Microwave Treatment Prevents Cytomegalovirus Transmission to Preterm Infants through Human Milk
Mizuno K1*, Kohda C2, Den H3
1Department of Pediatrics, Showa University School of Medicine
2Department of Microbiology and Immunology, Showa University School of Medicine
3Department of Hygiene, Public Health, and Preventive Medicine, Showa University School of Medicine
*Corresponding Author: Katsumi Mizuno, Department of Pediatrics, Showa University School of Medicine 142-8666, 1-5-8 Hatanodai, Shinagawa-ku, Tokyo, Japan
Received: 06 July 2022; Accepted: 11 July 2022; Published: 14 July 2022
Article Information
Citation: Mizuno K, Kohda C, Den H. Microwave Treatment Prevents Cytomegalovirus Transmission to Preterm Infants through Human Milk. Journal of Food Science and Nutrition Research 5 (2022): 608-611.
DOI: 10.26502/jfsnr.2642-110000103
View / Download Pdf Share at FacebookAbstract
Background: Mother’s own milk (MOM) is the best nutrition for preterm infants; however, milk from cytomegalovirus (CMV)-seropositive mothers may cause the transmission of the virus to the infants. As extremely preterm infants are at a risk of developing serious conditions due to CMV infection, even MOM is sometimes pasteurized. Previously, we demonstrated that microwave heating of 50 mL formula milk containing CMV at 500 W for 40s prevented CMV infection in living cells. However, we do not know if this is the case with reactivated CMV in human milk (HM). Therefore, we investigated if microwave heating of HM would be effective in preventing CMV infection in living cells.
Methods: Twenty-three CMV-IgG-positive and four CMV-IgG-negative mothers who donated HM to the human milk bank during 6 to 16 weeks postpartum were enrolled. The HM was treated with microwave at 500 W. HFL-III cells were seeded in culture dishes. Aliquots of HM samples subjected to microwave was inoculated onto susceptible cell monolayers. Infectious vial titer was measured by the 50% median tissue culture infectious Dose (TCID50) assay.
Results: The TCID50 assay was decreased in five out of eight 100-mL samples after microwave at 200W for 60 s. The CMV infectivity assay was negative in three, decreased in eight, and no change in six 100-mL samples, and negative in four and decreased in eight 50-mL samples.
Conclusions: Microwave heating of HM at low settings could decrease CMV transmission through HM, however, to obtain entire prevention is difficult when loss of bioactive properties is considered.
Keywords
<p>Human milk, Cytomegalovirus, Microwave, Preterm infant</p>
Article Details
1. Introduction
Human milk (HM) is an optimal source of nutrition for infants and is even considered therapeutic for preterm infants. However, HM from mothers who are seropositive for cytomegalovirus (CMV) can be a source of postnatal infection in preterm infants. The estimated cumulative rate of transmission of CMV from seropositive mothers to preterm infants is 37% [1]. Extremely preterm infants are at a high risk of developing a sepsis-like syndrome, cholestasis, or bronchopulmonary dysplasia because of the absence of the transmission of maternal antibodies. The strategy to prevent CMV transmission via HM differs among countries. France and Austria recommend pasteurization of HM from CMV-seropositive mothers until 32 and 34 weeks post-conception, respectively [2]. However, it is unclear whether HM from CMV-seropositive mothers should be pasteurized as this procedure can cause loss of bioactive properties. There has been no clear consensus on whether HM from CMV-seropositive mothers should be treated. Ben-Shoshan et al. [3]3 demonstrated the relevance of microwave (MW) heating on prevention of CMV infection in HM. We have previously added CMV with a viral load of 5.0 ×103 plaque-forming units/mL to 50 mL of formula milk, resulting in 772 plaque-forming units/mL at baseline. After MW heating, the supernatants (0.1 mL) were inoculated onto susceptible cell monolayers and incubated for 90 min to allow viral attachment to cells [4]. There was no cell infection observed following 500 W heating for 40 s. Furthermore, MW heating of 100 mL HM at 500 W for 40 s did not result in a significant reduction in secretory immunoglobulin A (SIgA), lactoferrin, or transforming growth factor (TGF)-beta levels in HM [5]. Although MW heating of formula milk at 500 W for 40 s was effective in preventing the CMV infection in living cells, we do not know if this is the case in reactivated CMV in HM. Furthermore, the viral load of CMV in HM differs depending on the individuals and period after the delivery. As reported in the previous study, heating to 60 °C for a short time would be effective in preventing CMV infection. Formula milk (100 mL) at an initial temperature of 10 °C reaches 60 °C when exposed to 500 W MW heating for 40 s [4]. However, 100 mL of breast milk did not attain a temperature of 60 °C following treatment with 500 W MW heating for 40 s under the same conditions [6]. Therefore, we used HM derived from CMV-positive mothers to determine whether MW treatment prevents CMV infection in living cells.
