Assessment of the Uptake of Universal Test and Treat Strategy of HIV/AIDS in Fako Health Districts of Cameroon
Kah Emmanuel Nji1, Dickson Shey Nsagha1, Vincent Verla Siysi2, Ayok Maureen Tembei3, Eno Orock GE4, Ngowe Ngowe Marcelin5,*
1Department of Public Health and Hygiene, University of Buea, Cameroon
2Department of Internal Medicine and Pediatrics, Faculty of Health Sciences, University of Buea, Cameroon
3Department of Microbiology and Parasitology, Faculty of Science, University of Buea, Cameroon
4 Bafoussam Regional Hospital, West Region, Cameroon
5 Faculty of Medicine and Biomedical Sciences, University of Douala, Cameroon
*Corresponding Author: Professor Ngowe Ngowe Marcelin, Faculty of Medicine and Biomedical Sciences, University of Douala BP 2701 -Cameroon
Received: 08 August 2020; Accepted: 17 August 2020; Published: 24 August 2020
Article Information
Citation: Kah Emmanuel Nji, Dickson Shey Nsagha, Vincent Verla Siysi, Ayok Maureen Tembei, Eno Orock GE, Ngowe Ngowe Marcelin. Assessment of the Uptake of Universal test and treat strategy of HIV/AIDS in Fako Health districts of Cameroon. Journal of Environmental Science and Public Health 4 (2020): 229-243.
View / Download Pdf Share at FacebookAbstract
Background: In December 2016, the Cameroon ministry of Public health in collaboration with WHO updated its HIV guidelines to a test and treat all strategy, expanding antiretroviral therapy (ART) eligibility to all individuals with HIV infection, regardless of CD4+ cell count, and recommending ART be initiated within two weeks of HIV diagnosis and this has been implemented in Cameroon since 2016.
Objective: The overall objective of this study was to assess the uptake of universal test and treat strategy and associated challenges.
Methods: This was a cross sectional study where participants were randomly selected from 8 communities and 4 Health facilities within Fako Health districts.1501 and 384 participants were randomly selected from the communities and health facilities, respectively .Data was collected using electronic questionnaires and analyzed using SPSS version 25. Chi square test was used to compared proportions between categorical variables while descriptive analysis was used to measure the uptake of Universal test and treat strategy.
Results: A total of 1501 respondents were interviewed in the 8 randomly selected communities among which there were 882(58.8%) females and 619(41.1%) males. Among the 384 participants that were sampled from the 4 different health facilities,282(73.4%) and 102(26.6%) were males. With respect to history of HIV test, 1207(85.9%) reported to have ever done an HIV test in their lifetime among which majority (61%) were females and the difference was statistically significant (x2=40.1, p<0.001).Out of the 774 respondents who reported to have visited health facility in the past 12 months, only 517(69.5%) were offer HIV test which was far lower than the expected 100% in the context of universal test and treat strategy. Also, the proportion of females who accepted HIV test was significantly higher than that of the males
Keywords
<p>Universal test and treat strategy; Uptake; HIV/AIDS; Fako health districts</p>
Article Details
1. Background
HIV continues to have a major impact on public health globally with an estimated 36.9 million people living with HIV (PLWH) including 1.8 million new infections in 2017 [1]. Beginning from 2013, the Coordinating Board of the Joint United Nations Programme on HIV/AIDS (UNAIDS) called upon UNAIDS to set targets with the goal of ending the AIDS epidemic globally. In response to this, the 90-90-90 strategy was announced in 2014, laying out an ambitious worldwide target of 90% of all people living with HIV (PLWH) knowing their status, 90% of these PLWH receiving sustained antiretroviral therapy (ART), and 90% of all PLWH on ART achieving durable viral suppression by 2020 [2]. Achieving these targets is particularly important for epidemic control in sub-Saharan Africa, which remains disproportionately affected by the epidemic. At the end of 2017, 59% of PLWH in sub-Saharan Africa were receiving ART, an increase from 24% in 2010 [1] . The expansion of access to ART also resulted in a 36% reduction in AIDS-related deaths in the region over the same period [1]. These gains, however, have not been equally distributed over all countries in the region.
