An Unusual Metastatic Signet-ring Cell Carcinoma of the Rectosigmoid Colon Presenting as Mandibular Tumor in a Female patient: A Case Report and Review of the Literature
Kuang-Ting Liu1, 2, Yueh-Ching Chang1, 2, Yu-Chieh Lin1, 3, Junn-Liang Chang1, 3, 4*
1Department of Pathology and Laboratory Medicine, Taoyuan Armed Forces General Hospital, Taoyuan City, Taiwan
2Hsin Sheng Junior College of Medical Care and Management, Taoyuan City, Taiwan
3Department of Pathology, Tri-Service General Hospital, National Defense Medical Center, Taipei City, Taiwan
4Department of Biomedical Engineering, Ming Chuan University, Taoyuaan City, Taiwan
*Corresponding Author: Junn-Liang Chang, MD. PhD, 32551, No. 168, Chung-Shing Rd., Long-Tang District, Taoyuan City, Taiwan
Received: 31 March 2021; Accepted: 09 April 2021; Published: 20 April 2021
Article Information
Citation: Kuang-Ting Liu, Yueh-Ching Chang, Yu-Chieh Lin, Junn-Liang Chang. An Unusual Metastatic Signet-ring Cell Carcinoma of the Rectosigmoid Colon Presenting as Mandibular Tumor in a Female patient: A Case Report and Review of the Literature. Journal of Cancer Science and Clinical Therapeutics 5 (2021): 201-209.
View / Download Pdf Share at FacebookAbstract
Background: Metastatic adenocarcinomas of the colon to the oral cavity are very uncommon, especially signet-ring cell carcinoma (SRCC) is relatively extremely rare, and constitutes about 1% of all oral malignancies.
Case Presentation: A 54-year-old female who had been diagnosed with SRCC of the rectosigmoid (RS) colon with peri-colic nodal metastasis after initial low anterior resection (LAR). Then, she has performed completely 12 cycles of palliative adjuvant chemotherapy. Two years later, she presented a progressively swelling painful mass in the right mandible and incisional biopsy was performed. Histopathology examination demonstrated metastatic SRCC of the RS colon to the right mandible bone diagnosed in an incisional biopsy. Three months after the definite diagnosis of the right mandibular lesion, she died of the disease because she represented an incurable disseminated disease.
Keywords
<p>Metastatic adenocarcinoma; Rectosigmoid colon; Signet-ring cell carcinoma; Mandible; Chemotherapy</p>
Article Details
1. Introduction
Primary signet ring cell carcinoma (SRCC) of the colorectum is an uncommon subtype of mucinous adenocarcinoma, accounting less than 1% of all colorectal cancers [1-5]. The metastatic colorectal adenocarcinoma (MCRA) especially SRCC to oral cavity or mandible is very rare. Metastatic oral tumors are uncommon, contributing to 1% of total reported malignant tumors in the oral cavity [2-7]. MCRA is commonly related to widespread malignancy and poor survival rates. Usually, oral metastases spread from major organs, including breasts, lungs, kidneys, bones, colon, liver, and prostate [2-4, 8-10].
The most common site of oral metastasis is the mandibular jawbone [5-8]. The high incidence of anatomical sites may be related to extensive vast vascularization. Patients with MCRA exhibits a wide range of clinical features can be presented including swelling, pain and paresthesia as in our case. We describe a case who was investigated a metastatic mandibular mass from primary SRCC of the colon after initial LAR and developed advanced multiple bony metastasis. Previous documents have been proposed the diagnostic and management strategies for this unusual presentation patient with advanced disease and poor prognosis, and investigators also have considered that the following therapeutic strategic role of radiation therapy, chemotherapy, or both in this setting is still uncertain.
2. Case Presentation
A 54-year-old female was complained of passage of tarry stool for months. She visited at local medical clinic and received colonoscopy with biopsy. The pathological diagnosis confirmed adenocarcinoma of the sigmoid colon. And the she was referred to our hospital and admitted to the Colo-Rectal Surgery (CRS) Division for further evaluation and treatment. She has hypertension with HCVD development with regular treatment. Physical examination, vital signs showed stable, abdomen was soft and ovoid with no tenderness, and no others significant abnormal findings. Laboratory findings showed Hg was 9.6 g/dl, tumor markers CEA was 159 ng/mL, CA199 was 48 U/mL. The chest-x ray film showed no abnormal finding. The CT scan without contrast of the abdomen and pelvis (Figure 1) revealed asymmetric wall thickening, peri-focal fatty stranding, and regional lymph nodal enlargement over the RS colon. Adenocarcinoma of RS colon was highly considered. She underwent a low anterior resection for RS cancer.
