Effects of Ketamine, S-Ketamine and MK 801 on Integrin Beta-3-mediated Cell Migration in Pancreatic Carcinoma
Manuela Malsy1*, Veronika Hofer1, Stephan Schmidbauer1, Bernhard Graf1 and Anika Bundscherer1
1Department of Anesthesiology, University Medical Center Regensburg, Germany
*Corresponding Author: Manuela Malsy, Department of Anesthesiology, University Medical Center Regensburg, Franz Josef Strauss Allee 11, 93053 Regensburg, Germany.
Received: 06 December 2022; Accepted: 15 December 2022; Published: 22 December 2022
Article Information
Citation: Manuela Malsy, Veronika Hofer, Stephan Schmidbauer, Bernhard Graf and Anika Bundscherer. Effects of Ketamine, S-Ketamine and MK 801 on Integrin Beta-3-mediated Cell Migration in Pancreatic Carcinoma. Journal of Cancer Science and Clinical Therapeutics 6 (2022): 446-451.
View / Download Pdf Share at FacebookAbstract
Introduction: Pancreatic ductal adenocarcinoma is one of the most aggressive malignancies in humans. The main reason for its unfavourable prognosis is the combination of rapid tumour growth, early-onset metastasis and currently still inadequate diagnostic and therapeutic options. Thus, only very few patients are eligible for radical resection of the primary tumour as the only curative treatment option available so far. In the perioperative period, tumour progression and metastasis are facilitated by the activation of key signalling pathways and the altered regulation of transcription factors. Various tumour entities have shown increased expression of the integrin-3 receptor subunit, which correlates with more rapid tumour progression and metastasis through advanced migration, invasion and proliferation. The influence of perioperative medication and postoperative pain management remains unclear. To investigate the effects of ketamine, s-ketamine and MK 801 on integrin beta-3-mediated cell migration in pancreatic cancer cells in vitro.
Methods: The effects of ketamine, s-ketamine and MK 801 on integrin beta-3 expression were investigated with immunoblot. Cell migratory potentials were analysed using a Cell Migration Assay Kit with a Boyden chamber, in which cells migrate through a semipermeable membrane under different stimuli.
Results: Stimulation with ketamine and MK 801 significantly promoted migration in pancreatic cancer cells, increasing the expression of integrin beta-3.
Conclusion: Novel therapeutic approaches target the effective modulation of specific signalling and transcription pathways. The prerequisite for such ‘target therapies‘ is comprehensive knowledge about the respective carcinogenesis. Further studies are required to identify the
Keywords
<p>Integrin Beta-3; Ketamine; Migration; MK 801; Pancreatic Cancer; S-Ketamine</p>
Article Details
List of Abbreviations:
DPBS- Dulbecco's Phosphate-Buffered Saline; GC-Box- Regulatory Element Rich in Guanine and Cytosine; ITGB3- Integrine Beta-3; MK 801- Dizocilpine; NFATc2- Nuclear Factors of Activated T-cells; NMDA-Receptor- N-methyl-D-aspartate-Receptor; PCP- Phencyclidine; Sp1- Specificity Protein 1; TBS-Buffer- Tris-buffered Saline-Buffer
1. Introduction
Pancreatic ductal adenocarcinoma is one of the most aggressive types of malignant tumours in humans. With increasing incidence rates in western industrialised countries and a 5-year survival rate of less than 10% after diagnosis [1], pancreatic carcinoma is the fourth most common tumour-related cause of death in Germany and other western countries [2]. Although some progress in the molecular and biological understanding of pancreatic carcinoma has been made in recent years [3], patients’ survival rates have not significantly improved. Long-term survival is still almost impossible [4]. The main reason for the unfavourable prognosis of pancreatic carcinoma is the combination of rapid tumour growth, early-onset metastasis and currently still inadequate diagnostic and therapeutic options [5]. Thus, only very few patients are eligible for radical resection of the primary tumour as the only curative treatment option available so far [6]. Recent studies have shown that the perioperative period is a particularly vulnerable phase, in which tumour progression and metastasis are facilitated by the constitutive activation of key signalling pathways and the altered regulation of transcription factors [7]. Various tumour entities have shown increased expression of the integrin-3 receptor subunit on tumour cells and vascular endothelial cells [8], which correlates with more rapid tumour progression and metastasis through increased migration, invasion and proliferation [9]. The extent of the influence of medication administered in the perioperative setting or as postoperative pain therapy remains unclear. Aim of this study is to investigate the effects of ketamine, s-ketamine and MK 801 on integrin beta-3-mediated migration of pancreatic cancer cells in vitro.