In 2018 in Cameroon, there were 540 000 people living with HIV. HIV incidenceper 100 (the number of new HIV infections among the uninfected population over one year among all people of all ages) was 1.02. HIV prevalence which is the percentage of people living with HIV among adults (15-49 years) was 3.6%. Also 23 000 people were newly infected with HIV and 18 000 people died from an AIDS-related illness [3].There has been progress in the number of AIDS-related deaths since 2010, with a 19% decrease, from 22 000 deaths to 18 000 deaths. The number of new HIV infections has also decreased, from 36 000 to 23 000 in the same period [3].
Over the past several years, studies have demonstrated clear benefits for treating PLWH early in disease progression [4]. Studies have shown that immediate initiation of ART after a positive HIV test result could contribute to epidemic control [5, 6] prompting the launch of the World Health Organization of the test and Treat all guidelines in 2016 [7]. To expand the test and treat all approach to sites nationwide and to decrease the time to initiating ART after a positive HIV test result, two significant changes to the national HIV prevention and treatment guidelines were made in December 2016. First, CD4+ cell count thresholds for ART initiation were removed, thus expanding ART eligibility to all HIV-positive individuals, and second, ART should be initiated as soon as possible following a positive HIV test [1]. To evaluate the uptake of the universal test and treat strategy, which was implemented in Cameroon since 2016, we conducted a community and hospital based cross sectional study.
2. Materials and Methods
2.1 Study design
This was a Hospital and community based cross sectional study that was carried out 8 in some selected communities and 4 health facilities within the Fako Health districts of the South West region of Cameroon.
2.2 Study area and setting
This study was carried out in 8 randomly selected communities and 4 health facilities within the Fako Health districts. These communities include, Upper kostain and modeka in Tiko Health district, Sandpit, and Mile 16 in Buea Health district, Munyenge in Mayuka Health district, Batoke, Watutu, and Idenau in Limbe Health district (Figure 1).
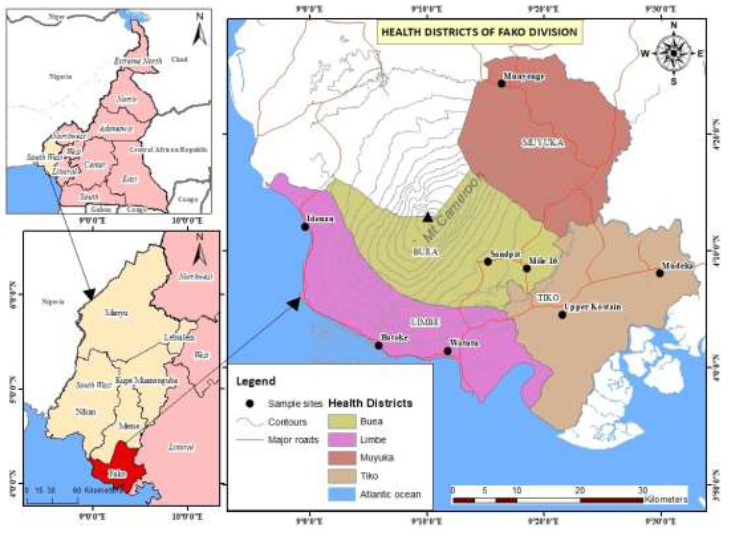
Figure 1: Map the study area.
2.3 Study population
The study population constituted two groups of participants. In the community based cross sectional study, the study population were those who were permanently living in the community and was 15 years or older and who accepted to take part in the study whereas in the Hospital based cross sectional study, those included in the study were medical personels who were also consented.
2.3.1 Sample size calculation for community-based cross-sectional study: The sample size was calculated using the single population proportion formula by karimollah, 2011 [8.] To adjust for the design effect of the sample design, the sample size was multiplied by the design effect. Hence, Z-score=1.96; Proportion= 50% marginal error=0.05, Design effect=3.5 and non-response rate=10%.
