Erythrocytosis As A Paraneoplastic Syndrome in A Case of Angiosarcoma
Caroline Hana1*, George Hanna2, Atif Hussein3
1PGY-4, Hematology/oncology fellowship, Memorial Healthcare system, 703 N Flamingo Road, Pembroke Pines, FL, USA
2Third year medical student, NOVA southwestern university, College of Osteopathic medicine 3200 S University Dr, Davie, Fl, 33328, USA
3Medical Director, East Operations-Adult Hematology & Oncology, Director, Hematology & Oncology Fellowship Program, Memorial Healthcare system, 1150 North 35th Avenue, suite 330, Hollywood, FL 33021, USA
*Corresponding Author: Caroline Hana, PGY-4, Hematology/oncology fellowship, Memorial Healthcare system, 703 N Flamingo Road, Pembroke Pines, FL, USA.
Received: 20 March 2022; Accepted: 11 April 2022; Published: 13 June 2022
Article Information
Citation: Caroline Hana, George Hanna, Atif Hussein. Erythrocytosis As A Paraneoplastic Syndrome in A Case of Angiosarcoma. Journal of Cancer Science and Clinical Therapeutics 6 (2022): 239-243.
View / Download Pdf Share at FacebookAbstract
Angiosarcoma is a rare form of sarcoma that is rarely associated with paraneoplastic syndromes. Its association with increased Erythropoietin (EPO) secretion has only been reported in one case. We report the case of a 73-yearold female patient presenting with a mass on the parotid gland, which was identified to be an angiosarcoma, demonstrated through biopsy and Positron Emission Tomography (PET) scan. The laboratory studies demonstrated elevated hemoglobin and hematocrit levels, with a markedly increased serum erythropoietin level. The workup for primary polycythemia was negative. The patient was treated with immediate phlebotomy on 3 occasions and then started paclitaxel, initially alone and then in combination with external beam radiation therapy for the angiosarcoma. After 8 weeks of the initiation of chemotherapy alone, the patient's hemoglobin and erythropoietin levels normalized. The repeat PET scan after the third cycle of paclitaxel showed a mixed response with improved size of the mass but increased intensity probably a reflection of the inflammatory response from chemotherapy. These findings suggest that the patient's polycythemia was secondary to increased erythropoietin secretion from her angiosarcoma.
Keywords
<p>Angiosarcoma; Paraneoplastic syndrome; Erythropoietin secreting tumor; Erythrocytosis</p>
Article Details
1. Introduction
Malignant tumors present in many ways, one of them is paraneoplastic syndromes. Paraneoplastic syndromes are disorders that develop when a tumor secretes hormones, peptides, or cytokines or from immune cross-reactivity between malignant and normal tissues. This, in turn, may affect diverse organ systems, most notably the endocrine, neurologic, dermatologic, rheumatologic, and hematologic systems, hence, producing a variety of clinical syndromes. Examples of these syndromes include, but not limited to, humoral hypercalcemia of malignancy, Cushing syndrome, and Syndrome Of Inappropriate Anti-Diuretic Hormone Secretion (SIADH). The most commonly associated malignancies include small cell lung cancer, breast cancer, gynecologic tumors, and hematologic malignancies [1]. These disorders can either precede, occur concurrently with, or follow the diagnosis of a neoplastic disease. They often represent the first clinical sign of an underlying neoplasm or the earliest symptom of relapse of a previous cancer [2]. Angiosarcoma is one of the rare soft-tissue sarcomas that arise from the vascular endothelium, arising either as a primary tumor or secondary to other causes, such as radiation therapy. It comprises 1% of all soft-tissue sarcoma [3, 4]. Angiosarcoma has rarely been associated with paraneoplastic syndromes. Some of the reported cases included the association with opsoclonus myoclonus syndrome, limbic encephalitis, and some cutaneous syndromes for example eruptive seborrheic warts [5-7]. Only one case has reported the association between angiosarcoma of the liver with erythrocytosis secondary to EPO secretion [4]. The only other case reporting a similar syndrome happened in a cat diagnosed with splenic hemangiosarcom.[8].