2. Material and Methods
2.1 Cell Lines
The human pancreatic cancer cell lines PaTu 8988t and PANC-1 were obtained from Professor Ellenrieder (Philipps University of Marburg, Germany). PaTu 8988t and PANC-1 cells were maintained in Dulbecco's modified Eagle’s medium (Sigma-Aldrich) supplemented with 10% foetal calf serum (Sigma-Aldrich) and 5% Myco Zap (Lonza Verviers SPRL). Cells were cultured in humidified CO2 atmosphere (5%) at 37°C and maintained in monolayer culture. Experiments were done with cells at ~70-80% confluence.
2.2 Reagents
Commercially available ketamine, s-ketamine and MK 801 were purchased from Sigma-Aldrich. Final concentrations were obtained by diluting drugs in standard growth media. All solutions were prepared freshly prior to use.
2.3 Cell Lysate
Cells were washed twice with cold DPBS and re-suspended in RIPAE buffer (5 mL Triton X100, 190 mg EDTA, 0.5 g SDS, 2.5 g deoxycholic acid, 500 mL DPBS, proteinase inhibitors) for 15 min and centrifuged at 13.000 rpm for 30 min. Supernatants were transferred to new cups and incubated on ice.
2.4 Subcellular Fractionation and Immunoblotting
Cells were washed twice with cold DPBS and collected through centrifugation at 4000 rpm at 4°C for 10 min. Lysates were then re-suspended in RIPAE buffer (5 mL Triton X100, 190 mg EDTA, 0.5 g SDS, 2.5 g deoxycholic acid, 500 mL DPBS, proteinase inhibitors) for 15 min and centrifuged at 13.000 rpm for 30 min. Supernatants were transferred to new cups and incubated on ice. For Western blotting, 30 µg protein extracts were analysed with SDS-PAGE and blotted onto nitrocellulose. Upon protein extraction and gel transfer, membranes were washed in TBS washing buffer and incubated with peroxidase-conjugated secondary antibodies. Immunoreactive proteins were visualised by means of an enhanced chemi-luminescence detection system (Western Blotting Detection Reagent, GE Healthcare). For immunoblotting, membranes were probed with antibodies against integrin beta-3 (cell signalling) and ß-actin (Sigma-Aldrich).
2.5 Cell Migration Assay
Cell migratory potentials were evaluated using a Cell Migration Assay Kit (abcam). The test includes a Boyden chamber, in which the cells migrate through a semipermeable membrane under different stimuli. In brief, cells were treated with 0 µM, 10 µM, 100 µM or 1000 µM ketamine, with 0 µM, 10 µM, 100 µM or 1000 µM s-ketamine or with 0 µM, 10 µM, 100 µM or 1000 µM MK 801 in a serum-free medium for 2 h. Afterwards, 200.000 cells of the human pancreatic cancer cell lines PaTu 8988t or PANC-1 were placed into the upper Boyden chamber, and a stimulant was pitted into the lower chamber. The chambers were incubated at 37°C for 24 h. The migrating cells passed through the semipermeable membrane and migrated into the bottom chamber or adhered to the bottom of the upper chamber. After dismantling, cell migration was directly analysed by means of reading fluorescence (Ex/Em = 530/590 nm) in a plate reader. All tests were done with three wells per treatment group and performed as two independent experiments.
