A Case of Early Recurrent Gallstone Ileus. What to do about the Residual Gallbladder Stone?
Henry Liao*1, Henry Richard Edward Drysdale1, Pia Bernardi2, Sonal Nagra2, David A Watters2
1Department of Surgery, Barwon Health, Geelong, Victoria, Australia
2Department of Surgery, Epworth Geelong Hospital and Deakin University, Geelong, Victoria, Australia
*Corresponding Author: Henry Liao, Department of Surgery, Barwon Health, Geelong, Victoria, Australia
Received: 10 March 2023; Accepted: 17 March 2023; Published: 20 April 2023
Article Information
Citation: Henry Liao, Henry Richard Edward Drysdale, Pia Bernardi, Sonal Nagra, David A Watters. A Case of Early Recurrent Gallstone Ileus. What to do about the Residual Gallbladder Stone?. Journal of Surgery and Research. 6 (2023): 150-152.
View / Download Pdf Share at FacebookKeywords
<p>Gallstone ileus, Recurrence, Enterolithotomy, Emergency surgery</p>
Article Details
Case Presentation
An 87-year-old lady presented to the emergency department with abdominal pain and vomiting. She had a past history of atrial fibrillation, cerebrovascular accident and type two diabetes mellitus. She had a virgin abdomen. Her medications included apixaban. A CT scan of the abdomen and pelvis was consistent with a gallstone ileus. The small bowel was grossly distended secondary to a 38mm gallstone in the distal jejunum. The gallbladder contained a second 36mm gallstone and gas locules consistent with a cholecystoduodenal fistula.
The patient proceeded promptly to theatre for a laparotomy. A longitudinal enterotomy was performed immediately proximal to the gallstone, the gallstone extracted and the enterotomy closed transversely with interrupted 3.0PDS sutures. Omentum was densely adhered to the gallbladder. The decision was made not to proceed with any hepatobiliary intervention. This included not attempting to milk the stone from within the gallbladder into the duodenum.
The patient initially recovered without issue. Bowel function returned on post-operative day (POD) three and patient was discharged for rehabilitation on day four. Unfortunately, on POD eight, the patient developed abdominal pain, distension and vomiting. A repeat CT scan revealed that the second 36mm gallstone had migrated from the gallbladder into the mid jejunum and had caused a recurrent small bowel obstruction.
The patient underwent a relook laparotomy, confirming a recurrent gallstone ileus in the mid jejunum, proximal to the site of previous obstruction. The gall stone was managed operatively in a similar fashion and again no intervention was performed on the cholecystoduodenal fistula.
The patient recovered without issue from their second laparotomy. She was discharged on POD 13 to inpatient rehabilitation. She remained in rehabilitation for 28 days prior to returning home. At a subsequent outpatient clinic review, in the setting of her multiple comorbidities and no residual stones, a decision was made not repair her cholecystoduodenal fistula.
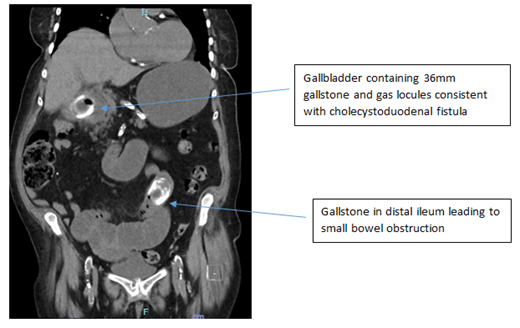
Figure 1: Coronal image of a CT abdomen/pelvis demonstrating a gallstone ileus with the gallbladder containing another gallstone and gas consistent with a cholecystoduodenal fistula
Discussion
Gallstone ileus (GSI) is an uncommon cause of mechanical obstruction of the gastrointestinal tract (GIT) resulting from an impacted gallstone. It is a rare complication of cholelithiasis (0.15% to 1.5%)1 and it accounts for 1-3% of all cases of mechanical GIT obstruction [1].
Once a gallstone is formed within the gallbladder, chronic inflammation or vascular insufficiency may lead to fistulation of the gallstone outside of the gallbladder. This process leads to the development of a cholecystoenteric fistula (CCEF) [2]. The majority of the CCEF (75-83%) are formed between the gallbladder and duodenum but it can be to the colon, stomach or other parts of small bowel [3]. When the stone is within the extra-biliary GIT it may become impacted and lead to mechanical obstruction. The larger the stone, the more likely it is to lead to obstruction. Stones >2.5cm are considered highly likely to become impacted [4,5]. A review of 1001 reported cases indicated the ileum as the most common site of impaction (50.0-60.5%), followed by jejunum (16.1-26.9%), duodenum (3.5-14.6%), and colon at 3-4.1% [4,5]. Impaction at the duodenal bulb causing gastric outlet obstruction, known as Bouveret syndrome, has also been reported [6].