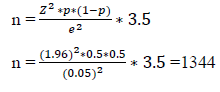
Therefore, the Minimum sample size was 1344 participants but finally a total of 1501 participants were recruited into the study.
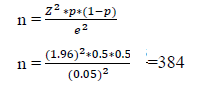
2.3.2. Sample size calculation for Hospital based cross sectional study: The sample size was calculated using the single population proportion formula by karimollah,2011 [8].To adjust for the design effect of the sample design, the sample size was multiplied by the design effect. Hence, Z-score=1.96; Proportion= 50% marginal error=0.05.
3.3 Sampling technique: A multi-stage sampling technique was used wherein, within the four health districts of Fako, 8 communities and 4 health facilities were randomly selected communities. Within each community and facility, those to participate also selected based on simple random sampling technique.
2.3.4 Data collection tools and procedures: This data was collected electronically using semi structured questionnaires. Two set of questionnaires were used, one for the community based cross sectional studies and the other for the hospital based cross sectional studies. The questionnaire for the community based cross sectional studies was made up of three sections: Section A was made up of sociodemographic characteristics of participants, section B consisted of test and treat acceptability and uptake related questions , section C had questions that assessed challenges associated with the effective implementation of the universal test and treat strategy.
2.3.5 Data analysis: Data was analyzed using SPSS version 25. Participants sociodemographic information was analyzed using descriptive statistics where results were presented in proportion and percentages. Chi square test was to use to compared proportion between categorial variables. All statistical significance was set at P<0.005.
2.4 Ethical and administrative approval
This study got ethical approval from the University of Buea Institutional Review Board. Administrative approval was sought from the Regional Delegation of Public Health for the South West Directors of health facilities and community leaders.
3 Results
3.1 sociodemographic characteristics of study participants -Community based cross sectional study
A total of 1501 participants were enrolled into this study among which there were 619 (41.2%) males and 882 (58.8%) females. The ages of the participants were categorized into four groups. Majority (41.1%) of them felt within the age group 25-35 years meanwhile 38% had ages between 15-24 years. However, 197 (13.1%) had ages between 35-44 years meanwhile those who were 45years and above constituted just 108 (7.2% ) of the study population.
Table 1: Sociodemographic characteristics of study participants -community based cross sectional study, Fako health districts, 2018.
|
Variables |
Frequency(n=1501) |
Percentage (%) |
|
Gender |
||
|
Males |
619 |
58.8 |
|
Females |
882 |
412 |
|
Age (Mean age=M±SD, 26±2.1) |
||
|
15-24 |
571 |
38 |
|
25-34 |
625 |
41.6 |
|
35-44 |
197 |
13.1 |
|
45+ |
108 |
7.2 |
|
Educational level |
||
|
No formal education |
22 |
1.5 |
|
Primary education |
282 |
18.8 |
|
Secondary education |
797 |
53.1 |
|
Tertiary education |
400 |
26.6 |
|
Religion |
||
|
Christians |
1451 |
96.7 |
|
Muslims |
32 |
2.1 |
|
Others |
18 |
1.7 |
|
Marital status |
||
|
Married/cohabiting |
622 |
41.4 |
|
Separated/divorce |
17 |
1.1 |
|
Single |
826 |
55 |
|
Widow/widower |
36 |
2.4 |
|
Occupation |
||
|
Business |
530 |
35.3 |
|
civil servant |
64 |
4.3 |
|
Farmer |
141 |
10.1 |
|
Private sector |
209 |
13.9 |
|
student |
420 |
28.0 |
|
unemployed/no job |
127 |
8.5 |
|
Income level/ FCFA |
||
|
< 50000 |
858 |
57.2 |
|
50000-100000 |
502 |
33.4 |
|
101000-200000 |
82 |
5.5 |
|
>200000 |
59 |
3.9 |
With respect to educational status, More than half (53.1%) had acquired secondary education whereas, 400 (26.6%) reported to have had tertiary education meanwhile those who reported not to have had any formal education and those who had primary education made up 22 (1.5%) and 282 (18.8 %) of the study population respectively .A vast majority (96.7%) of the study participants were Christians. As per marital status of participants, 622 (41.4%) were either married or cohabitating meanwhile those who were single constituted 826 (55%) of the study population. Widows/widowers and those who had divorced/separated made up 2.4% and 1.1% of the study population, respectively. As concerns occupation, 538 (35.3%) reported Business as their main occupation, however 420 (28%) of the study participants were students meanwhile those who were farmers and civil servants constituted 10.1% and 4.3% respectively. 209 (13.9%) reported to have been working in private sector whereas 127 (8.5%) reported that they were jobless. More than half (57.2%) of the participants reported to have monthly earnings of less than 50000FCFA while 502 (33.4 %) of the participants reported to have monthly earnings between 50000-100000FCA and only 59 (3.9%) have monthly income of more than 200000FCFA (Table 1).