2.6 Statistical Analysis
Data are presented as mean ± SD. The non-parametric Mann Whitney U-test was used for statistical evaluation of the data. P-values of <0.05 were considered significant. IBM SPSS Statistics (Vs. 26; IBM New York, US) and Excel Vs. 2019 (Microsoft, Redmond, USA) packages were employed for statistical analysis.
3. Results
3.1 Endogenous Proof of Integrin Beta-3 Expression in the Pancreatic Cancer Cell Lines PaTu 8988t and PANC-1 after Stimulation with Ketamine, S-Ketamine and MK 801
The first aim was to obtain evidence for the expression of integrin beta-3 in pancreatic cancer cells (Figure 1). Expression of integrin beta-3 was very weak in the pancreatic cancer cell line PaTu 8988t but much stronger in PANC-1 (Column 1). Stimulation with 100 µM ketamine, 100 µM s-ketamine or 100 µM MK 801 increased expression of integrin beta-3 in both pancreatic cancer cell lines compared to unstimulated control (Column 1). The endogenous expression of ß-actin serving as loading control can be seen in the lower blot (Column 2).
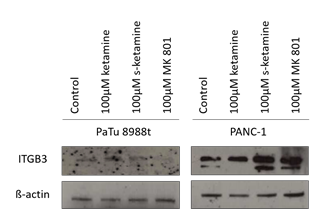
Figure 1: Immunoblotting and proof of the endogenic expression of integrin beta-3 in the pancreatic cancer cell line PaTu 8988t und PANC-1 after stimulation with 100 µM ketamine, 100 µM s-ketamine or 100 µM MK 801.
3.2 Analysis of Migration in Pancreatic Cancer Cells
A Cell Migration Assay Kit was used to determine whether stimulation with ketamine, s?ketamine or MK 801 induced cell migration. The test includes a Boyden chamber, in which cells migrate through a semipermeable membrane under different stimuli. For this purpose, the pancreatic cancer cell lines PaTu 8988t and PANC-1 were treated with 0 µM, 10 µM, 100 µM or 1000 µM ketamine, with 0 µM, 10 µM, 100 µM or 1000 µM s-ketamine or with 0 µM, 10 µM, 100 µM or 1000 µM MK 801 in a serum-free medium for 2 h. After 24 h incubation, cell migration was directly analysed by means of reading fluorescence in a plate reader. The pancreatic cancer cell lines PaTu 8988t (a) and PANC-1 (b) showed increased cell migration after stimulation with 100 µM and 1000 µM MK 801 compared to untreated control; the cell line PANC-1 also showed an additive increase in cell migration after stimulation with 10 µM MK 801 (Figure 2). In the cell line PaTu 8988t, stimulation with 10 µM and 100 µM ketamine also led to a statistically significant increase in cell migration (Figure 2a). In the pancreatic cancer cell line PANC-1, stimulation with 1000 µM ketamine significantly inhibited cell migration (Figure 2b).
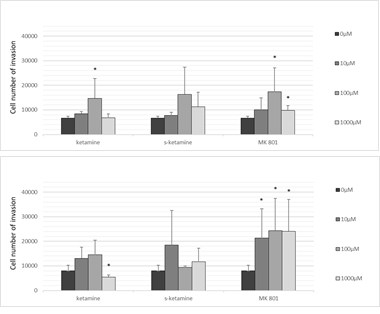
Figure 2 (a,b): The effects of ketamine, s-ketamine and MK 801 on cell migration in the pancreatic cell lines PaTu 8988t (a) and PANC-1 (b) in vitro. Cell migration was quantified by means of a Boyden chamber, in which cells migrate through a semipermeable membrane under different stimuli. (*) indicates statistical significance at p <0.05 compared to untreated control.