2.1 Histopathological findings
Grossly, the surgical resected RS colonic tissue showed an irregular, annular, diffuse fungating/ exophytic ulcerative plastica-like lesion measured 4 by 4 by 1 cm with deeply to subserosa involvement. Histopathologically, serial sections revealed SRCC (Figure 2A-B) composed of neoplastic cells infiltrative growing patterns, massive mucin-pools formation with proliferation of signet ring cells with intracellular mucin that displaces nucleus to side of marked signet-ring cell differentiation invaded through muscularis propria into pericolorectal tissues. The pericolic dissected lymph nodes revealed metastatic adenocarcinoma.
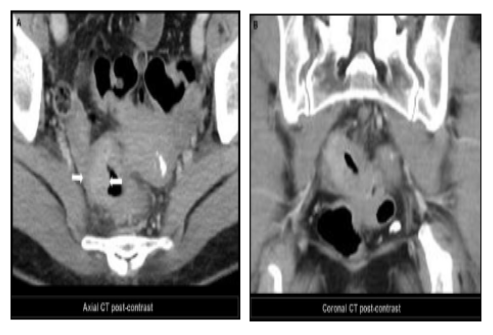
Figure 1: Representative photographs of the CT scan of the pelvis with contrast displays asymmetrical wall thickening (A, arrow), peri-colic fatty stranding, and regional lymph node enlargement at the recto-sigmoid colon (B).
IHC study, these tumor cells demonstrated positive immunoreactivity for pan-CK, CEA, MUC-1, CK20 (Figure 2C), and CDX2 (Figure 2D), but negative for CK7, TTF1, and GCDFP-15. Microsatellite instability (MSI) analysis for MMR proteins was performed that demonstrated positive immunostaining for MLH1, MSH2, MSH6 and PMS2 expression. The morphological characteristics of poorly differentiated adenocarcinoma of the RS colon with > 50% sig-net ring cells, and the pathological diagnosis was SRCC with pericolic nodal involvement with pathological TMN stage, 8th AJCC, pT3N1bM0, Sage IIIb. Then, she has performed completely scheduled courses of 12 cycles of palliative adjuvant chemotherapy with no evidence of tumor recurrence and regularly follow-up at our CRS Division.
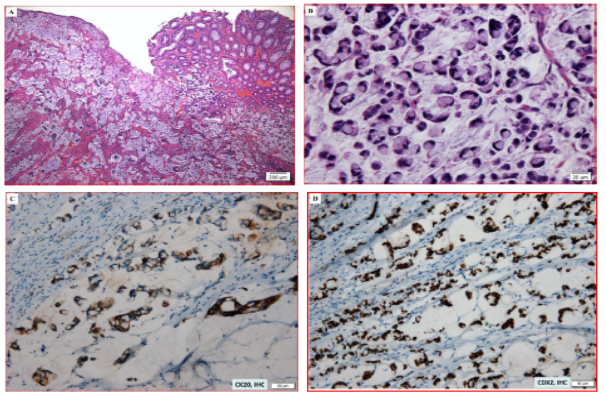
Figure 2: Representative photographs of the histological sections of the primary resected RS colon. The hematoxylin and eosin (H&E) shows the diffusely growth of signet-ring cell carcinoma (SRCC) (A, H&E, original magnification x 4). These SRCC cells display diffusely monotonous infiltration (B, H&E, original magnification x 40). The IHC staining illustrates strongly positive staining for CK20 for signet-ring cells (C, original magnification x 20), and positive nucleus level for CDX2 (D, original magnification x 20).
Unfortunately, she developed a progressive swelling with painful mass over the right mandibular region initial surgery 20 months later. Then an incisional biopsy of the mandibular mass was performed. The histopathology and immunohistochemical (IHC) examination exhibited the characteristics as metastatic SRCC of the RS colon to the right mandible bone was diagnosed (Figure 3A-B). The metastatic tumor cells with IHC staining demonstrated strongly positive immunoreactivity for pan-CK, CK18, CK20 (Figure 3C), CDX2 (Figure 3D), CEA, Muc-1 and presented proliferative index Ki-67 more than 60% involving tumor cells. These tumor cells illustrated negatively immunostaining for CK7, CK14, HepPar-1, GCDFP-15 and TTF1. Taken together, based on histopathologic and IHC analysis, the poorly differentiated metastatic adenocarcinoma was diagnosed and suggestive of metastatic SRCC of the RS colon was firstly considered.