3.2 Sociodemographic characteristics of study participants -Hospital based cross sectional study
In the hospital based cross sectional study, a total of 384 health workers were recruited into the study. Of the 384 participants, 282 (73.4%) were females. The mean age of the participants was 27±2.5 years. Majority (39%) of the participants were within the age group 35-44 years. As per the level of education, almost all (91.1%) reported to have acquired tertiary education. Religious wise, Christians made up 360 (93.8%) of the participants while those who reported to be Muslims constituted 20 (5.2%) of the study. As concerns monthly earnings, more than half (52.1%) of the participants reported a monthly earning of 101000-200000FCFA while only 57 (14.8%) earn greater than 200000FCFA (Table 2).
Table 2: Sociodemographic characteristics of study participants -hospital based cross sectional study, Fako health districts, 2018.
|
Variables |
Frequency(n=384) |
Percentage (%) |
|
Gender |
||
|
Males |
102 |
26.6 |
|
Females |
282 |
73.4 |
|
Age (Mean Age=M±SD, 27±2.4) |
||
|
|
||
|
15-24 |
45 |
11.7 |
|
25-34 |
106 |
27.5 |
|
35-44 |
150 |
39.0 |
|
45+ |
84 |
21.8 |
|
Educational level |
||
|
Secondary education |
34 |
8.9 |
|
Tertiary education |
350 |
91.1 |
|
Religion |
||
|
Christians |
360 |
93.8 |
|
Muslims |
20 |
5.2 |
|
Others |
4 |
1.0 |
|
Marital status |
||
|
Married/cohabiting |
250 |
65.1 |
|
Separated/divorce |
5 |
1.3 |
|
Single |
127 |
33.1 |
|
Widow/widower |
2 |
0.5 |
|
Income level/ FCFA |
||
|
< 50000 |
25 |
6.5 |
|
50000-100000 |
102 |
26.6 |
|
101000-200000 |
200 |
52.1 |
|
>200000 |
57 |
14.8 |
3.3 level of uptake of HIV/AIDS and Universal test and treat strategy
A cross section of variables were taken into consideration to assess the uptake of universal test and treat strategy ranging from Health utilization, sexual risk taking and HIV testing patterns. With respect to history of HIV test, 85.9% reported to have ever done an HIV test in their life time among which majority (61%) were females and the difference was statistically significant (x2=40.1, p<0.001).
Table 3: Health care utilization, sexual risk taking, and HIV testing patterns, Fako health distracts, 2018.