4. Discussion
In carcinogenesis, the metastasis of tumour cells represents the endpoint of a multi-step process [10]. Metastases develop when cancer cells detach from the primary tumour, migrate with blood or lymph and relocate and multiply in other tissues. Molecular biological analyses have shown loss or inactivation of cell-cell or cell-matrix adhesion molecules [11]. Integrins bind to various proteins of the extracellular matrix and mediate bidirectional signal transduction. Integrins are transmembrane heterodimeric glycoproteins, which consist of 18 different alpha subunits and 8 different beta subunits, forming a total of 24 integrins [12]. Integrins typically occur on the surface of cell membranes only for a limited period of time [13]. The presence or absence of integrins has a huge influence on the capacity of malignant tumours to invade and destroy local tissue, thus also on the metastasis of tumour cells [14]. A key factor in the carcinogenesis of pancreatic carcinoma is the family of NFAT (nuclear factor of activated T-cells) transcription factors [15]. Preliminary work has shown that NFATc2 interacts with other transcriptional partners, such as the oncogenic protein Sp1 in pancreatic cancer, and that carcinogenic effects are caused by the interaction of NFATc2 and Sp1 [16]. The application of ketamine or s-ketamine seems to inhibit this activation cascade [17]. As N?methyl-D-aspartate (NMDA) receptor antagonists, ketamine, s-ketamine and MK 801 bind at the phencyclidine binding site inside the NMDA channel, thereby inhibiting the action of NMDA agonists [18]. Several recent studies have shown that functional NMDA receptors are expressed in tumours [19], inhibiting intracellular calcium concentration and inactivating calcium-dependent cytosolic guanyl cyclase [20]. Thus, NMDA receptors play a critical role in tumour development, tumour growth and metastasis [21]. As a first messenger, calcium plays a central role in tumour cell progression by regulating various signalling cascades [22]. Calcium influx into the cytosol results in the calcium-dependent activation of second messengers, thereby activating proteins of various other groups including transcription factors; in turn, this activation influences further tumour cell behaviour [23]. The NFAT-dependent regulation of integrins was already described by Jauliac and colleagues in 2002 [24]. A more recent preliminary expression profile analysis carried out by our group showed the NFATc2- and Sp1-dependent regulation of integrin beta-3 in pancreatic cancer cells. Here, Sp1 acts as a transcriptional repressor of NFATc2 at the respective GC box of the promoter [25]. The present study shows that integrin beta-3 is expressed in the pancreatic cancer cell lines PaTu 8988t und PANC-1. Stimulation of the tumour cells with ketamine, s-ketamine or MK 801 increases the expression of integrin beta-3. Stimulation with ketamine and s-ketamine decreases the expression of NFAT transcription factors in the nucleus and increases the expression of these transcription factors in the cytoplasm. Thus, the application of ketamine and s-ketamine places NFATc2 in an inactive, dormant state [17]. Stimulation of pancreatic cancer cells with ketamine, s-ketamine or MK 801 significantly increases cell migration. Furthermore, our group has already shown that ketamine and s-ketamine inhibit both cell proliferation and apoptosis in pancreatic cancer cells [26]. Therefore, the following molecular biological mechanism may be conceivable (Figure 3): As NMDA receptor antagonists, ketamine, s-ketamine and MK 801 bind at the phencyclidine binding site inside the NMDA channel, thereby inhibiting the action of NMDA agonists. This inhibition decreases the intracellular calcium concentration, which, in turn, inactivates various signalling cascades, such as the calcium-calcineurin-NFAT pathway. As a result, NFATc2 remains in an inactive, dormant state in the cytoplasm and undergoes reduced dephosphorylation and nuclear displacement by calcineurin [27]. In the cell nucleus itself, control of the promoter is complex. Many proteins are involved, which act as transcription factors or co-factors, or both, and form the ‘transcription machinery’ together with the transcription factors NFATc2 and Sp1. Here, Sp1 acts as a transcriptional repressor of NFATc2 at the respective GC box of the promoter. Finally, the interaction of various and partly still unknown proteins increases the expression of integrin beta-3, which also increases cell migration.
