Long-Term Results of Patients with Hemochromatosis after Bariatric Surgery
Romina Frey*,1, Urs Pfefferkorn1, Monica La Vista2, Rudofsky Gottfried3
1General Surgery, Kantonsspital Olten, Olten, Switzerland
2Obesity Clinic, Kantonsspital Olten, Olten, Switzerland
3Private Practice, Olten, Switzerland
*Corresponding author: Romina Frey, General Surgery, Kantonsspital Olten, Olten, Switzerland.
Received: 05 October 2025; Accepted: 13 October 2025; Published: 10 November 2025
Article Information
Citation: Romina Frey, Urs Pfefferkorn, Monica La Vista, Rudofsky Gottfried. Long-Term Results of Patients with Hemochromatosis after Bariatric Surgery. Archives of Microbiology and Immunology. 9 (2025): 248-251.
View / Download Pdf Share at FacebookAbstract
Hereditary hemochromatosis is one of the most common hereditary metabolic disorders. We present the cases of two patients with hereditary hemochromatosis who were treated with regular phlebotomies and the long-term outcome after bariatric surgery and we provide an overview of the published cases of patients with hemochromatosis who have undergone bariatric surgery. In both patients, the regular phlebotomies before the bariatric operation could be stopped postoperatively without an increase in serum ferritin levels. Bariatric operations are therefore able to control the iron overload in patients with hemochromatosis and eliminate the need for phlebotomies.
Keywords
<p>Hemochromatosis, gastric bypass, sleeve gastrectomy</p>
Article Details
Introduction
Hereditary hemochromatosis is one of the most common hereditary metabolic disorders with an incidence of 1/200 in Caucasian populations in the United States and Western Europe. Due to a mutation, the control of iron absorption is lost which leads to an iron overload. Therapy consists of regular phlebotomies to deplete the elevated iron deposits to prevent secondary organ damage. Contrarily, bariatric operations are known to induce iron deficiencies, which may arise from the substantial reduction in food intake. Iron deficiency in Roux-en-Y Gastric Bypass (RYGB) patients may also result from malabsorption (because the main sites of iron absorption have been bypassed) and from reduced bioavailability of dietary iron because of the lack of hydrochloric acid production in the small gastric pouch [1]. There are only few cases and case series published showing a beneficial effect of bariatric surgery concerning iron overload in patients with hemochromatosis within the first years after operation [2-7].
Methods
We present two cases with hereditary hemochromatosis, which were treated with laparoscopic proximal gastric bypass and laparoscopic sleeve gastrectomy, respectively. Both patients gave written consent to publish their retrospectively collected data anonymously.
Results
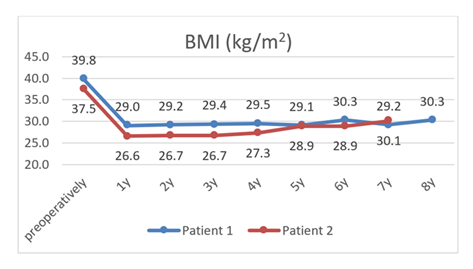
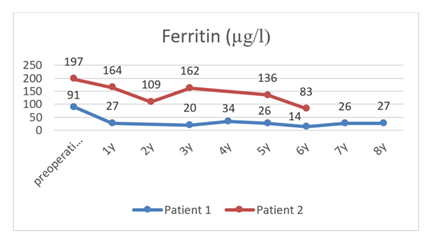
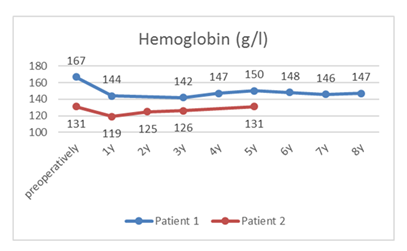
A 48-year-old male patient received a proximal gastric bypass and a 49 year-old female patient underwent sleeve gastrectomy 6, respectively 4 years after the initial diagnosis of hemochromatosis. Baseline demographics of the two patients are shown in table 1. Both patients were treated by repetitive phlebotomies prior to their bariatric surgery. The decision to perform a sleeve gastrectomy was taken because of patient preference for this procedure. The post-bariatric course was uneventful in both cases with good results concerning weight control (diagram 1). The maximum percent total BMI loss (%TBMIL) was 27.1% in Patient 1 and 29.1% in Patient 2. %TBMIL at the last recorded follow-up was 23.9% and 19.7%, respectively. Patient 1 received additional supplementation of vitamin B12 and Vitamin D on top of the standard oral multivitamin according to the vitamin levels in his regular blood checks. Patient 2 developed no malnutrition but a reflux oesophagitis grade C according to the Los Angeles classification, which was asymptomatic and successfully treated with oral proton pump inhibitors. In both patients the regular phlebotomies before the bariatric operation could be stopped postoperatively without an increase in serum ferritin levels (diagram 2) and stable haemoglobin (diagram 3). This effect was permanent and still there at the last follow-up at 8 respectively 6 years postoperatively.