|
|
Gender |
|
|
|
|
|
Indicator |
Females (%) |
Males (%) |
Total |
X2-value |
P-value |
|
Ever done HIV test (n=1405) |
|||||
|
Yes |
736 (61.0) |
471(39.0) |
1207(85.9) |
- |
- |
|
No |
84(42.4) |
114(57.60) |
198(14.1) |
40.1 |
<0.001* |
|
Total |
820(58.4) |
585(42.6) |
1405(100) |
- |
- |
|
Seen health care provider past 12 months (n=1339) |
|||||
|
Yes |
439(59) |
305(41) |
744(55.6) |
- |
- |
|
No |
370(62.2) |
225(48.8) |
595(44.4) |
21.01 |
<0.001* |
|
Total |
809(60.4) |
530(39.6) |
1339(100) |
- |
- |
|
Offered HIV test(n=744) |
|||||
|
Yes |
335(64.8) |
182 (36.2) |
517(69.5) |
- |
- |
|
No |
130(57.3) |
97(42.7) |
227(30.5) |
21.4 |
<0.001* |
|
Total |
465(62.5) |
279(38.5) |
744(100) |
- |
- |
|
Received results (n=517) |
|||||
|
Yes |
300(66.7) |
158(33.3) |
458(88.6) |
- |
- |
|
No |
35(59.3) |
24(40.7) |
59(11.4) |
12.8 |
0.012* |
|
Total |
390(75.4) |
182(24.6) |
517(100) |
- |
- |
|
Future intention of HIV testing (n=1494) |
|||||
|
Yes |
834(59.9) |
558(40.1) |
1392(93.3) |
2.40 |
0.078 |
|
No |
47(46.1) |
55(53.9) |
102(6.7) |
- |
- |
|
Total |
881(59.0) |
613(39.1) |
1494(100) |
- |
- |
|
Number of sex partner |
|||||
|
No sex partner |
140(55.8) |
114(44.2) |
251(16.7) |
|
|
|
One sex partner |
505(58.0) |
365(42) |
870(58.0) |
4.77 |
0.771 |
|
2 or more sex partner |
149(39.5) |
228(51.5) |
377(25.3) |
- |
- |
|
Total |
646(43.0) |
707(57) |
1501(100) |
- |
- |
|
Condon use with casual sex partner (n=1312) |
|||||
|
Consistence Condon use |
79(47.3) |
88(52.7) |
167(12.7) |
- |
- |
|
Inconsistence Condon use |
703(63.4) |
442(46.6) |
1145(87.3) |
1.84 |
0.941 |
|
Total |
782(59.6) |
530(40.4) |
1312(100) |
- |
- |
The findings also showed that among those who have never done an HIV test in their life time, more than half (57.6%) were men. Also, more than half (55.6%) of the participants reported to have visited health facility in the past 12months.The proportion of women (59%) who visited the facility within the last 12 months was significantly higher than that of the males (x2=21.01, p<0.001) .Out of the 744 participants that reported to have visited the health facility in the past 12 months, only 517 (69.5%) were offer HIV among which 458 (88.6%) accepted the test and received their results following laboratory analysis. As concerns future intensions to carry out an HIV test, 93.3% of the participants reported that they have plans to carry out the test in future. Among the 102 (6.7%) participants who refused that they do not plan to carry out HIV test in future, more than half (53.9%) were males (Table 3).
3.4 Reasons for HIV testing in the past 12 months
Among the 517 participants who reported to have done HIV test in the past 12 months, different reasons were advanced as to what prompted them to do the test .More than half (62.1%) of the participants reported that they went in for this test just out of curiosity to know their HIV status .On the other hand, 30.7% reported that they did not just decide to do the test on their own but the health worker asked them to do the test while on the other hand 1.3% of participants said they did it because they wanted to get married. 0.7% reported that they did the test in case they are positive they will prevent their partners and other people from contracting the infection (Figure 2).
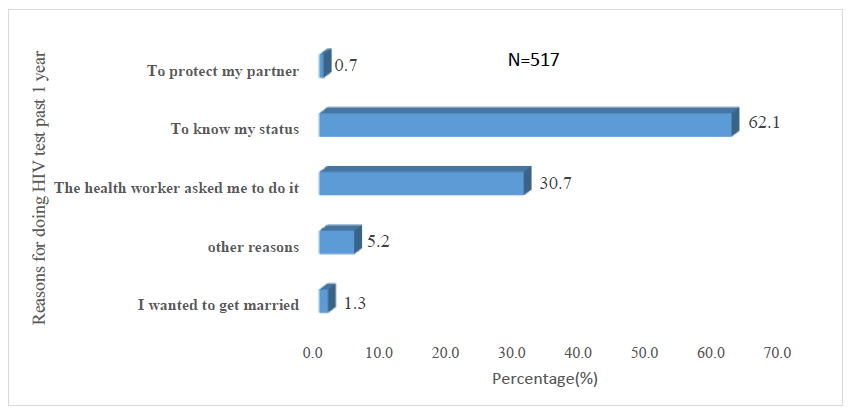
Figure 2: Reasons for taking an HIV test in the past 12 months.
