Male Medical Circumcision for the Control of Human Immunodeficiency Virus by Nurses using the Unicirc® Assist Device
Norman D Goldstuck
Department of Obstetrics and Gynaecology, Faculty of Medicine and Health Sciences, University of Stellenbosch, Francie van Zyl Dr, Tygerberg Hospital, Bellville, Cape Town 7505, South Africa
*Corresponding author: Norman D Goldstuck, Department of Obstetrics and Gynaecology, Faculty of Medicine and Health Sciences, University of Stellenbosch, Francie van Zyl Dr, Tygerberg Hospital, Bellville, Cape Town 7505, South Africa.
Received: 30 October 2023; Accepted: 07 November 2023; Published: 06 December 2023
Article Information
Citation: Norman D Goldstuck. Male Medical Circumcision for the Control of Human Immunodeficiency Virus by Nurses using the Unicirc Assist Device. Journal of Biotechnology and Biomedicine. 6 (2023): 579-584.
DOI: 10.26502/jbb.2642-91280120
View / Download Pdf Share at FacebookAbstract
Objective: To demonstrate that male medical circumcision can be performed and evaluated by nurse practitioners using the Unicirc circumcision assist device.
Methods; Thirty nurses were trained to carry out circumcisions by learning how to perform them on a Unicirc training module before performing them under supervision and finally independently. They were also taught to assess circumcision related complications and how to identify absolute contra-indications for performing the procedure. The no-needle, no-suture approach using topical anaesthesia was used wherever possible. The subjects were males aged from one week to 66 years who requested circumcision for hygiene purposes, disease prevention or religious reasons. Results: The nurses performed 221 circumcisions. The mean age of the subjects was 17.3 years and 74% were under 20. Those over 21 required the larger sized Unicircs. Circumcisions were performed mainly for religious reasons in the younger boys and for hygiene and disease protection in the older boys ang men. The boys under 10 required local anaesthetic in addition to topical. Some 21 subjects required dilatation of the prepuce, 28 required a dorsal slit procedure and 5 required a frenulectomy. There were 5 cases of wound dehiscence which were managed conservatively with complete resolution. The patients who attended for follow-up were all extremely satisfied with the procedure.
Conclusion: Nurses can rapidly be taught to perform circumcisions with the Unicirc assist device and consideration should be given to teaching medical surgical technicians as well.
Keywords
Nurses; Circumcision; Unicirc; Topical; Local; Anaesthetic
Article Details
Introduction
The last few years have seen a lot of attention on the viral pandemic caused by Covid-19. Most other infectious and viral diseases have been in its shadow. The Human Immunodeficiency Virus (HIV) continues to cause morbidity and mortality some forty odd years after its identification. It is especially prevalent in sub-Saharan Africa where it is spread largely by heterosexual sexual transmission [1]. Following the observation that the incidence of HIV was lower in parts of Africa which practiced circumcision compared to those that did not [2], three randomized controlled trials (RCTs) were conducted which indicated that circumcision was about 60% effective in reducing male HIV rates [3-5]. Hopefully this should also prevent heterosexual spread of HIV to the female population as well. The probable mechanism for decreased HIV infection is the removal of the Langerhans cells in the foreskin which can become HIV infected [6] and subsequently pass the virus into the systemic circulation. Male circumcision using surgical techniques, usually the dorsal slit method is both time consuming and costly. It also requires a degree of skill and training if problems are to be avoided. This is especially true in younger men who may have adhesions or an attached frenulum. The history of using some type of circumcision assist device for completion of circumcision for males of all ages goes back many years and has been well described by Morris and Eley [6]. Most of these devices, especially when used in adults work by creating necrotic tissue which may act as a nidus for infection. One of these newer devices, the Unicirc© (Kapasa Medical, Vienna, Austria) is non-necrotizing and does not require needles or sutures (Figure 1). It has been evaluated in clinical trials in both adults and children [7-9]. Previous studies of nurses performing circumcisions either using the dorsal slit method or using the now discontinued Prepex™ device have been reported [10]. The purpose of this study was to show that male circumcision could be completed safely and effectively by medical auxiliary personnel, mainly nurses, using the Unicirc method. This would help make mass circumcision programs to help prevent HIV in Africa more achievable and more economical. This evaluation was therefore designed to be completed in the kind of low-resource setting where it is anticipated that the device would largely be used.