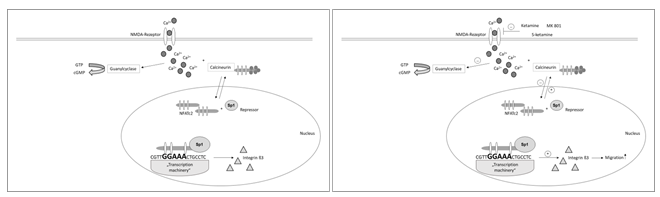
Figure 3 (a + b): Potential molecular biological mechanism of the effect of ketamine, s?ketamine and MK 801 on integrin beta-3-mediated migration in pancreatic carcinoma.
5. Conclusions
Pancreatic ductal adenocarcinoma is one of the most aggressive malignant tumours in humans. Its oncogenic potential is primarily characterised by extremely rapid tumour growth and early-onset metastasis [28]. Novel therapeutic approaches target the effective modulation of specific signalling and transcription pathways [29]. The integrin inhibitor cilengitide (Merck), a cyclic pentapeptide, was also developed for this purpose. Cilengitide is considered a highly potent inhibitor of tumour-induced angiogenesis because it inhibits interaction with the extracellular matrix by binding to integrin αvβ3 and/or αvβ5 [30]. In a clinical study (Phase I/II) investigating recurrent and metastasised squamous cell carcinoma of the head and neck, cilengitide was tested in combination with cisplatin, 5-fluorouracil and cetuximab, but the additional administration of cilengitide did not yield any therapeutic advantage [31]. The basis and prerequisite for new therapeutic approaches in the context of a ’target therapy’ is comprehensive knowledge about the carcinogenesis of the respective tumour entity. Therefore, further studies are required to identify the underlying disease mechanisms of pancreatic carcinoma. The identification and characterisation of cellular receptors as well as their extracellular activators will eventually help to establish new therapeutic options for the treatment of aggressive pancreatic cancer.
Acknowledgements
We thank Sigrid Bamberger, Regina Lindner, Gabriele Bollwein, Marion Schindler, and Ruth Spaeth for technical assistance. We thank Monika Schoell for linguistic support.
Conflicts of Interest
The authors declare that they have no conflicts interests.
References
- Mizrahi JD, Surana R, Valle JW, et al. Pancreatic cancer. Lancet 395 (2020): 2008-2020.
- Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol 22 (2016): 9694-9705.
- Lai HC, Kuo YW, Huang YH, et al. Pancreatic Cancer and Microenvironments: Implications of Anesthesia. Cancers (Basel) 14 (2022): 2684.
- Kleeff J, Korc M, Apte M, et al. Pancreatic cancer. Nat Rev Dis Prime 2 (2016): 16022.
- Schneider G, Siveke JT, Eckel F, et al. Pancreatic cancer: basic and clinical aspects. Gastroenterology 128 (2005): 1606-1625.
- Deplanque G, Demartines N. Pancreatic cancer: Are more chemotherapy and surgery needed? Lancet 389 (2017): 985-986.
- Gottschalk A, Sharma S, Ford J, et al. Review article: the role of the perioperative period in recurrence after cancer surgery. Anesth Analg 110 (2010): 1636-1643.
- Switala-Jelen K, Dabrowska K, Opolski A, et al. The biological functions of beta3 integrins. Folia Biol 50 (2004): 143-152.
- Desgrosellier J, Cheresh D. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer 10 (2010): 9-22.
- Chiang A, Massague J. Molecular basis of metastasis. N Engl J Med 359 (2008): 2814-2823.
- Talmadge J, Fidler I. AACR centennial series: the biology of cancer metastasis: historical perspective. Cancer Res 70 (2010): 5649-5669.
- De Franceschi N, Hamidi H, Alanko J, et al. Integrin traffic - the update. J Cell Sci 128 (2015): 839-852.