3.5 Reasons for refusing to take an HIV test in the past 12 months
A total of 59 participants reported to have turned down HIV test in the past12 months and a variety of justifications were given as to why they refused to do this test. On one hand 17.1% said that they refused to do this because they were afraid of positive results and on the other hand 22.8% reported fear of stigmatization and discrimination as the main reason for refusing to take the test. Also, 17.1% said they have not been at the risk of HIV infection and therefore do not find any reason why they should do the test. 22% said they just do not want to do it. However, 21% of the participants said they were discouraged to do the test because they do not trust health workers as they can spread the news of positive results in the community (Figure 3).
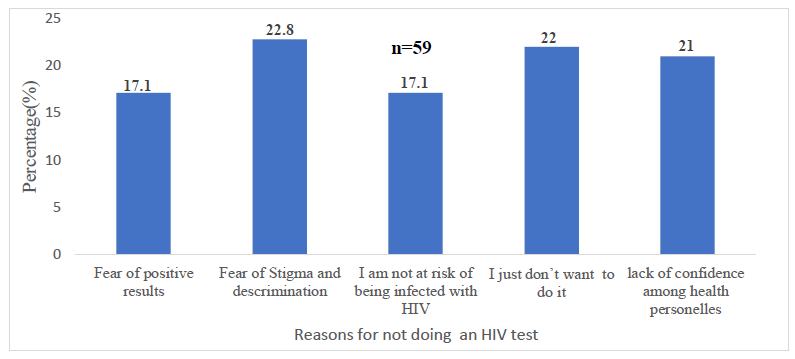
Figure 3: Reasons for not doing an HIV test.
3.6 Challenges associated with the implementation of the test and treat strategy
A total of 384 health workers were interviewed using a semi- structured questionnaire. The Health workers were drawn from the following Health facilities: Regional hospital Buea, Mutengene Baptist hospital, Tiko district Hospital, Muyuka district hospital and Limbe regional hospital. With respect to the challenges faced in the implementation of universal test and treat strategy, majority (34%) of the participants reported that patients retention in care is the major challenges as most patients do not stay on drugs once initiated .Also 56 (13%) reported that the limited number of psychosocial workers is also a challenge as these patients requires a lot of psychosocial support and follow up to be able to stay on treatment. Another challenge reported was long waiting time as reported by 11% of the participants while 12% reported lack of working spaces to provide services as another challenge. Other changes include limited number of HIV testers, frequent drug stock out and unavailability of test kits (Table 4).
Table 4: Challenges associated with the implementation of universal test and treat strategy Fako health districts, 2018.