Methods and Materials
Surgical Method
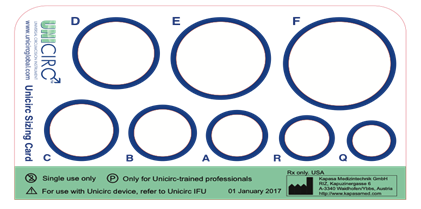
The Unicirc is a plastic and metal single-use only, disposable instrument designed in South Africa (Figure 1). It comes pre-packaged and gas sterilized and with all the additional disposable equipment which is needed including topical anaesthetic cream (EMLA), a surgical blade, curved forceps and tissue glue and the required dressings including Hypafix tape. There were seven different Unicirc sizes (diameters) used in this study: They are the available sizes designated A-F. and R. The dimensions are given in Table 1. The SA Medical Association’s Ethics Committee (SAMAREC) approved Unicirc for Phase IV (post-licensing) use (06 March, 2014). The Unicirc disposable devices were supplied by the manufacturer. The ClinicalTrials.gov identifier is NCT02593630. The work described has been carried out in accordance with ‘The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans’. The original data are available from Simunye Primary Health Care, Mitchells Plain, Western Cape, South Africa. Topical anesthesia is applied to the foreskin and is left in place for 25 minutes before the coronal circumference is measured with a sizing card (Figure 2) so that the appropriate Unicirc can be used. After 5 minutes of application of compression of the foreskin by the device it is excised and the wound sealed with cyanoacrylate tissue adhesive (iSeal™ (enbucrilate-n-butyl-2-cyanocrilate), IBC Pharmaceuticals Pvt, Ltd. Mumbai, India). Operative duration was timed from the and the wound covered with adherent tape (Hypafix). The technique has previously been described in great detail [9]. The technique of Unicirc circumcision can also be performed using local anaesthetic (a combination of lignocaine 1% and marcaine 0.5%) given directly or via a penile block which is more appropriate particularly if additional surgical procedures are contemplated at the same time, e.g. vasectomy [7]. For circumcision alone the use of topical lidocaine/prilocaine anaesthetic is preferable [7,8] but local anesthetic is often needed in the very young and additional sedation using diazepam or Ketamine for infants was sometimes needed. The study was conducted between January and August 2022.
|
Unicirc |
Diameter (mm) |
Circumference (mm) |
|
F |
32 |
100.52 |
|
E |
28 |
87.96 |
|
D |
24 |
74.76 |
|
C |
20 |
62.83 |
|
B |
18 |
56.54 |
|
A |
16 |
50.26 |
|
R |
14 |
43.98 |
|
Q† |
12 |
37.69 |
|
† - This size is too small and is no longer used |
||
Table 1: Unicirc type and size
Participants
Circumcision subjects
Healthy males of any age who requested voluntary medical circumcision, or whose guardian requested circumcision, were eligible. Informed consent was given by the subjects or by their guardian for those under 18 years of age. They were asked to give one of four reasons for requesting circumcision, including, ‘protection from disease’, ‘hygiene’ or ‘religious reasons’ or medical problem, eg phimosis. There was no specific minimum limit on the number of participants to be evaluated because 1) this technique had already been fully evaluated and there was no comparative group and 2) the numbers would be determined by each member of the auxiliary medical personnel acquiring sufficient experience to be allowed to perform them independently. It was expected that this would require the experience of performing 25-30 circumcisions so that the probability of doing one which was not perfectly straight forward would present itself. Circumcision with Unicirc is fully complete after the procedure is performed and similarly to wound suturing with absorbable suture there is no clinical need for follow up in the absence of complications. The Hypafix dressing can either be gently removed after seven days or preferably left on until it falls off. We requested that subjects follow up where possible so that we could get an indication of healing progress and complications in comparison to those of previous studies. The study was not funded for large scale follow up which was not the primary aim of the study. Those participants who elected to follow up after 7 days for a healing assessment and at 28 days, either in the clinic or by contact, were asked to give a satisfaction rating on a four point rating scale of 1) very satisfied, 2) somewhat satisfied, 3) somewhat dissatisfied, 4) very dissatisfied at the 28 day follow up visit. Healing was assessed by the circumcision surgeon at the same time for those who attended in person. Participants were also advised to return as soon as possible if they experienced bleeding, pain, discoloration or swelling as soon as possible.
Circumcision surgeons
The circumcision surgeons were nurses who were registered and eligible for independent practice as nurse practitioners who were able to perform minor surgical procedures such as wound suturing and insertion of intrauterine devices. Some had additional qualifications in midwifery and psychiatry. Fewer than 10% had previously had any involvement with circumcision even as an assistant. Initial training was on a model constructed by the manufacturers of Unicirc (Figure 3.) Each surgeon had to perform three circumcisions on the model before being considered to perform an initial supervised circumcision. After two to three supervised surgeries they were allowed to perform them independently if deemed competent. They were also taught to recognize and manage situations in which complications could arise as well as situations where circumcision is contra-indicated such as hypospadias.
