean E, et al. Seasonal Occurrence and Removal of Polycyclic and Nitro Musks from Wastewater Treatment Plants in Ontario, Canada. Journal of Environmental Engineering and Science 7 (2008): 299-317.
- Godoy AA, Kummrow F, Pamplin PAZ. Occurrence, Eco toxicological effects and risk assessment of antihypertensive pharmaceutical residues in the aquatic environment-A review. Water Research 115 (2017): 74-83.
- Destrieux D, Laurent F, Budzinski H, et al. Drug residues in urban water: A database for ecotoxicological, risk management. Science of the Total Environment 609 (2017): 927-941.
- Maszkowska J, Stolte S, Kumirska J, et al. Beta-blockers in the environment: Part I. Mobility and hydrolysis study. Science of the Total Environment 493 (2014): 1112-1121.
- Minguez L, Pedelucq J, Farcy E, et al. Toxicities of 48 pharmaceuticals and their freshwater and marine environmental assessment in northwestern France. Environ Sci Pollut Res 23 (2016): 4992-5001.
- Haq MRU, Metcalfe C, Li H, et al. Discharge of pharmaceuticals into municipal sewers from hospitals and long-term care facilities. Water Quality Research Journal of Canada 47 (2012): 140-152.
- Kleywegt S, Pileggi V, Lam YM, et al. The Contribution of Pharmaceutically Active Compounds from Healthcare Facilities to a Receiving Sewage Treatment Plant in Canada. Environmental Toxicology and Chemistry 35 (2016): 850-862.
- Van der Vring JA, Daniels MC, Holwerda NJ. Combination of calcium channel blockers and beta blockers for patients with exercise-induced angina pectoris: a double-blind parallel-group comparison of different classes of calcium channel blockers. The Netherlands Working Group on Cardiovascular Research 50 (1999): 447-454.
- Manger WM, Gifford RW. 100 Questions and Answers about Hypertension. Blackwell Science (2001).
- Metcalfe CD, Chu S, Judt C, et al. Antidepressants and their metabolites in municipal wastewater, and downstream exposure in an urban watershed. Environmental Toxicology and Chemistry 29 (2010): 79-89.
- Spongberg AL, Witter JD. Pharmaceutical compounds in the wastewater process stream in Northwest Ohio. Sci Total Environ 397 (2008): 148-157.
- Brooks BW, Hambliss CK, Stanley JK, et al. Determination of select antidepressants in fish from an effluent?dominated stream. Environmental Toxicology and Chemistry 24 (2005): 464-469.
- Haider S, Baqri SSR. Beta-Adrenoceptor antagonists reinitiate meiotic maturation in Clarias batrachus oocytes. Comp Biochem Physiol Mol Integr Physiol 126 (2007): 517-525.
- Miege C, Choubert JM, Ribeiro L, et al. Fate of pharmaceuticals and personal care products in wastewater treatment plants-conception of a database and first results. Environ Pollut 157 (2009): 1721-1726.
- Wick A, Fink G, Joss A, et al. Fate of beta blockers and psycho-active drugs in conventional wastewater treatment. Water Research 43 (2009): 1060-1074.
- Kovalova L, Siegrist H, Singer H, et al. Hospital Wastewater Treatment by Membrane Bioreactor: Performance and Efficiency for Organic Micropollutant Elimination. Environ Sci Technol 46 (2012): 1536-1545.
- Corre KSL, Ort C, Kateley D, et al. Consumption-based approach for assessing the contribution of hospitals towards the load of pharmaceutical residues in municipal wastewater. Environment International 45 (2012): 99-111.
- Santos LHMLM, Gros M, Rodriguez-Mozaz S, et al. Contribution of hospital effluents to the load of pharmaceuticals in urban wastewaters: Identification of ecologically relevant pharmaceuticals. Science of the Total Environment (2013): 461-462: 302?316.
- Yuan S, Jiang X, Xia X, et al. Detection, occurrence and fate of 22 psychiatric pharmaceuticals in psychiatric hospital and municipal wastewater treatment plants in Beijing, China. Chemosphere 90 (2013): 2520-2525.
- Al-Aukidy MA, Verlicchi P, Voulvoulis N. A framework for the assessment of the environmental risk posed by pharmaceuticals originating from hospital effluents. Science of the Total Environment 493 (2014): 54-64.
- Chonova T, Keck F, Labanowski J, et al. Separate treatment of hospital and urban wastewaters: A real scale comparison of effluents and their effect on microbial communities. Science of the Total Environment 542 (2016): 965-975.
- Ort C, Lawrence MG, Reungoat J, et al. Determining the fraction of pharmaceutical residues in wastewater originating from a hospital. Water research 44 (2010): 605-615.
- Verlichhi P. Hospital Wastewasters-Characteristics, Management, Treatment and Environemtnal Risks. Hdb Env Chem 60 (2018): 1-16.
- Al-Aukidy MA, Verlicchi P, Jelic A, et al. Monitoring release of pharmaceutical compounds: Occurrence and environmental risk assessment of two WWTP ef?uents and their receiving bodies in the Po Valley, Italy. Sci Total Environ 438 (2012): 15-25.
- Alrhmoun M. Hospital wastewaters treatment: Upgrading water systems plants and impact on purifying biomass. Environmental Engineering, Universite de Limoges. English. NNT: 2014LIMO0042 (2014).