2. Case Report
We report a case of a 73-year-old female, never smoker, previously healthy, who presented to the Ear, Nose and Throat (ENT) office complaining of a 2-month history of left-sided swelling of her face. She was found to have swelling of left parotid gland, which was hard, non-tender, fixed to deep tissues and of approximately 8 x 6 cm. She underwent Magnetic Resonance Imaging (MRI) of the neck which was positive for a large lobulated enhancing mass centered within the deep lobe of the left parotid gland and extending anteriorly into the left carotid jugular neurovascular space, and posteriorly to involve the left sternocleidomastoid measuring 6.1 x 5.3 x 4.2 cm. A Computed Tomography Arteriogram (CTA) showed that the mass had trans-spatial extension and complete encasement of the carotid system at the level of the bulb and origins and proximal segments of the internal and external carotid arteries which remain patent distally, and of the left vertebral artery. It also showed a small metastatic left neck levels III/IV lymph nodes. Multiple non-calcified sub-centimeter nodules of the lung apices suspecting metastatic disease. She then underwent biopsy of the mass which showed fibrous tissue and skeletal muscle diffusely infiltrated by a poorly differentiated malignant neoplasm, no salivary gland tissue was visualized. The tumor cells were variably spindled, polygonal or more epithelioid and showed focally notable nuclear pleomorphism and hyperchromasia. Immunostains showed diffuse nuclear positivity for ERG (an Erythroblasts Transformation-Specific family transcription factor known to be expressed in endothelial cells) along with focal weaker positivity for CD31 and diffuse positivity for D2-40, while pan-keratin, CK5, SOX10 and CD34 are negative.
Findings were consistent with angiosarcoma which was morphologically of a high grade. Positron Emission Tomography (PET) scan performed showed large hypermetabolic left neck mass and adjacent level II/V node. Multiple bilateral low-grade pulmonary nodules, highly concerning for metastatic disease. Upon evaluation of the patient’s blood counts, she was noted to have a hemoglobin of 19.9 g/dL with a hematocrit of 61.4%. Her White Blood Cell (WBC) count was 6.9 x 1000/uL and her platelets were 217 x 1000/uL. Other blood work was obtained to delineate the cause of her polycythemia, this included iron studies which showed iron level of 143 ug/dL, Total Iron Binding capacity (TIBC) 360 ug/dL, iron saturation of 40% and a ferritin level of 124 ng/mL. Her serum erythropoietin level was found to be significantly elevated at 75.9 mIU/mL (normal range 2.6-18.5 mIU/mL). Peripheral blood Next Generation Sequencing (NGS) was negative for JAK2 exon 12, JAK 2 V617F, CALR and MPL mutations. The patient was started on treatment with phlebotomy for her polycythemia as well as weekly paclitaxel at 80 mg/m2 for her angiosarcoma followed by concurrent paclitaxel with external beam radiation to the left neck mass.
2.1. Outcome
At the end of cycle 2, i.e. 8 weeks after starting chemotherapy, her repeat labs showed hemoglobin decrease to 12.1 g/dL with WBC count of 5.1 K/uL and platelets of 295 K/uL. Her repeat EPO level was 2.5 mIU/mL. She underwent phlebotomy only 3 times then her counts normalized. A repeat PET scan after cycle number 3 showed a mixed response with decreased extent of metabolic activity associated with infiltrative left neck angiosarcoma; however, the intensity had increased, which is probably reflective of the inflammatory response from chemotherapy and the nature of the malignancy being that of blood vessels (Figure 1). The PET scan also showed cavitation of the lung metastases suggesting improvement; but a new 7 mm nodule in the posterior left lower lobe was noted. These findings suggest that this patient had a polycythemia secondary to increased erythropoietin secretion by her angiosarcoma. The patient continued weekly dose reduced paclitaxel treatment (50mg/m2) along with radiation to the left neck mass (a total of 5000 cGy over 25 sessions). NGS testing on the biopsy obtained at diagnosis showed that the tumor is programmed cell death lignand-1 (PD-L1) (SP142) 3+ positive, 100% by immunohistochemistry. It was also microsatellite stable, mismatch repair status proficient, and no fusion of NTRK1/2/3 was detected. Other mutations detected were POT1 pathogenic variant Exon 13 p.R363*, TP53 pathogenic variant exon 6 c.672+1G>T, and CRKL CAN-seq amplified. Genomic loss of heterozygosity Seq DNA high 24% of tested genomic segments exhibited LOH threshold > 16%. After her chemoradiation course, the patient was noted to have complete resolution of her mass by physical exam. At the time of this case report, a PET scan is pending do decide regarding starting pembrolizumab since her tumor exhibited 100% positivity for PD-L1.
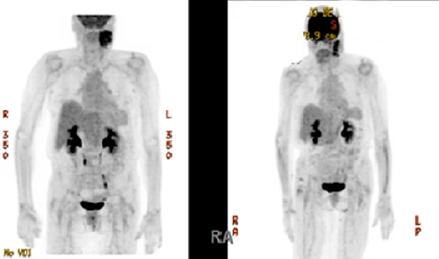
Figure 1: Pet scans before (left side) Vs after (right) treatment showing improvement in the size of the left parotid mass .
