Fever of Unknown Origin in Adult Caused by Hemophagocytic Lymphohistiocytosis: A case Report and Review of the Literature
Mendez GD1, Vivas M2, Rodriguez-Pascual J3*
1Hematology Department, Hospital Universitario HM Puerta del Sur. Avenida Carlos V - Móstoles, 28938 Madrid. Spain
2Internal Medicine Department, Hospital Universitario HM Puerta del Sur. Avenida Carlos V - Móstoles, 28938 Madrid. Spain
3Oncology Department, Hospital Universitario HM Puerta del Sur. Avenida Carlos V - Móstoles, 28938 Madrid. Spain
*Corresponding Author: Dr. Jesus Rodriguez-Pascual, Oncology Department, Hospital Universitario HM Puerta del Sur. Avenida Carlos V - Móstoles, 28938 Madrid. Spain
Received: 11 July 2019; Accepted: 02 August 2019; Published: 12 August 2019
Article Information
Citation: Mendez GD, Vivas M, Rodriguez-Pascual J. Fever of Unknown Origin in Adult Caused by Hemophagocytic Lymphohistiocytosis: A case Report and Review of the Literature. Journal of Cancer Science and Clinical Therapeutics: 3 (2019): 098-101.
View / Download Pdf Share at FacebookAbstract
Hemophagocytic lymphohistiocytosis (HLH), also known as hemophagocytic syndrome, is a very uncommon and life-threatening hematologic disorder that occurs as a primary or acquired disease. Secondary HLH usually appears in the setting of infections, underlying rheumatologic disorders or lymphoid malignancies. Clinically the syndrome is characterized by fever, multiple cytopenias, hepatosplenomegaly and activated macrophages in hematopoietic organs. We describe a rare case of HLH in the context of abdominal pain and fever of unknown origin, dramatic worsening and, finally, successful evolution with immunosuppressive therapy. In addition, we review the available literature on this topic.
Keywords
<p>Hemophagocytic; Lymphohistiocytosis; Fever</p>
Article Details
1. Case Report
A 70 year- old man was admitted to our hospital with cough, fever, abdominal pain with no alteration of the gastrointestinal transit and progressive poor performance status, presenting for two weeks. He was previously treated with amoxicillin and then levofloxacin with a poor clinical response. Examination revealed a fever of 38º and confused state. Blood tests showed minor thrombocytopenia (87,000 platelets/mL), elevated transaminases (GGT 293 U/L, GOT 65 U/L, GPT 41 U/L) with normal bilirubin, LDH 1665 U/L, ferritin 858 ng/mL, VSG 120 mm/h, PCR 211 mg/L, b2microglobulin 11.58 ug/mL, serum soluble IL-2 receptor level > 7500 U/mL and coagulopathy. Peripheral blood smear showed no evidence of schistocytes or parasites. The lumbar puncture was negative. A CT scan revealed homogeneous splenomegaly and a thoracic breast nodule; this lesion was biopsied and a breast ductal carcinoma was confirmed. We started empirical antibiotic coverage with broad spectrum antibiotics (piperacillin-tazobactam, linezolid and doxycycline). All microbiological cultures were negative. The patient maintained a persistent fever during hospital admission, presenting a dramatic worsening with hypovolemic shock, anuria and acute renal failure, requiring immediate transfer to our intensive care unit. Once stabilized hemodynamically, a bone marrow biopsy revealed hemophagocytic cells (CD8+ macrophages) and erythroid hyperplasia with hemophagocytic phenomena [see Figure 1], and she was diagnosed with HLH. The patient started treatment with dexamethasone, etoposide and immunoglobulins, presenting progressive clinical improvement. Oncological surgery of the patient was performed, consisting of radical mastectomy and axillary lymphadenectomy. Finally, the patient was discharged after 60 days on a descending regimen of oral corticosteroids.
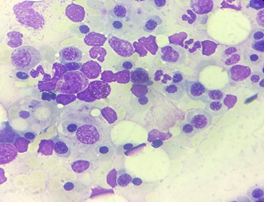
Figure 1: Marrow aspirate.
However, in a control PET carried out more than a month after hospital discharge, multiple adenopathies were observed and biopsy confirmed a large-B-cell lymphoma. The patient started treatment with CHOP and appears to be responding well.
2. Discussion
Hemophagocytic lymphohistiocytosis (HLH) is a syndrome of excessive immune activation in which lymphocytes and macrophages produce high levels of cytokines, and that is thought to be a primary mediator of tissue damage. HLH is a febrile illness associated with multiple organ involvement, lymphadenopathy and neurological signs. The most common laboratory findings are: cytopenias, especially anemia and thrombocytopenia, elevated ferritin, increased triglycerides and abnormal coagulation and liver function test abnormalities with elevation of liver enzymes, LDH and bilirubin. Hemophagocytosis is not pathognomonic, is not required for diagnosis and may be absent initially [1].