2. Methods
Participants
We used HM derived from 27 participants aged 29-41 y (mean 32.1 y), who gave birth from March to August 2021, and were 6-16 weeks postpartum (Median, 9; Q1, 7; Q2, 9; Q3, 10; interquartile range, 3) when they donated their HM. This HM was frozen prior to use for up to 3 months. All participants were donors for the HM bank in Japan. The HM samples were tested for CMV IgG antibodies, Human Immunodeficiency Virus (HIV), Human T-cell Leukemia Virus (HTLV), Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and syphilis at the time of registration. The inclusion criteria for the donors were same as human milk banking association of North America (HMBANA); the babies were exclusively breastfed and growing well, and the donors had no comorbidities [7]. To maintain confidentiality, we allocated a unique number to each donor. Data were stored in a personal computer that was never connected to the internet. Samples of HM used in this experiment were rejected when excessive bacterial counts were recorded, and permission to use donor’s HM for this study was given by all donors. Prior to use, frozen HM was placed in a refrigerator, thawed overnight, and subsequently, stirred well by hand. The experiment was performed in the research laboratory of the Department of Pediatrics, Showa University School of Medicine, Japan.
3. Data Analysis
Treatment of HM with MW heating
A MW oven (DR-D278B; Twinturbo Co. Ltd, Niigata, Japan) was used for the experiment. After MW treatment, HM samples were stored at -20 °C until further use.
Experiment 1
Milk samples (100 mL) were placed in 160-mL glass bottles and heated using a MW oven for 60 s at 200 and 500 W.
Experiment 2
Milk samples (50 and 100 mL) were placed in 160-mL glass bottles, followed by heating for 60 s at 500 W.
Determination of HCMV-DNA copies
Determination of the number of HCMV-DNA copies was performed as previously described, with minor modifications [4]. Briefly, DNA was extracted from HM using a QIAamp DNA mini kit (Qiagen, Hilden, Germany), and a real-time polymerase chain reaction (real time-PCR) was performed using LightCycler 480 instrument (Roche Diagnostics, Basel, Switzerland).
Investigation of CMV infectivity titer
Investigation of CMV infectivity titer was performed using median tissue culture infectious dose (TCID50). The HFL-III cells were propagated in 15% fetal bovine serum supplemented with DMEM/Ham’s F-12 medium. Cells were maintained in 5% CO2 and 37 °C in an incubator. The HM samples were centrifuged at 8,000 g for 5 min, and the supernatant was collected for determining the infectious viral titer. The supernatants of HM obtained after centrifugation (0.1 mL) were inoculated onto susceptible cell monolayers and incubated for 90 min to allow viral attachment to cells. After 14 days of incubation, TCID50/mL was measured to quantify the CMV infectivity titer.