- Alrhmoun M, Casellas M, Baudu M, et al. Efficiency of Modified Granular Activated Carbon Coupled with Membrane Bioreactor for Trace Organic Contaminants Removal, World Academy of Science, PhD thesis, Engineering and Technology, International Journal of Chemical, Nuclear, Metallurgical and Materials Engineering 8 (2015): 43-49.
- Boillot C, Bazin C, Tissot-Guerraz F, et al. Daily physicochemical, microbiological and ecotoxicological ?uctuations of a hospital ef?uent according to technical and care activities. Sci Total Environ 403 (2008): 113-129.
- Cruz-Morato C, Lucas D, Llorca M, et al. Hospital wastewater treatment by fungal bioreactor: Removal efficiency for pharmaceuticals and endocrine disruptor compounds. Science of the Total Environment 493 (2014): 365-376.
- DHI. Full scale advanced wastewater treatment at Herlev Hospital, Treatment performance and evaluation, Grundfos BioBooster A/S, Report, May (2016).
- Galletti A, Verlicchi P, Al Aukidy M, et al. Hospital as a source of emerging contaminants (pharmaceutical): Results of an investigation on its ?nal ef?uent chemical characteristics. In: Proceeding of the 12th International Conference of Environmental Science and Technology, Rhodes, Greece (2011).
- Galletti A. Pharmaceutical compounds in waters, Investigations on hospital effluents as a source of environmental contamination and on their treatability, Italy (2010).
- Gomez MJ, Petrovic M, Fernandez-Alba AR, et al. Determination of pharmaceuticals of various therapeutic classes by solid-phase extraction and liquid chromatography-tandem mass spectrometry analysis in hospital effluent wastewaters. Journal of Chromatography A 1114 (2006): 224-233.
- Klancar A, Trontelj J, Kristl A, et al. Levels of pharmaceuticals in Slovene municipal and hospital wastewaters: A preliminary study. Arh Hig Rada Toksikol 67 (2016): 106-115.
- Lin AYC, Tsai YT. Occurrence of pharmaceuticals in Taiwan's surface waters: Impact of waste streams from hospitals and pharmaceutical production facilities. Science of the Total Environment 407 (2009): 3793-3802.
- Mendoza A, Acena J, Perez S, et al. Pharmaceuticals and iodinated contrast media in a hospital waste-water: A case study to analyze their presence and characterize their environmental risk and hazard. Environmental Research 140 (2015): 225-241.
- Moller T, Rickers CK, Sundmark K, et al. Environmental effective treatment and mapping of toxic medicine in hospital wastewater. Paper presented in Conference CleanMed Europe, Copenhagen, Denmark, Aarhus University Hospital, Denmark (2016).
- Mullot JU, Karolak S, Fontova A, et al. Modeling of hospital wastewater pollution by pharmaceuticals: first results of Mediflux study carried out in three French hospitals. Water Science and Technolog 62 (2010): 2912-2919.
- Nagarnaik P, Batt A, Boulanger B. Source characterization of nervous system active pharmaceutical ingredients in healthcare facility wastewaters. Journal of Environmental Management 92 (2011): 872-877.
- Nielsen U, Hastrup C, Klausen MM, et al. Removal of APIs and bacteria from hospital wastewater by MBR plus O 3, O3 + H2O2, PAC or ClO2. Water Sci Technol 67 (2013): 854-862.
- Qarni HA, Collier P, O’Keeffe J, et al. Investigating the removal of some pharmaceutical compounds in hospital wastewater treatment plants operating in Saudi Arabia. Environ Sci Pollut Res Int 23 (2016): 13003-13014.
- Sim WJ, Lee JW, Lee ES, et al. Occurrence and distribution of pharmaceuticals in wastewater from households, livestock farms, hospitals and pharmaceutical manufactures. Chemosphere 82 (2011): 179-186.
- Thomas KV, Dye C, Schlabachb M, et al. Source to sink tracking of selected human pharmaceuticals from two Oslo city hospitals and a wastewater treatment works. Journal of Environmental Monitoring 1410 (2007): 1410-1418.
- Verlicchi P, Al Aukidy M, Zambello E. Occurrence of pharmaceutical compounds in urban wastewater: Removal, mass load and environmental risk after a secondary treatment-A review. Science of the Total Environment 429 (2012): 123-155.
- Verlicchi P, Al Aukidy M, Galletti A, et al. Hospital effluent: Investigation of the concentrations and distribution of pharmaceuticals and environmental risk assessment. Science of the Total Environment 430 (2012): 109-118.
- Kovalova L, Siegrist H, von Gunten U, et al. Elimination of Micropollutants during Post-Treatment of Hospital Wastewater with Powdered Activated Carbon, Ozone, and UV. Environ Sci Technol 47 (2013): 7899-7908.
- Lin AYC, Lin AC, Tung H, et al. Potential for biodegradation and sorption of acetaminophen, caffeine, propranolol and acebutolol in lab-scale aqueous environments. Journal of Hazardous Materials 183 (2010): 242-250.
- Scheurer M, Ramil M, Metcalfe C, et al. The challenge of analyzing beta-blocker drugs in sludge and wastewater. Anal Bioanal Chem 396 (2009): 845-856.
Citation: Edward A McBean, Hamid Salsali, Munir A Bhatti, Jinhui Jeanne Huang. Beta-Blockers and Antidepressants: Contributions to Municipal Wastewaters from Hospitals and Residential Areas. Journal of Environmental Science and Public Health 2 (2018): 144-159.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 76.49%
Acceptance Rate: 76.49%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 