Many patients have a genetic predisposing factor and others have an immunologic trigger. They are divided into primary hemophagocytic lymphohistiocytosis (HLH) and secondary hemophagocytic syndromes [2]. Primary HLH is caused by genetic mutations that impair the cytotoxic function of the natural killer cells (NK) and the cytotoxic T cells and usually happens in childhood. Secondary or acquired hemophagocytic syndromes generally affect adolescents and adults and are not associated with known genetic defects. Acquired HLH is associated with a variety of underlying conditions, including infection (the most common form), malignancy, rheumatological disorders and immune dysregulation.
Macrophage activation syndrome (MAS) is a variant of HLH that occurs in patients with auto-inflammatory or autoimmune diseases. Most MAS cases have been described in systemic juvenile idiopathic arthritis (sJIA) and its adult-onset form, but also in systemic lupus erythematosus or other rheumatic diseases. Malignant lymphomas associated with HLH are more frequent in adults than in children and often have a T cell origin. There is increased awareness that patients with acquired immunodeficiencies such as AIDS, either drug-induced or after organ and hematopoietic stem cell transplants (HSCT), are at risk of developing HLH. Rare causes of HLH are metabolic diseases [1]. The diagnosis of HLH requires that either conditions 1 or 2 below (see Table 1) are fulfilled.
|
Molecular diagnosis |
|
|
· Pathological mutations of PRF1, UNC13D, STXBP1, RAB27A, STX11, SH2D1A, or XIAP |
|
|
OR |
|
|
Clinical criteria |
Five of the following |
|
• Fever of 38.5ºC or more |
|
|
• Splenomegaly |
|
|
• Peripheral blood cytopenia with at least two of these: hemoglobin <9 g/L, platelets < 100000/microL, absolute neutrophil count <1000/microL. |
|
|
• Hypertriglyceridemia (fasting triglycerides >3 mmol/L and/or hypofibrinogenemia < 150 mg/dL) |
|
|
• Hemophagocytosis in bone marrow or spleen, lymph nodes or liver. |
|
|
• Low or absent NK-cell activity |
|
|
• Ferritin ≥500 ng/mL |
|
|
• Elevated soluble CD 25 (i.e., soluble IL-2 receptor alpha) ≥2 standard deviations above age-adjusted lab forms. |
|
Table 1: HLH criteria.
Patients should be referred to a hematology or oncology specialist. They can be treated for a trigger condition if stable but can rarely avoid cytotoxic therapy. Treatment regimens include etoposide and steroids. HPS associated with lymphomas are given CHOP (Cyclophosphamide Doxorubicin) [3]. Initial treatment usually includes steroids in most cases. Other regimens include etoposide for secondary HLH and in some cases therapy with hematopoietic cells has been used. Other treatment regimens include plasma exchange, splenectomy, and recombinant human thrombopoeitin (rhTPO) [4, 5]. Intrathecal methotrexate and hydrocortisone are used in case of neurological involvement. Allogeneic hematopoietic stem cell transplant is used when sustained remission cannot be achieved by immunosuppressive drugs.
Our patient was initially treated with steroids and etoposide and, after the diagnosis of lymphoma, with CHOP regimen. In summary, HLH is a very infrequent and life-threatening syndrome that requires the cooperation of multiple specialists for a correct diagnosis and early treatment. This Case Report shows an example of multidisciplinary management (Internal Medicine, Hematology, Pathological Anatomy but also Medical and Surgical Oncology, Intensive Care Unit etc), that is essential for a successful clinical management.
References
- Janka GE, Lehmberg K. Hemophagocytic lymphohistiocytosis: pathogenesis and treatment. Hematology Am Soc Hematol Educ Program (2013): 605-611.
- Jaffe R. The histiocytoses.Clin Lab Med 19 (1999): 135-155.
- Kleynberg RL, Schiller GJ. Secondary hemophagocytic lymphohistiocytosis in adults: an update on diagnosis and therapy. Clin Adv Hematol Oncol 10 (2012): 726-732.
- Hayden A, Park S, Giustini D, et al. Hemophagocytic syndromes (HPSs) including hemophagocytic lymphohistiocytosis (HLH) in adults: A systematic scoping review. Blood Rev 30 (2016): 411-420.
- Hayden A, Park S, Giustini D, et al. Hemophagocytic syndromes (HPSs) including hemophagocytic lymphohistiocytosis (HLH) in adults: A systematic scoping review. Blood Rev 30 (2016): 411-420.


 Impact Factor: * 4.1
Impact Factor: * 4.1 Acceptance Rate: 74.74%
Acceptance Rate: 74.74%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 