- Arcangeli A, Crociani O, Bencini L. Interaction of tumour cells with their microenvironment: ion channels and cell adhesion molecules. A focus on pancreatic cancer. Philos Trans R Soc Lond B Biol Sci 369 (2014): 20130101.
- Li J, Peng L, Chen Q, et al. Integrin β1 in Pancreatic Cancer: Expressions, Functions, and Clinical Implications. Cancers (Basel) 14 (2022): 3377.
- König A, Fernandez-Zapico ME, Ellenrieder V. Primers on molecular pathways--the NFAT transcription pathway in pancreatic cancer. Pancreatology 10 (2010): 416-422.
- Malsy M, Graf B, Almstedt K. Interaction between NFATc2 and the transcription factor Sp1 in pancreatic carcinoma cells PaTu8988t. BMC Mol Biol 18 (2017): 20.
- Malsy M, Graf B, Bundscherer A. The effects of analgesics and local anesthetics on gene transcription mediated by NFATc2 and Sp1 in pancreatic carcinoma. Anticancer Res 39 (2019): 4721-4728.
- Stepulak A, Sifringer M, Rzeski W, et al. NMDA antagonist inhibits the extracellular signal-regulated kinase pathway and supresses cancer growth. Proc Natl Acad Sci U S A 102 (2005): 15605-15610.
- Luksch H, Uckermann O, Stepulak A, et al. Silencing of selected glutamate receptor subunits modulates cancer growth. Anticancer Res 10 (2011): 3181-3192.
- Hirota K, Lambert DG. Ketamine; history and role in anesthetic pharmacology. Neuropharmacology 216 (2022): 109171.
- Kalariti N, Pissimissis N, Koutsilieris M. The glutamatergic system outside the CNS and in cancer biology. Expert Opin Investig Drugs 12 (2005): 1487-1496.
- Monteith G, Davis F, Roberts-Thomson. Calcium channels and pumps in cancer: changes and consequences. Journal Biol Chem 287 (2012): 31666-31673.
- Bengtson C, Bading H. Nuclear calcium signaling. Adv Exp Med Biol 970 (2012): 377-405.
- Jauliac S, Lopez-Rodriguez C, Shaw LM, et al. The role of NFAT transcription factors in integrin-mediated carcinoma invasion. Nat Cell Bio 4 (2012): 540-544.
- Malsy M, Graf B, Almstedt K. The active role of the transcription factor Sp1 in NFATc2-mediated gene regulation in pancreatic cancer. BMC Biochem 20 (2019): 2.
- Malsy M, Bundscherer A, Gebhardt K, et al. Effects of ketamine, s-ketamine and MK 801 on proliferation, apoptosis and necrosis in pancreatic cancer cells. BMC Anesthesiol 15 (2015): 111.
- Buchholz M, Schatz A, Wagner M, et al. Overexpression of c-mycin pancreatic cancer caused by ectopic activation of NFATc1 and the Ca2+/calcineurin signaling pathway. EMBO J 25 (2006): 3714-3724.
- Zuzcák M, Trnka J. Cellular metabolism in pancreatic cancer as a tool for prognosis and treatment (Review). Int J Oncol 61 (2022): 93.
- Lo W, Zureikat A. Neoadjuvant therapy in pancreatic cancer: a review and update on recent trials. Curr Opin Gastroenterol 38 (2022): 521-531.
- Mas-Moruno C, Rechenmacher F, Kessler H. Cilengitide: the first anti-angiogenic small molecule drug candidate design, synthesis and clinical evaluation. Anticancer Agents Med Chem 10 (2010): 753-68.
- Vermorken J, Peyrade F, Krauss J, et al. Cilengitide with cetuximab, cisplatin, and 5-FU in recurrent and/or metastatic squamous cell cancer of the head and neck: The ADVANTAGE phase II trial. J Clin Oncol 30 (2010).


 Impact Factor: * 4.1
Impact Factor: * 4.1 Acceptance Rate: 74.74%
Acceptance Rate: 74.74%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 