Total Knee Arthroplasty in Advanced Active Tuberculous Arthritis of the Knee
Jingsheng wang1*, Tingting Liu1, Apeng Zou2, Qingpeng Shi2, Baisui Zhou2
1Department of Orthopedics, Laizhou People,s Hospital, No.1718, Wuli Street, Laizhou, China, 261400
2Department of Orthopedics, Yantai Affiliated Hospital of Binzhou Medical University, No.717, Jinbu Street, Yantai, China, 264100
*Corresponding Author: Jingsheng Wang, Department of Orthopedics, Laizhou People’s Hospital, No.1718, Wuli Street, Laizhou, China, 261400
Received: 19 May 2022; Accepted: 25 May 2022; Published: 27 May 2022
Article Information
Citation: Jingsheng Wang, Tingting Liu, Apeng Zou, Qingpeng Shi, Baisui Zhou. Total Knee Arthroplasty in Advanced Active Tuberculous Arthritis of the Knee. Journal of Surgery and Research 5 (2022): 296-304
View / Download Pdf Share at FacebookAbstract
Purpose
The purpose of this study was to evaluate the safety of total knee arthroplasty (TKA) in the patients with advanced active tuberculous arthritis of the knee.
Methods
Eight patients with advanced active tuberculous arthritis of the knee were reviewed in this study. The diagnosis of each patient was confirmed by intraoperative histopathology of the biopsy specimen revealing granulomatous lesions with epithelioid histiocytes surrounded by lymphocytes. Cemented TKA with primary prosthesis was performed in all patients. Patients were given post-operative antitubercular medications for a total of twelve months. Local symptoms, erythrocyte sedimentation rate (ESR) values, and radiographs were used for detecting the recurrence of tuberculosis. The hospital for special surgery knee score (HSS) system was used to evaluate the function outcomes of the involved knees.
Results
Within an average follow-up period of 48.8 months, no recurrence of tuberculous infection was found in any of the patients. The ESR became normal (< 20 mm/h) within six months after TKA in all patients. At the most recent follow-up, the average HSS score improved from 32.4 ± 8.6(18-42) points preoperatively to 85.6 ± 9.7(68-94) points (p<0.001). All knees showed good integrity and no evidence of loosening of the prostheses was found. Bacteriological examination was positive for four patients.
Conclusions
TKA for advanced active tuberculosis of the knee is a safe procedure providing symptomatic relief and functional improvement. A long infection-free interval is not a prerequisite for TKA. Wide surgical debridement and adequate p
Keywords
<p>Infection, Tuberculosis, Total knee arthroplasty, Antitubercular therapy</p>
Article Details
1. Introduction
Tuberculosis (TB) is an ancient human disease caused by Mycobacterium tuberculosis and remains a major global health challenge with an estimated 10 million new TB cases worldwide in 2018 [1]. TB is a multi-systemic disease with a protean presentation although it mainly affects the lungs [2]. The rate of extra-pulmonary TB worldwide is about 20%–40%. Of cases with extra-pulmonary TB, 10%–25% have musculoskeletal involvement [3]. The most commonly affected site of musculoskeletal TB infection is the spine, followed by the hip, knee, and ankle/foot [4,5]. Due to its non-specific presentation TB of the knee is often reaches a very advanced state before a definite diagnosis is made, which then leads to a poor prognosis [6]. For the patients with end-stage joint destruction surgical intervention is frequently required to relieve pain and to restore mobility. Traditionally arthrodesis and total knee arthroplasty (TKA) are the main available options for orthopedic surgeons in the treatment of end-stage TB of the knee [7-13]. Arthrodesis may lead to decreased function in the affected limb and is associated with multiple complications such as nonunion and leg-length discrepancy although it can provide control of the infection and relief of pain [7,8]. In this realm, TKA can provide substantial benefits over arthrodesis, permitting the restoration of both function and mobility. By now there have been several reports on successful management of TB of the knee with TKA [9-14]. While TKA has clear benefits as a treatment modality, there is no consensus on the appropriate treatment regimens for the patients with tuberculosis of the knee [5]. For the timing of surgery, some authors suggested that TB should be inactive for several years prior to performing a TKA, while others proposed a much shorter interval [9,14,15]. To our knowledge, there are only a few articles on patients with active tuberculosis of the knee joint treated with TKA [12,13,16]. Additionally, when treating an active TB of the knee there is no consensus on whether to use a single- or two-stage TKA [5]. Therefore, the use of TKA for active tuberculous infection of the knee is still controversial and should be further investigated. Based on previous experience on active tuberculosis of hip treated with total hip arthroplasty [17] we performed TKA procedures for eight patients with active tuberculosis of the knee. The aim of the present study was to evaluate our encouraging experience and clinical outcomes of TKA in the patients with advanced active tuberculous arthritis of the knee.