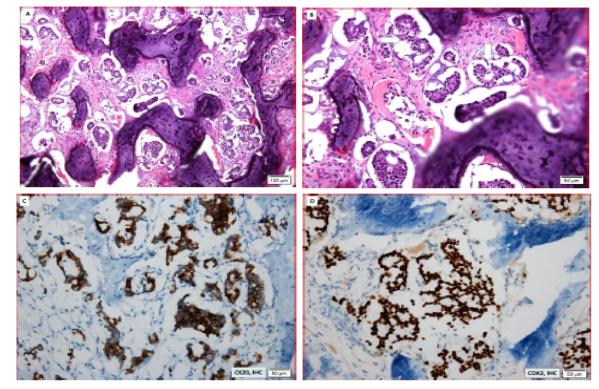
Figure 3: Photographs of the histological sections of metastatic carcinoma to the right mandibular bone. The metastatic adenocarcinoma cells with H&E stain reveals marked destructive bony trabeculae infiltration by metastatic sig-net-ring cell carcinoma (A, H&E, original magnification x10) and obscure tubular-glandular architectures (B, H&E, original magnification x 20), Representative photomicrographs of IHC examination demonstrates strongly positive immunostaining for CK20 (C, original magnification x 20), and at the nucleus expression for CDX2 (D, original magnification x 20).
The postoperative clinical course was uneventful and no adjuvant chemotherapy was performed. To confirm a definite diagnosis, biopsy and imaging studies were also undertaken. The MRI of spines displayed multiple pathological compression fractures at T7, T9, T11, L1-2 levels and suggestive of bony metastasis (Figure 4). Unfortunately, she died of the cancer two years after initial LAR due to incurable recurrent and disseminated bony metastasis.
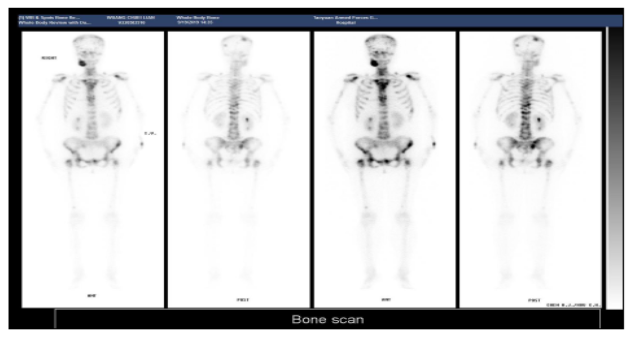
Figure 4: Photographs of a scintigraphy of bone scan with injection of TC-99m MDP analysis depicts multiple metastatic lesions in the skull, right mandible, bilateral glenoids and humeri, sternum, rib cage, T-L spines, right SI joints, bony pelvis, and bilateral femurs.
3. Discussion
Colorectal cancer is one of the most common malignant tumors in the worldwide. Primary colorectal SRCC is a rare variety characterized by distinctive signet ring morphology, was first reported in 1951, with an estimated incidence about 0.1-2.4% [1-4]. Colorectal SRCC should be a primary origin in the colon or rectum constitute of 0.7%-1%, with more frequently in females age 48 to 70 years. The SRCC most frequent involve the stomach (96%), followed by the colon, rectum, gallbladder, pancreas, and bladder. The SRCC histomorphology make up to at least 50% of the tumor part with signet ring cell pattern to confirm the diagnosis. Colorectal SRCC represents on late and is associated with high-grade characteristics of aggressiveness. Primary SRC cancer of the colon appears predominantly in the rectum (32.9%), followed by the sigmoid colon (20.4%), the cecum (11.2%) and the ascending colon (10.5%) [6-7]. Previous studies have been postulated that the colorectal SRCC is a factor of poor survival rate, regardless of comorbidity or tumor extension as was shown in the present case.