|
Identified Challenges associated with the implementation of test and treat strategy |
Frequency (n=384) |
Percentage (%) |
|
Frequent drug stock out |
23 |
6 |
|
Limited number of Psychosocial counsellors |
56 |
13 |
|
Lack of space to provide services |
46 |
12 |
|
Unavailability of test kits |
35 |
9 |
|
long waiting time |
42 |
11 |
|
Poor retention in care |
131 |
34 |
|
Limited number of HIV testers |
31 |
8 |
|
Issues of confidentiality |
5 |
19 |
|
Rude nature of some health workers |
2 |
2 |
4. Discussion
Our study aimed at assessing the uptake universal test and treat strategy of HIV/AIDS and associated challenges following 3 years after its implementation. Our findings showed that 85% our participants have ever done an HIV test. These findings are in line with that reported by PEPFAR in 2020 [9]. However, within the past 12 months only 69% of those who visited the health facility were offered an HIV test. The principles of universal test and treat stipulates that HIV test should be systematically offered to everybody that visits the hospital irrespective of the illness and this in order to meet the 90-90-90- target [2]. Our findings showed that this is not systematically done. Investigation showed that most of the health facilities use screening tools ( screening tool is a document that contains a series of HIV exposed related questions that are asked to the patient and the responses determine whether the patients will be tested or not ) to identify if a patients is eligible for testing or not and by so doing do not screen everybody. Among those who reported to have done an HIV test in the past 12 months, the number of women were significantly higher than the males. Studies conducted in six Sub-Sahara African countries revealed similar pattern [10]. Majority of our participants reported that they have intensions to do the test in the future among these, there were more women compared to men though the difference was not statistically different. Studies have demonstrated that women turn to have a positive health seeking behavior compared to men [10]. In finding out reasons why an HIV test was done within the past 12 months, more than half of the participants reported that they just wanted to know their status .Also, 30.7% reported that they did the test because it was requested by the Doctor. Some participants gave different reasons why they have not done an HIV test in the past 12 months. Majority of the participants reported that they are afraid of stigma and discrimination. stigma and discrimination as a barrier to HIV testing has also be reported in other studies [2]. Other stated that they lack confidence among the health personels, and they argued that health workers have the tendency to spread the news of positive results to other people. These findings are in line with findings reported in Ghana [11]. Another reason advanced for not been tested was that they have not been at risk of HIV and so no need to do the test. The coincides with a study that was conducted by Pisculli et al [12]. Also, fear of positive results was another reason advanced by participants for not taking an HIV test in the past 12 months. The consensus was that they prefer not to know their HIV status and stated that just knowing that one is positive is enough to psychologically destabilize him/her. Studies carried out in Uganda among couples also identified fear of positive results as a barrier to the uptake of HIV testing [13]. Similar findings have been reported in studies conducted in Puru [14].
Apart from the community-based survey, a hospital-based survey was also conducted to identify challenges that are hindering the effective implementation of the universal test and treat strategy. More than half of the participants reported that the limited number of psychosocial workers affect effective follow up of patients, and this consequently leads to poor retention. The argument is that the advent of universal test and treat strategy has brough an increase in the number of positives cases identified and placed on treatment and this requires close follow by the Psychosocial workers for them to stay on treatment .studies carried in Sub-Sahara Africa underscored the importance of psychosocial workers in the attainment of the 90-90-90 targets [15]. Also, as much as 12% of the participants reported lack of spaces to offer services and hence confidentiality of the patient is violated as this is done in the open air. Also, this study revealed frequent drugs stock out as another challenge that hinders the uptake universal test and treat strategy. This is in line with Studies conducted by Bella Hwang et al in south Africa, who also reported frequent drug stock out as one of the major challenges associated with the implementation of the test and treat strategy [16]. Participants also reported long waiting time to be offered services as a barrier to the implementation of this strategy and this has greatly affected retention. This has also been reported by kwapong et al where pregnant women On ART reported that waiting for a long period of time before services are offered renders them dissatisfied and discouraged [17]. The poor attitude of health workers towards patients also stood out as a barrier to the implementation of the test and treat strategy. Other studies have also reported the poor attitude of health workers as barrier to the implementation of test and treat strategy [17, 18].
5. Conclusion
Following 2 years of implementation of universal test and treat strategy, it was necessary to assess I uptake and associated challenges that could hinder the attainment of the 90-90-90 target. Our findings showed that more women were being tested for HIV than Men and the uptake of the universal test and treat was low given that testing was not systematically offered to patients during hospital visits. fear of positive of positive results and discrimination were the main reasons why people do not accept to do an HIV test. At the level of the health facilities, limited number of the psychosocial works among others was reported as the main challenge in the implementation of test and universal treat strategy. Moving forward, it is crucial to recognize that fear of a positive HIV test result is related to many interconnected negative health and social outcomes (e.g. stigma, depression, early death from taking medication, separation). Fear remains a major barrier to HIV screening in general, Additional research and health promotion advocacy work should be done not only to decrease the fear associated with HIV testing, but also to increase the awareness of the benefits of an early diagnosis, including the effectiveness of the treatment on one’s health and the reduction of transmission to one’s sexual partner. Also, materials, and human resources are highly needed to scale up this strategy to bring the pandemic under control by 2030.