2. Materials and Methods
This study was approved by the review board of our hospital and the informed consent was acquired from every patient. From January 2010 to December 2017, eight patients with advanced active tuberculous arthritis of the knee were admitted to our institution. There were three men and five women with the mean age of 57.6±6.8 years ranging from 47 to 67. The clinical data of the patients are shown in table 1. The preoperative diagnosis of TB of the knee joint was based on past history, clinical symptoms (unilateral excruciating knee pain, joint swelling, and disability) and imaging studies (the Phemister triad: juxta-articular osteoporosis, peripherally located osseous erosions, and gradual narrowing of the joint space) (Figure 1a, b).
|
Patient |
Gender |
Age |
Pre-anti-TB/ Pre-operation ESR(mm/h) |
Antitubercular therapy |
Post-operative investigate |
follow-up period (months) |
HSS |
||||
|
Pre-operation |
follow-up* |
||||||||||
|
Pre- operation (days ) |
Post- operation (months) |
Biopsy culture |
Acid-fast staining |
||||||||
|
1 |
F |
47 |
114/82 |
24 |
12 |
- |
+ |
78 |
18 |
92 |
|
|
2 |
F |
62 |
54/46 |
18 |
12 |
- |
- |
71 |
26 |
85 |
|
|
3 |
M |
53 |
69/51 |
15 |
12 |
- |
- |
63 |
42 |
89 |
|
|
4 |
F |
59 |
32/26 |
14 |
12 |
- |
- |
60 |
38 |
94 |
|
|
5 |
F |
67 |
48/44 |
94 |
12 |
M.TB |
- |
38 |
26 |
68 |
|
|
6 |
M |
56 |
70/49 |
17 |
12 |
- |
- |
26 |
31 |
94 |
|
|
7 |
M |
65 |
90/67 |
110 |
12 |
- |
+ |
30 |
36 |
74 |
|
|
8 |
F |
49 |
72/37 |
14 |
12 |
- |
+ |
24 |
42 |
90 |
|
ESR: erythrocyte sedimentation rate; HSS: hospital for special surgery knee score; M.TB: Mycobacterium tuberculosis
Table 1: Details of 8 patients with active tuberculosis of the knee.

Figure 1: A 62 years old female, suffering from right knee pain for 1 year, cannot walk for 2 months. a: obvious swelling in her right knee; b: the Phemister triad was shown on her anteroposterior and lateral radiographs.