Colorectal SRCC is diagnosed at a more advanced stage with widespread transmural extension, regional lymph node metastases and peritoneal dissemination and high risk of death. SRCC common sites of metastasis include the regional lymph nodes, liver, lungs, cutis, vagina, myocardium, breast, and prostate. The rate of liver metastases has been seen in 2.9%–14.3% and bone metastases from colorectal cancer are approximately 4.7 % to 10.9%. Colorectal SRCC with diffuse bone metastases estimate about 1-2%. The average age of oral metastasis is 50-60 years old, but it may occur at any age, and there is no significant gender difference [9]. Irani et al. [9-10] have investigated 453 metastatic cases with a male to female ratio of 1.2:1, and the average age was 53.4 years. Considerable hematopoietic active bone marrow is an attractive site of metastasis. The most common clinical symptoms and signs of oral metastases could be asymptomatic or may induce tumors, pain, ulcers, paresthesia, bleeding, periodontitis, trismus, anesthesia and paresthesia or pathological fracture. The primary SRCC in women is usually originated from the breasts, reproductive organs, thyroid gland, and kidneys, whereas in men it is found in the lungs, prostate, kidneys, bones, large intestine, and suprarenal glands [9-10].
In addition, the diagnoses of an oral metastatic tumor and primary colon cancer were often synchronous and were frequently accompanied with metastases to other organs. It is recommended that several key aspects that should be considered when diagnosing colon cancer patients, including focusing attention to oral symptoms when examining cancer patients, adopting a multidisciplinary approach for differential diagnosis and using postoperative pathological examination to accurately diagnose the tumor type and optimize curative effects [11-12].
The immunophenotypic markers of the colorectal SRCC include cytokeratin 20 (CK20), CK7 and CDX2. Therefore, the immunostaining pattern of CK20 is positive, while the immunostaining pattern of CK7 is negative. Cytokeratin CDX2 is usual expressed in enteric differentiation and positive in most cases [13-17]. IHC analysis is a well-documented evaluation of the expression coordinates CK7 and CK20, which can assist recognize and distinguish the primary locations of metastatic carcinomas including breast, ovarian, and lung primaries (usually CK7+/CK20-), as well as colorectal primaries (usually CK7-/CK20+) [18-21]. CDX2 is a sensitive and specific maker for colorectal cancer. CDX2 expression has also been shown in some adenocarcinomas cause by the colon, rectum, stomach, and esophagus. In additionally, CK7, CK20, and CDX2 may be applied to the diagnosis of gastrointestinal metastatic tumors [1, 19-21].
The degree of the primary tumor and metastatic spread is the important factors in predicting survival rate and therapeutic strategy. Previously, the treatment of metastatic lesion should be included by radiation, chemotherapy, surgical resection, or a combination of these techniques. Palliative treatment helps in reducing the patient's pain, size of tumor, and also preserves oral function. The median survival and average survival of patients with mandible metastases were 12 months and 27.7 months, respectively [11, 22]. Metastatic SRCC from the RS colon to the oral cavity are extremely rare frequently indicative of an advanced-stage disease associated with poor survival rates. So that should be considered in the differential diagnosis of a synchronous or metachronous origin of oral cavity tumors. Early detection and management of oral cavity metastasis may be palliative alternatives aimed at improving the patient's quality of life and prolong survival [9,10,23].
4. Conclusion
In summary, mandibular metastasis is usually a sign of disseminated malignant tumors and with poor prognosis and can be used for palliative therapy. Patients with oral metastatic tumors, because they have already wide spread to other sites, they have very poor chemotherapeutic response with a poor survival. We herein describe a 54-year-old female with a history of SRCC of the RS colon and multiple bony metastasis was referred to our hospital with a chief complaint of progressive swelling and painful mass in the right mandible was included in the differential diagnosis. Therefore, the correct radiographic diagnosis became difficult. Ultimately, histologic evaluation is necessary to make a definitive diagnosis. The management of metastatic lesions is still a controversial issue, and the development of new specific markers of gastrointestinal differentiation may promote early diagnosis.
Acknowledgements
The authors thank Dr. Yen-Lin Chen of the Department of Radiology for providing the medical images and explanations of the present case.
Conflicts of Interest
The authors declare no conflict of interest.
Declaration
The authors have no support or funding.
References
- Álvarez-Álvarez C, Iglesias-Rodríguez B, Pazo-Irazu S, et al. Colonic adenocarcinoma with metastasis to the gingiva. Med Oral Pathol Oral Cir Bucal 11 (2006): E85-87.