6. Limitation of the Study
In assessing the effective implementation of the universal test and treat strategy, our study focused mostly on testing which is a gateway to treatment and less was done on the treatment outcome in the context of test and treat strategy. In order to better appreciate the uptake and impact of test and treat strategy, we therefore recommend that another study be done to assess HIV/AIDS treatment outcomes in the context of test and treat strategy.
Conflict of Interest
The authors declare that there are no conflicts of interest.
Acknowledgements
This is part of a Ph.D. thesis by Kah Emmanuel Nji under the supervision of Prof. Ngowe Ngowe Marcelin and co-supervised by Professor Nsagha Dickson Shey, Professor Vincent Verla in the Department of Public Health and Hygiene of the University of Buea. We acknowledge all stakeholders including the District Medical Officers of Fako Health Districts, Regional Delegate for Public Health-South West Region, Chief of Health Centres, Heads of HIV treatment centers, Community leaders and colleagues for their contributions in the realization of this study. We equally acknowledge all the participants of this study for their collaboration.
References
- UNAIDS GA. Global AIDS update 2016. Geneva Switz World Health Organ Libr (2016).
- Granich R, Williams B, Montaner J, et al. 90-90-90 and ending AIDS: necessary and feasible. The lancet 390 (2017): 341-343.
- Cameroon UNAIDS [Internet]. [cited 2020 Aug 3].
- Group ISS. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med 373( 2015): 795-807.
- Fox MP, Rosen S, Geldsetzer P, et al. Interventions to improve the rate or timing of initiation of antiretroviral therapy for HIV in sub-Saharan Africa: meta-analyses of effectiveness. J Int AIDS Soc 19 (2016): 20888.
- Rosen S, Maskew M, Fox MP, et al. Initiating antiretroviral therapy for HIV at a patient’s first clinic visit: the RapIT randomized controlled trial. PLoS Med 13 (2016): e1002015.
- Organization WH. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. World Health Organization (2016).
- Hajian-Tilaki K. Sample size estimation in epidemiologic studies. Casp J Intern Med 2 (2011): 289.
- Global HIV/AIDS Overview | HIV.gov [Internet]. [cited 2020 Aug 6].
- Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract 17 (2016): 38.
- Dapaah JM, Senah KA. HIV/AIDS clients, privacy and confidentiality; the case of two health centres in the Ashanti Region of Ghana. BMC Med Ethics 17 (2016): 41.
- Pisculli ML, Reichmann WM, Losina E, et al. Factors associated with refusal of rapid HIV testing in an emergency department. AIDS Behav 15 (2011): 734-742.
- Nannozi V, Wobudeya E, Gahagan J. Fear of an HIV positive test result: an exploration of the low uptake of couples HIV counselling and testing (CHCT) in a rural setting in Mukono district, Uganda. Glob Health Promot 24 (2017): 33-42.
- Blas MM, Alva IE, Cabello R, et al. Risk behaviors and reasons for not getting tested for HIV among men who have sex with men: an online survey in Peru. PLoS One 6 (2011): e27334.
- Bemelmans M, Baert S, Negussie E, et al. Sustaining the future of HIV counselling to reach 90-90-90: a regional country analysis. J Int AIDS Soc 19 (2016): 20751.
- Hwang B, Shroufi A, Gils T, et al. Stock-outs of antiretroviral and tuberculosis medicines in South Africa: A national cross-sectional survey. PloS One 14 (2019): e0212405.
- Kwapong GD, Boateng D, Agyei-Baffour P, et al. Health service barriers to HIV testing and counseling among pregnant women attending Antenatal Clinic; a cross-sectional study. BMC Health Serv Res 14 (2014): 267.
- Fanta W, Worku A. Determinants for refusal of HIV testing among women attending for antenatal care in Gambella Region, Ethiopia. Reprod Health 9 (2012): 8.


 Impact Factor: * 3.6
Impact Factor: * 3.6 Acceptance Rate: 76.49%
Acceptance Rate: 76.49%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 