3. Discussion
This is a very interesting case of a paraneoplastic syndrome. Our patient had an increased level of serum EPO secondary to her angiosarcoma. EPO is a glycoprotein that promotes the proliferation and differentiation of erythrocyte precursors, which are needed in order to maintain red blood cell mass.(9) It is primarily secreted endogenously by the kidney followed by the liver and its production increases in response to the stress of anemia or hypoxemia.(10) Polycythemia secondary to increased EPO levels has been reported as a paraneoplastic syndrome in cases of renal cell carcinoma, hemangioblastoma and hepatocellular carcinoma (HCC) [11,12]. Interestingly, in a study by Kew & Fischer, the level of EPO hormone in patients with HCC was noted to be elevated in 23% of cases. This, however, did not always correlate with an elevated level of hemoglobin and polycythemia, which raises the question about the biological activity of the EPO secreted by these tumors [10,13]. In our case, however, the elevated level of EPO was reflected into polycythemia and elevated hemoglobin level. Angiosarcoma is rarely associated with paraneoplastic syndromes. Very few case reports highlighted its association with hematologic syndromes. In 1982, Rothmann et al reported the only human case of EPO secretion by a hepatic angiosarcoma [4]. Extreme leukocytosis was also reported in a 74-year-old patient, whose autopsy showed an angiosarcoma, also, in the liver [14]. Unlike these two cases with angiosarcoma of the liver, our patient’s angiosarcoma was found to be in the parotid gland, an organ that is not related to EPO secretion or hematopoiesis. This, in turn, adds to the rarity of this condition.
4. Conclusion
Angiosarcoma can be associated with erythrocytosis secondary to paraneoplastic EPO secretion. Paraneoplastic EPO secretion improves with the tumor response to treatment. It should be suspected in patients with angiosarcoma and erythrocytosis. It is also important to rule out other causes of erythrocytosis before making the diagnosis of paraneoplastic syndrome.
References
- Pelosof LC, Gerber DE. Paraneoplastic syndromes: an approach to diagnosis and treatment. Mayo Clin Proc 85 (2010): 838-854.
- Zappasodi P, Del Forno C, Corso A, et al. Mucocutaneous paraneoplastic syndromes in hematologic malignancies. International Journal of Dermatology 45 (2006): 14-22.
- Spiker AM, Mangla A, Ramsey ML. Angiosarcoma. StatPearls. Treasure Island (FL) (2021).
- Rothmann SA, Savage RA, Paul P. Erythropoietin-dependent erythrocytosis associated with hepatic angiosarcoma. J Surg Oncol 20 (1982): 105-108.
- Rubegni P, Feci L, Fimiani M. Three simultaneous paraneoplastic skin manifestations in a patient with renal angiosarcoma. Clin Exp Dermatol 39 (2014): 553-554.
- Periasamy K, Das N, Khosla D, et al. Recurrent angiosarcoma of scalp with opsoclonus myoclonus syndrome: role of salvage treatment. BMJ Case Rep 14 (2021).
- Wagner-Altendorf TA, Wandinger KP, Frydrychowicz A, et al. Anti-Amphiphysin-associated limbic encephalitis in a 72-year-old patient with aortic angiosarcoma. BMJ Case Rep 12(2019).
- Seo KW, Hong H, An SA, et al. Secondary inappropriate polycythemia with splenic hemangiosarcoma in a young adult cat. Can Vet J 59 (2018): 1320-1324.
- Adamson JW. Regulation of red blood cell production. Am J Med 101 (1996): 4s-6s.
- Gaballah AH, Jensen CT, Palmquist S, et al. Angiosarcoma: clinical and imaging features from head to toe. Br J Radiol 90 (2017): 20170039.
- Villanueva-Gimeno MM, Vicario-Bermudez JM, Fonseca-Lopez C, et al. [Renal cell carcinoma producing erythrocytosis due to inappropriate production of erythropoietin]. Semergen 39 (2013): 282-284.
- Feng CC, Ding GX, Song NH, et al. Paraneoplastic hormones: parathyroid hormone-related protein (PTHrP) and erythropoietin (EPO) are related to vascular endothelial growth factor (VEGF) expression in clear cell renal cell carcinoma. Tumour Biol 34 (2013): 3471-3476.
- Kew MC, Fisher JW. Serum erythropoietin concentrations in patients with hepatocellular carcinoma. Cancer 58 (1986): 2485-2488.
- Halkes CJ, Dijstelbloem HM, Eelkman Rooda SJ, et al. Extreme leucocytosis: not always leukaemia. Neth J Med 65 (2007): 248-251.


 Impact Factor: * 4.1
Impact Factor: * 4.1 Acceptance Rate: 74.74%
Acceptance Rate: 74.74%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 