- Van der Waal RIF, Buter J, Van der Waal I, et al. Oral metastases: report of 24 cases. Brit J Oral Maxilofacial Surg 41 (2003): 3-6.
- Hirshberg A, Buchner A. Metastatic tumors to the oral region. An overview. Eur J Cancer B Oral Oncol 31B (1995): 355-360.
- Thota R, Fang X, Subbiah S. Clinicopathological features and survival outcomes of primary signet ring cell and mucinous adenocarcinoma of colon: Retrospective analysis of VACCR database. J Gastrointest Oncol 5 (2014): 18-24.
- Pelissari C, Cavalcanti D, Braz-Silva PH, et al. Metastatic colorectal adenocarcinoma in oral cavity: case report and literature review. J. Oral Diag 03 (2018): e20180014.
- Pande R, Sunga A, Levea C, et al. Significance of signet-ring cells in patients with colorectal cancer. Dis Colon Rectum 51 (2008): 50-55.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, et al. Metastatic tumours to the oral cavity - pathogenesis and analysis of 673 cases. Oral Oncol 44 (2008): 743-752.
- Mora-Guzmán I, Di Martino M, Mu˜noz de Nova JL, et al. Primary signet ring cell carcinoma of the colon: A rare condition with a poor prognosis. A report on two Cases. Revista de Gastroenterología de México 83 (2018): 358-360.
- Irani S. Metastasis to the oral soft tissues: A review of 412 cases. J Int Soc Prevent Communit Dent 6 (2016): 393-401.
- Irani S. Metastasis to the Jawbones: A review of 453 cases. J Int Soc Prevent Communit Dent 7 (2017): 71-81.
- Owosho AA, Xu B, Kadempour A, et al. Metastatic solid tumors to the jaw and oral soft tissue: A retrospective clinical analysis of 44 patients from a single institution. J Craniomaxillofac Surg 44 (2016): 1047-1053.
- Ren QG, Huang T, Yang SL, et al. Colon cancer metastasis to the mandibular gingiva with partial occult squamous differentiation: A case report and literature review. Mol Clin Oncol 6 (2017): 189-192.
- Andabak Rogulj A, Tomasovic Loncaric C, Muller D, et al. Solid malignant metastases in the jaw bones. Br J Oral Maxillofac Surg 56 (2018): 705-708.
- Hadhri A, Abidi R, Ben Rejeb M, et al. Metastasis of colon adenocarcinoma to the mandible: A case report. Tunis Med 98 (2020): 518-521.
- Dalirsani Z, Mohtasham N, Samiee N. Metastasis of Colon Adenocarcinoma to Maxillary Gingiva and Palate. Iran J Otorhinolaryngol 32 (2020): 327-331.
- Fleming M, Ravula S, Tatishchev SF, et al. Colorectal carcinoma: Pathologic aspects. J Gastrointest Oncol 3 (2012): 153-173.
- Chu PG, Weiss LM. Keratin expression in human tissues and neoplasms. Histopathology 40 (2002): 403-439.
- Pelissari C, Cavalcanti D, Braz-Silva PH, et al. Metastatic colorectal adenocarcinoma in oral cavity: case report and literature review. J Oral Diag 3 (2018): e20180014.
- Meer S, Altini M. CK7+/CK20- immunoexpression profile is typical of salivary gland neoplasia. Histopathology 51 (2007): 26-32.
- Li MK, Folpe AL CDX-2, a new marker for adenocarcinoma of gastrointestinal origin. Adv Anat Pathol 11 (2004): 101-105.
- Watanabe M, Tada M, Satom T, Chikazu D, et al. Metastatic rectal adenocarcinoma in the mandibular gingiva: a case report. World J Surg Oncol 14 (2016): 199.
- Kende AI, Carr NJ, Sobin LH. Expression of cytokeratins 7 and 20 in carcinomas of the gastrointestinal tract. Histopathology 42 (2003): 137-140.
- Neumann ED, León Vintró X, Vega García C, Quer Agustí M. Oral cavity colon adenocarcinoma metastases: case report with surgical approach and review of more than 30 years literature. Oral Maxillofac Surg 25 (2021): 99-101.


 Impact Factor: * 4.1
Impact Factor: * 4.1 Acceptance Rate: 74.74%
Acceptance Rate: 74.74%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 