Results
Seven nurse practitioners completed 221 circumcisions with each practitioner performing over 30 surgeries. Only 211 surgical report forms were completed in sufficient detail to be suitable for analysis. The circumcision subjects were from one week to 66 years of age. The mean age was 17.3 years (standard deviation 10.5) with a median of 14 years. Most of the subjects (74%) were under 20 and those over 40 were less than 10%. This is in keeping with the benefit profile of circumcision for HIV control. The relationship of Unicirc size, indication for requesting circumcision and the type of anaesthetic or anaesthetics used are given in Table 2. The numbers are not identical in each category because of partial missing data. These numbers were small and not of marked significance. The size of the Unicirc used increased with age as the subjects (and penile corona enlarged) so that by the age of 21 only the largest sizes, D, E and F were used. The size of the device used increased with age (Kruskal Wallis, p<0.0001). The reason given for circumcision by the subject or his guardian was significantly correlated with age. Religious reasons were the main indication in the pre-pubertal boys and disease protection in the teenage boys and older men (Analysis of variance, p=0.00257). Most of the boys under 10 years of age and almost all under the age of 5 years old required local anaesthetic injection in addition to the topical anaesthesia to counteract the pain resulting from the breakdown of adhesions tethering the foreskin to the glans.
|
Age |
N |
Unicirc size (n) |
Indication (n) |
Anaesthetic (n) |
|
0-10 |
40 |
a-13 b- 3 r-24 (40) |
disease protection- 6 hygiene -11 religion- 22 (39) |
topical- 1 local- 6 topical+local- 33 (40) |
|
11-20 |
122 |
a- 22 b- 8 c- 8 d- 23 e- 34 f- 17 r- 10 (122) |
disease protection- 32 hygiene- 62 religion- 25 (119) |
topical- 52 local- 2 topical+local- 66 (120) |
|
21-30 |
19 |
d- 3 e- 8 f-8 (19) |
disease protection- 3 hygiene- 13 religion-1 (17) |
topical- 17 topical+local- 1 (18) |
|
31-40 |
20 |
c- 1 e-10 f-9 (20) |
disease protection- 7 hygiene- 8 religion- 2 (17) |
topical- 17 local- 2 (19) |
|
41-50 |
8 |
f-8 (8) |
disease protection- 1 hygiene- 4 religion- 1 (6) |
topical- 8 |
|
51-66 |
2 |
f-2 (2) |
disease protection- 0 hygiene- 1 religion- 1 (2) |
topical- 2 |
Table 2: Unicirc use by age, indication and type of anaesthesia.
Complications
Circumcisions are often complicated by an adherent frenulum, adhesions or the need to dilate the prepuce. There were 21 subjects all aged 14 or less where the prepuce required dilating. There were 28 subjects of various ages requiring the performance of a dorsal slit. In 34 subjects under the age of 14 a combined prepuce dilatation and dorsal slit was required, while 5 frenulectomies were required prior to performing the circumcision. . Five subjects also had an early wound dehiscence which was treated conservatively.
Wound healing
Healing is usually fully completed around 14 days in those under 10 and by 28 days in adults. If there are no problems then by 5 days in children, and a week in adults healing should be progressing well. The patients who returned for healing assessment and for complications are shown in Table 3. All of those who were asked for a satisfaction rating gave the procedure a ‘very satisfied’ rating.
|
Age |
1-7 days (n) |
8-15 days (n) |
16-27 days (n) |
28 days (n) |
Satisfaction† (n) |
Complications |
|
0-10 |
9 |
8 |
0 |
6 |
6 |
one needed antibiotics at 10 days |
|
11-20 |
5 |
21 |
0 |
37 |
37 |
wound disruption (3) healed after 28 days |
|
21-30 |
1 |
4 |
0 |
15 |
15 |
wound disruption (2) |
|
31-66 |
2 |
4 |
25 |
25 |
one delayed healing after 28 days in a diabetic subject |
† Total of ‘very satisfied’ at 28 days
Table 3: Healing at various times and complications after circumcision.
Discussion
The foreskin probably evolved because males with a foreskin were only able to reproduce relatively later in life. This provided a selective advantage in bringing their offspring to adulthood [6]. The possession of a foreskin turned deadly when it became adherent after infections and obstructed urinary flow. Before the antibiotic era circumcision could thus be lifesaving. The concept of the foreskin being ‘unhealthy’ evolved so that it became advocated for health as well as for religious reasons. Once the health issues related to the presence of a foreskin subsided, circumcision became a type of ‘mutilation’ in the opinion of some. Circumcision is once again a health issue in Africa following discovery of its role in heterosexual HIV transmission [2]. This may be true even in developed countries [11]. The pathology seems to be that infected T cells pass the virus on to Langhans cells in the foreskin and they are then passed on to dermal cells through the non-keratinized mucosal surface. These dermal cells then enter the circulation. The keratinized skin left behind after circumcision appears impervious to the passage of infected T-cells so that they do not come into contact with the Langans cells [12].