Clinical suspicion and a well-documented history were the most important steps in the diagnosis of active TB of the knee. Magnetic resonance imaging (MRI) was carried out to define the extent of tuberculous infection. Computed tomography (CT) of lung and spine were obtained to rule out other active foci of concomitant tuberculous infection. Preoperative symptoms and elevated erythrocyte sedimentation rate (ESR) were used to evaluate preoperative activation and postoperative recurrence of TB. All patients were free from contraindications caused by other systems. The hospital for special surgery knee score (HSS) system was used to evaluate the function outcomes of the knees. The preoperative HSS scores were acquired at admission. Preoperative antitubercular drugs were administered once TB of the knee was diagnosed clinically. Preoperative drugs included isoniazid (300 mg, once daily), rifampicin (450 mg, once daily), ethambutol (750 mg, once daily), and streptomycin (750 mg/d, once daily×3 months in total). At admission a popliteal abscess was found in one patient (Case 5) and a recent onset discharging sinus tract in another (Case 7). These two patients were treated with two-stage TKA. The goal of the first stage of surgery was to debride the popliteal tuberculous abscess in Case 5 and eliminate the sinus tract for fear of mixed infection in case 7. The final stage of surgery was not performed until the incisions healed without complications. This interval was about 3 months and antituberculous medications were uninterrupted. Six other patients were treated with one-stage TKA. For these patients the preoperative antitubercular medication was given for 2 to 4 weeks to make the ESR decrease more than 20% or below 50mm/h. All TKA procedures were performed by a senior surgeon, using continuous epidural anesthesia and via a medial parapatellar approach. The surgical operation was in consistent with the common practices with inflammatory synovium and caseous substance being debrided thoroughly. A medical pulse irrigator was used in all patients after osteotomy and debridement were completed. A primary cemented posterior-stabilized prosthesis (Waldemar Link, Hamburg, Germany) was used in all cases. Local isoniazid (300 mg) and streptomycin (250 mg) were administered in joint cavity in all cases before the incisions were closed. Drainage was performed in all cases and removed 24 -48 hours after surgery. The resected tissues were sent for histopathologic examination, acid-fast staining and tuberculosis culture for further diagnosis. Antitubercular drugs were continued for 12 months after surgery in all patients. Cefuroxime was used for 72 hours to prevent additional infection postoperatively. Enoxaparin was used for two weeks to prevent deep venous thromboembolism. ESR was examined every two months postoperatively until it was below 20 mm/h. Follow-ups were performed every two months within the first 6 months and once per year. The postoperative HSS scores and radiographs were acquired every year after surgery. Re-aggravated knee pain, joint swelling, and disability were considered as possible recurrence of TB during the follow-up period and further investigation must be performed. Statistical analysis was made by Wilcoxon test using SPSS 19.0 statistical software (SPSS Inc., Chicago, IL, USA) to compare the preoperative and postoperative HSS scores of the patients. A value of p<0.05 was considered to be statistically significant.
3. Results
Intraoperatively synovial hyperplasia edema and worm-eaten damage of cartilage and subchondral bone were found in all patients. Caseous tissue was seen in five patients (Figure 2). An intraoperative complication happened in one patient (Case 5) whose tibia end of the patellar tendon was torn from the tubercle of tibia due to stiffness of the involved knee. The patellar tendon was fixed with two anchors. A semi-confined brace was used for six weeks after surgery. No postoperative complications such as pyogenic infection, deep vein thrombosis were observed during the follow-ups. Histopathologically, TB was confirmed by typical granulomatous lesions including epithelioid histiocytes surrounded by lymphocytes in all patients. Acid-fast staining bacilli were detected in three specimens and culture was positive in only one. The postoperative ESR decreased below 20mm/h within six months in all patients. Within an average follow-up period of 48.8(24-78) months no recurrence of TB was found. The average HSS score improved from 32.4 ± 8.6(18-42) points preoperatively to 85.6 ± 9.7(68-94) points at the most recent follow-up (p<0.001) (Table 1). All knees showed good integrity and all patients could ambulate without walking aids. The radiographs at the most recent follow-up did not reveal any loosening of the prostheses (Figure 3).

Figure 2: Synovial hyperplasia edema and worm-eaten damage of cartilage and subchondral bone were found intraoperatively. Caseous tissue was also obvious (white arrow).
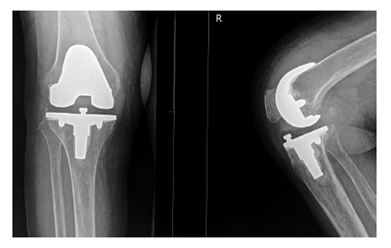
Figure 3: Anteroposterior and lateral radiographs 24 months after surgery, showing no signs of loosening of prosthesis.