4. Results
Experiment 1
CMV-DNA was detected in all CMV-positive mother's milk samples and was below the detection limit in CMV-negative mother's milk samples (Table 1). After 200 W or 500 W of MW treatment, the number of CMV-DNA copies did not significantly differ from that of control samples (Table 1). The TCID50/mL value was zero for CMV-negative mother's milk samples, and infectious virus was not detected. However, the infectious virus was determined in seven of eight samples of non-treated CMV-positive mother's milk after freezing at −20°C. After 200 W of MW heat treatment, TCID50/mL decreased in five out of eight samples of CMV-positive mother's milk (Table 1). Although a significant decrease was observed in TCID50/mL after 200 W MW heat treatment of milk samples for 60 s (Wilcoxon rank sum test, p=0.036) compared to that in control samples, the infectious CMV still persisted in the treated samples. A similar result was obtained after 500 W MW heat treatment. Therefore, we decreased the volume of milk to determine whether a smaller volume improved the prevention of CMV infection following treatment with the same MW heat setting (Experiment 2).
Experiment 2
The volume of HM was reduced from 100 mL to 50 mL, followed by MW heat treatment. CMV-DNA was detected in all the milk samples used in experiment 2, with viral titers ranging from 2,840 to 117,467 copies/mL (Table 2). After 500 W, 60 s of MW heat treatment, the number of CMV-DNA copies did not differ significantly among treated or control samples (Table 2). The TCID50/mL was 100 for all non-treated HM samples in experiment 2 and CMV was not inactivated by freezing at -20 °C. After 100 mL of HM was treated with MW heating at 500 W for 60 s TCID50/mL decreased in 6 of 10 CMV-positive milk samples. In contrast, TCID50/mL decreased in all 12 CMV-positive samples with 50 mL volume after exposure to 500 W for 60 s. Thus, MW heat treatment inactivated CMV with a decrease in TCID50/mL; infectivity of CMV was completely lost in 4 of 12 samples of HM with 50 mL volume following MW heat treatment for 60 s. In total, 17 HM samples (100 mL) were treated with MW heating at 500 W for 60 s, resulting in significant decrease in TCID50/mL (Wilcoxon signed rank test, p<0.001) across experiments 1 and 2. A significant decrease in TCID50/mL (Wilcoxon signed rank test, p<0.001) was also demonstrated when 50 mL of HM was treated with MW heating (500 W) for 60 s. When we compared the decrease in TCID50/mL between 50 mL and 100 mL samples, a significantly higher decrease was observed in the 50 mL samples than that in the 100 mL samples (Wilcoxon signed rank test, p=0.016).
Number of CMV-DNA copies in HM samples was same that we reported in our previous study [8]. The number of CMV-DNA copies at baseline did not change even if MW heat treatment was performed. This result supports our previous study [4]. In addition, the association was not recognized between DNA copy number and CMV infectivity titer.
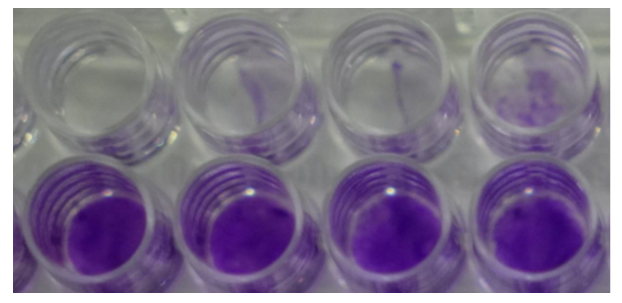
Figure 1: CMV infected cells
|
Sample |
number of CMV-DNA copies per milliliter |
TCID50 per milliliter |
||||
|
No treat |
200 W treat |
500 W treat |
No treat |
200 W treat |
500 W treat |
|
|
A |
679 ± 73 |
1352 ± 96 |
1281 ± 310 |
100 |
10 |
10 |
|
B |
27300 ± 1229 |
3680 ±1060 |
1056 ± 247 |
100 |
10 |
10 |
|
C |
10760 ± 510 |
7087 ± 136 |
13030 ± 1811 |
100 |
10 |
10 |
|
D |
1649 ± 271 |
1183 ± 351 |
1603 ± 217 |
10 |
10 |
10 |
|
E |
1952 ± 604 |
1071 ± 323 |