Surgery is indicated to relieve acute mechanical obstruction from a GSI. Rates of non-operative resolution of a GSI are low [5]. This usually involves an enterotomy to remove the offending stone with subsequent closure, as was done in this case.
What to do about the CCEF at the time of the initial operation remains a controversial area of surgical management. Modern surgical teaching would advise against any acute surgical management of a cholecystoenteric fistula at the time of the initial operation. The combination of an acutely unwell patient, who are often elderly with medical co-morbidities, with a technically difficult operation can lead to an increased risk of adverse outcomes.
Single stage enterolithotomy with cholecystoenteric tract closure was shown to have higher mortality at 16.9% due to its invasiveness, longer hospital stays and higher post-operative complication rates compared to lower mortality rate of simple enterolithotomy at 11.7% [1,5].
The decision to not acutely intervene with the cholecystoenteric fistula can also lead to adverse outcomes, as was demonstrated in this case. An early recurrent GSI from the residual gallstone in the setting of a patent CCEF eventuated because no acute intervention was performed. A systematic review demonstrated that untreated CCEF with known cholelithiasis or undetected non-obstructive calculous in more proximal small bowel carries a 5-8% risk of recurrent GSI (RGSI) [5,7,8]. 85% of RGSI occurred within six months of the initial enterolithotomy, and 62.6% recurred within six weeks [3]. In 113 cases of RGSI, the average stone was 3.6cm in size, and the vast majority were faceted, increasing the likelihood of finding additional stones [7].
In order to decrease the risk of RGSI, whilst avoiding the increased risk of the acute surgical management of a CCEF, a thorough search of the entire GIT at the time of the initial operation has been advocated [3]. This usually involves intra-operative palpation of the GIT, aided by visual inspection. This includes both the gallbladder itself as well as the stomach, small bowel and colon. The utilizing of pre-operative CT imaging allows a targeted approach for this search [9].
In the setting of a known large stone within the gallbladder, consideration may be given to ‘milking’ of the stone from the gallbladder into the GIT. If easily done, this may allow subsequent removal and avoidance of an early post-operative recurrent obstruction. This intervention must of course be balanced against the risk of disrupting the cholecystoenteric fistula. With the benefit of retrospect, such an approach in this case may have prevented the complication of early RGSI.
Aside from recurrent obstruction, a persistent cholecystoduodenal fistula and cholecystocolonic fistula can result in recurrent cholangitis (11% and 60% risk respectively) [4,10]. There may also be an increased risk of gallbladder malignancy, up to a 15% risk in patients with a persistent fistula [11]. These risks of complications of the fistula track underlie the decision making when considering delayed surgical intervention for a CCEF. Whilst a spontaneous closure of the fistula is possible, it is unlikely to occur [10]. As with any surgical condition, the risks of an elective repair of a CCEF must be made in the context of the individual patient profile and surgeon experience.
Conclusion
This case demonstrates the risk of RGSI from a residual gallstone when managing a patient with a GSI. Whilst acute surgical management of a CCEF is associated with an increased risk of perioperative complications, consideration should be given for the interrogation of the remainder of the GIT for another stone. Identification of another stone, aided by pre-operative imaging, may allow for subsequent removal and prevention of a RGSI.
References
- Halabi WJ, Kang CY, Ketana N, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 259 (2014): 329-335.
- Rodriguez-Sanjuan JC, Casado F, Fernandez MJ, et al. Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. The British journal of surgery 84 (1997): 634-637.
- Mir SA, Hussain Z, Davey CA, et al. Management and outcome of recurrent gallstone ileus: A systematic review. World J Gastrointest Surg 7 (2015): 152-159.
- Clavien PA, Richon J, Burgan S, et al. Gallstone ileus. The British journal of surgery 77 (1990): 737-742.
- Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. The American surgeon 60 (1994): 441-446.
- Cappell MS, Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol 101 (2006): 2139-2146.
- Buetow GW, Glaubitz JP, Crampton RS. Recurrent Gallstone Ileus. Surgery 54 (1963): 716-724.
- Doogue MP, Choong CK, Frizelle FA. Recurrent gallstone ileus: underestimated. Aust N Z J Surg 68 (1998): 755-756.
- Yu CY, Lin CC, Shyu RY, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 11 (2005): 2142-2147.
- Inukai K. Gallstone ileus: a review. BMJ Open Gastroenterol 6 (2019): e000344.
- Bossart PA, Patterson AH, Zintel HA. Carcinoma of the gallbladder. A report of seventy-six cases. Am J Surg. 103 (1962): 366-369.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 