Table 1
|
Patient 1 |
Patient 2 |
|
|
age |
48 |
49 |
|
Gender |
Male |
Female |
|
mutation |
HFE C282Y homozygous |
HFE C282Y/H63D compound heterozygous |
|
Time from diagnosis of hemochromatosis to surgery |
6 years |
4 years |
|
Type of operation |
Proximal gastric bypass |
Sleeve gastrectomy |
|
Follow-up after bariatric operation |
8 years |
7 years |
|
BMI at surgery |
39.8 kg/m2 |
37.5 kg/m2 |
Table 2
Discussion
Including our two patients, there are thirteen reported cases of patients with hemochromatosis undergoing RYGB or sleeve gastrectomy until today (table 2). The follow-up time ranges from 1 to 8 years and all patients had a successful weight reduction. In all cases phlebotomies could be stopped and ferritin levels remained low even in long term follow-up, despite the possible adaptation of the more distal small bowel to improve iron absorption. Patients with a RYGB seem to reach lower ferritin levels than those with sleeve gastrectomies, but the number of cases is too small for this to be statistically significant. Because a major component of RYGB, in addition to stomach reduction, is the exclusion of the duodenum and the portion of the jejunum, which is the main location of iron absorption, it is reasonable to assume, that this result would be confirmed in larger series [8]. There seem to be no negative effect of the hemochromatosis on the success of the bariatric operation.
Conclusion
The reduced iron intake and absorption after bariatric interventions is outweighing the uncontrolled iron absorption in hemochromatosis. Bariatric operations are therefore able to control the iron overload in patients with hemochromatosis and eliminate the need for phlebotomies. There seems to be an advantage for gastric bypass over sleeve gastrectomy, most likely due to the bypassing of the main location of the iron uptake in the duodenum and the proximal jejunum.
Acknowledgments
All authors were involved in editing the manuscript.
Statement of funding sources and conflicts of interest
The authors received no specific funding for this work. The authors declare no conflicts of interest.
References
- Yeongkeun Kwon, Hyun Jung Kim, Emanuele Lo Menzo, Anemia, iron and vitamin B12 deficiencies after sleeve gastrectomy compared to Roux-en-Y gastric bypass: a meta-analysis. Surgery for Obesity and Related Diseases 10 (2014): 589–599
- James C Barton Hemochromatosis, HFE C282Y homozygosity, and bariatric surgery: report of three cases. Obesity Surgery 14 (2004): 1409-14
- Mickey Ott, Chad Stouffer, James Foote, Anthony Foster Roux-en-Y gastric bypass: a novel approach to the treatment of hemochromatosis? American Journal of Hematology 82 (2007): 1033.
- Ganesh C Kudva, Bruce R Bacon Iron deficiency anemia in hereditary hemochromatosis after gastric bypass surgery Annals of Hematology 88 (2009): 291-2.
- S Gopaluni, C Martinez-Balzano, S Graziano. Gastric bypass surgery as an intervention for obese patients with hemochromatosis Quarterly Journal of Medicine 107 (2014): 1023-5.
- Phan, C. Vatier, C. Vauloup-Soupault, Christine Poitou, J. Bouillot, et al. Diabetes remission after bariatric surgery in obese patients with haemochromatosis. Diabetes and Metabolism 4 (2017):185-187
- Yagnik Pandya, Darius Ameri, Jacqueline Paolino. Roux en Y gastric bypass as a proposed treatment operation for patients with hemochromatosis- a case series Surgery for Obesity and Related Diseases: 13 (2017): S80
- Schumann K, Elsenhans B, Forth W, Schroeder P. Intestinal iron transfer after ileojejunal transposition. Digestion 50 (1991): 182–93.


 Impact Factor: * 3.5
Impact Factor: * 3.5 Acceptance Rate: 71.36%
Acceptance Rate: 71.36%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 