1633 ± 993 |
0 |
0 |
0 |
|
F |
2145 ± 1684 |
3636 ± 2323 |
3975 ± 2022 |
10 |
0 |
0 |
|
G |
1336 ± 115 |
1300 ± 616 |
1083 ± 408 |
10 |
10 |
10 |
|
H |
2329 ± 1613 |
2327 ± 446 |
2980 ± 225 |
10 |
0 |
0 |
|
I |
< 200 |
ND |
ND |
0 |
ND |
ND |
|
J |
< 200 |
ND |
ND |
0 |
ND |
ND |
ND: not done
Table 1: The number of HCMV-DNA copies and the value of TCID50 in the human milk (100ml) after 200W/500W for 60s
|
Sample |
number of CMV-DNA copies per milliliter |
TCID50 per milliliter |
||||
|
No treat |
50 mL treat |
100 mL treat |
No treat |
50 mL treat |
100 mL treat |
|
|
K |
3367 ± 151 |
3373 ± 31 |
ND |
100 |
10 |
ND |
|
L |
108667 ± 14257 |
117467 ± 29223 |
73267 ± 60802 |
100 |
10 |
10 |
|
M |
5393 ± 1068 |
3120 ± 647 |
3793 ± 1437 |
100 |
10 |
ND |
|
N |
45533 ± 8778 |
40067 ± 4163 |
35067 ± 5558 |
100 |
0 |
0 |
|
O |
28600 ± 6762 |
23200 ± 3650 |
37400 ± 4915 |
100 |
10 |
100 |
|
P |
4500 ± 1733 |
4173 ± 978 |
3387 ± 220 |
100 |
0 |
10 |
|
Q |
5307 ± 808 |
2840 ± 410 |
3560 ± 92 |
100 |
0 |
10 |
|
R |
4440 ± 1193 |
2893 ± 527 |
2947 ± 613 |
100 |
0 |
10 |
|
S |
3267 ± 1196 |
5927 ± 2400 |
2827 ± 437 |
100 |
10 |
100 |
|
T |
3680 ± 260 |
4426 ± 338 |
4220 ± 253 |
100 |
10 |
100 |
|
U |
23467 ± 2203 |
20927 ± 2024 |
21473 ± 8192 |
100 |
10 |
100 |
|
V |
30400 ± 721 |
9873 ± 471 |
30733 ± 2715 |
100 |
10 |
10 |
ND: not done
Table 2: The number of CMV-DNA copies and the value of TCID50 in the human milk with 500W for 60s (50ml and 100ml)
5. Discussion
In this study, we demonstrated that infectious CMV persisted even if HM samples were kept frozen for more than one month. Furthermore, we demonstrated that MW heat treatment with 200 W or 500 W can prevent CMV infection to some extent. We have already reported that MW heating of formula milk, to which CMV was artificially added, at 500 W for 40 s was effective in preventing CMV infection. There was a discrepancy between the results of our previous study and this study. One of the reasons is that formula milk was heated to a higher temperature than HM with the same MW heat setting and for the same duration. Consequently, even if the same volume of HM is heated with 500 W for 60 s, the temperature attained is less than 60 °C. Furthermore, in our previous study, we added live HCMV to formula milk and then treated with MW heating, but in this study, we used HM expressed by CMV IgG positive donors. Reactivated CMV in HM might have better viability compared to the HCMV Towne strain. In general, viral agents in HM show lower rates of infection compared to those in buffers [9]. Our experiments demonstrated that CMV cell infection could be prevented to some extent by treatment with 500 W 60 s MW heating for 100 mL samples of HM. When we decreased the volume of milk from 100 mL to 50 mL, the effectiveness of MW irradiation in reducing viral titer was significantly larger. We have previously demonstrated that the levels of SIgA, lactoferrin, and TGF-beta in 100 mL of HM samples were not affected by irradiation with 500 W for 60 s [5]. The temperature of 50 mL HM samples increased significantly compared to that for 100 ml samples at the same MW heat settings. Therefore, the bioactive properties in HM are decreased more in 50 mL milk samples. We always must consider a balance between the benefit and risk whenever we utilize a new intervention. We have previously found that there was some decrease even with 200 W 60 s MW heat treatment that did not lead to a loss of bioactive properties in HM milk