There have been many attempts to make a surgical assist device to make the procedure faster, safer, simpler and more economical. There are 2 types of device, 1) those which assist the surgery like the prototype, viz; the Gomco™ clamp and 2) those which adhere to the foreskin and must be removed later after having produced a necrotic reaction and which then subsequently rely on secondary intention healing to heal the area from which the foreskin has been removed. The latter have fallen into disrepute because of infection related problems, including gangrene. The Unicirc is a surgical assist device which is relatively simple to use. This study demonstrates that nurses can adequately perform the procedure independently after only a few days of training on models and then under initial supervision. The follow up numbers are small because patients who have a Unicirc circumcision do not normally require a follow up if they follow basic hygiene procedures and refrain from sexual intercourse, even with condoms, for at least 3 weeks. The type of healing and problems in the small follow up group mirrors that of what is experienced in our larger full scale trials [7-9]. The use of nurses can dramatically help lower costs to help scale up large circumcision programs. In some hospitals in Southern Africa medical technicians are taught to complete small medical procedures including wound dressing and suturing. The design of the Unicirc prevents damage to the penis by protecting the glans. In short, the device is as close to ‘foolproof’ as it can possibly be. It should be possible to extend its use to competent medical technicians as well nurses and midwives [10].
Conclusion
The Unicirc circumcision device can be used by nurses after rapid training on models and in vivo so that they can perform independent circumcisions within days while recognizing possible complications and pitfalls and the contraindications to sterilization. The clinical and cosmetic results appear to be the same as when circumcisions have been performed by medical personnel. This is a step enabling cheaper and more extensive provision of elective circumcision to help control the spread of HIV when used in conjunction with other known preventive methods eg condoms. Medical technicians who are already performing minor surgical procedures should be able to be taught the safe use of this method.
Acknowledgement
We would like to thank Mr. Bradley Paulse for statistical advice.
Declaration
The authors report no conflicting interests.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not- for- profit sectors but the Unicircs and training was provided by Simunye Health Care, Sea Point, Cape Town, South Africa.
Data Utilisation
The data were collected in compliance with the South African ratification of the Nagoya Protocol.
References
- Williams BG, Lloyd -Smith JO, Gouws E, et al. The potential impact of male circumcision on HIV in sub-Saharan Africa. PLoS Med 3 (2006): e262.
- Bongaarts J, Reining P, Way P, et al. The relationship between male circumcision and HIV infection in African populations. AIDS 3 (1989): 373-377.
- Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlledintervention trial of male circumcision for the reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med 2 (2005): e298.
- Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomized controlled trial. Lancet 369 (2007): 643-656.
- Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in Rikai, Uganda: a randomized trial. Lancet 369 (2007): 657-666.
- Morris BJ, Wamai RG. Biological basis for the protective effect conferred by male circumcision against HIV infection. International Journal of STD & AIDS 23 (2012): 153-159.
- Millard PS, Wilson HR, Godlstuck ND, et al. Rapid, minimally invasive adult voluntary male circumcision: a randomized trial of Unicirc, a novel disposable device. S Afr Med J 104 (2014): 52-57.
- Millard PS, Goldstuck ND. No needle, single-visit adultmale circumcision with Unicirc: a muli-centre field trial. PLoS ONE 10 (3): e0121686.
- Millard PS, Goldstuck ND. Minimally invasive, sutureless, adolescent male circumcision with topical anesthetic: a field trial of Unicirc, a single-use surgical instrument. Transl Androl Urol 9 (2020): 516-522.
- Davis SM, Baker H, Gross JM, et al. The role of nurses and midwives in expanding and sustaining voluntary male medical circumcision services for HIV prevention: A systematic and policy review. J of Assoc of Nurses in AIDS care 32 (2021): 3-28.
- Morris BJ, Klausner JD. In developed countries male circumcision prevalence is inversely related to HIV prevalence. Israel Journal of Health Policy Research 4 (2015): 40.
- Goldstuck ND, The role of adult male circumcision in HIV? AIDS – does the technique make a difference? Androl Gyneco: Curr Res 2 (2014): 3.




 Impact Factor: * 5.3
Impact Factor: * 5.3 Acceptance Rate: 75.63%
Acceptance Rate: 75.63%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 