samples [5]. Furthermore, rise in temperature of HM samples after exposure to 200 W for 60 s is between 22.8 and 24.2 °C. Although the temperature itself does not rise enough to inactivate CMV, some positive effects remain, probably due to the power of MW radiation. A 60 s treatment of 100 mL HM samples using either 200 W or 500 W did not reduce the CMV titer, and therefore further examination is required to establish a means for complete prevention of CMV infection. However, a significant fraction of bioactive substances in HM would be lost following application of higher power MW. To decrease CMV infection as well as to minimize the loss of bioactive properties in HM, we suggest investigating a combination of 100 mL of milk and 500 W for 60 s using randomized control trials to establish the clinical prevention of CMV transmission through HM.
Ethics approval and consent to participate
This study was approved by Showa University Research Ethics Review Board (approval number: 2714)
Consent for publication
We obtained written consent for publication from participants.
Availability of data and materials
Competing interests
We do not have any competing interests.
Funding
This work was supported by MEXT Grant Number 20K08217.
Authors' contributions
Provide individual author contribution
Conception and design of study
K Mizuno; acquisition of data: K Mizuno and C Kohda; analysis and/or interpretation of data: C Kohda, and H Den.
Drafting the manuscript
K Mizuno, H Den, and C Kohda; revising the manuscript critically for important intellectual content
Approval of the version of the manuscript to be published (the names of all authors must be listed)
K Mizuno, C Kohda, and H Den, N agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the warok are appropriately investigated and resolved.
Acknowledgements
This work was supported by MEXT Grant Number 20K08217
References
- Hamprecht K, Maschmann J, Vochem M, et al. Epidemiology of transmission of cytomegalovirus from mother to preterm infant by breastfeeding. Lancet 357 (2011): 513-518.
- Bonet M, Durox M, Blondel B, et al. Management of mother's own milk for very preterm infants in tertiary-level neonatal units in the Ile-de-France region in France. Breastfeed. Med 9 (2014): 47-48.
- Ben-Shoshan M, Mandel D, Lubetzky R, et al. Eradication of cytomegalovirus from human milk by microwave irradiation: A pilot study. Breastfeed. Med 11 (2016): 186-187.
- Mikawa T, Mizuno K, Tanaka K, et al. Microwave treatment of breast milk for prevention of cytomegalovirus infection. Pediatr Int 61 (2019): 1227-1231.
- Yamamoto K, Mizuno K, Sakurai M, et al. Effects of microwave radiation on human milk properties. Japan Society for Neonatal Health Development 32 (2020): 179-183.
- Yoshida et al. Microwave heating of human milk with direct temperature monitoring. J Hum Lact in print
- The Nippon Foundation Human Milk Bank. Donor Registration Requirements. Our Standards | The Nippon Foundation Human Milk Bank.
- Wakabayashi H, Mizuno K, Kohda C et al. Low HCMV DNA copies can establish infection and result in significant symptoms in extremely preterm infants: A prospective study. Am J perinatal 29 (2012): 377-382.
- Gallo V, Giansanti F, Arienzo A, et al. Antiviral properties of whey proteins and their activity against SARS-CoV-2 infection. J Funct Foods 89 (2022): 104932.


 Impact Factor: * 3.8
Impact Factor: * 3.8 Acceptance Rate: 77.96%
Acceptance Rate: 77.96%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 