4. Discussion
The most important finding of the present study was that 2 to 4 weeks of preoperative antitubercular therapy is enough for the patients with advanced active TB of the knee and a long infection-free interval is not a prerequisite for TKA. We recommend one-stage TKA for the patients with advanced active TB of the knee unless there is a discharging sinus tract or abscess that cannot be debrided during the surgery of TKA. In line with previous studies we recommend a long period of postoperative antitubercular therapy which should be at least 12 months after surgery to reduce the risk of local recurrence of TB [11-14,16,18]. TKA can provide the patients with quiescent TB of the knee with an excellent function, but joint replacement for active tuberculous infection is opposed by most authors because they believe that the risk of local recurrence of TB is too high [20]. Other authors recommend a long interval between the treatment of the active infection and arthroplasty [11,12,14,18]. They believe that a prolonged preoperative antitubercular therapy could decrease the reactivation risk of TB infection. However, the optimal timing of TKA for the patients with TB of the knee joint is still controversy. Su et al [11] reported sixteen cases of tuberculosis of the knee treated with TKA. Eight cases were treated with antitubercular therapy for 2 (3 cases) to 12 (5 cases) months before and 1 year after arthroplasty. Another 8 cases were not diagnosed primarily and therefore received only postoperative antitubercular therapy. Five cases had a recurrence of TB. Four of these 5 cases did not receive preoperative antitubercular treatment. The last case of recurrent infection occurred in a patient who had received longstanding corticosteroid therapy. They suggested that effective preoperative and postoperative antitubercular chemotherapy were mandatory for the prevention of tuberculous reactivation after TKA. Oztürkmen et al. [12] reported twelve patients with recent onset tuberculous arthritis of the knee. Two-stage TKA was performed in all patients with 7 primary prostheses and 5 revisions. The time interval between the first and the second stage was not more than 6 months. All patients were given postoperative antitubercular treatment for more than 1 year, and within an average follow-up period of 6.1 ± 1.8 years, no reactivation of tuberculous infection was found. Kim et al. [13] performed TKA in 19 patients (22 knees) with tuberculous arthritis of the knee. The interval between the subsidence of the signs of tuberculous infection and arthroplasty ranged from 3 months to 5 years. They found 3 recurrent cases during the follow-up. Habaxi et al. [14] analyzed 10 patients with active tuberculosis of the knee. One-stage TKA was performed in all cases. The patients were given preoperative antitubercular treatment for 2-4 weeks and more than 1 year postoperatively. They had one recurrent case. Our study is in line with Habaxi et al. In our series, preoperative antitubercular therapy was administered for 2-4 weeks in six patients and no recurrence was found at the most recent follow-up. Antitubercular treatment for more than 3 months was performed in two cases because the concomitant popliteal abscess and discharging sinus tract had to be eliminated before TKA. No recurrence of TB was found in these two cases. From the results of our study and reviews of previous studies we find that the recurrence of TB after TKA is not related to the duration of preoperative antitubercular treatment. The recurrence of TB after TKA may occur even when TB is quiescent for several years [13,19] while patients without preoperative antitubercular treatment may be free from recurrence even the tuberculous arthritis of the knee is active [11,16,21]. We recommend a short-term preoperative antitubercular treatment so as to shorten the course of the treatment of TB. In our opinion 2-4 weeks of preoperative antitubercular treatment is enough before TKA if there are no special conditions such as discharging sinus tracts or extra-articular abscesses that cannot be debrided through the incision of TKA. The reason that we recommend a short-term preoperative antitubercular treatment lies in that M. tuberculosis has specific behavioral characteristics differ from pyogenic bacteria [22]. M. tuberculosis reproduces slowly and has little tendency to adhere to an implant. In vitro studies also demonstrated that M. tuberculosis has little or no biofilm formation making it susceptible to antitubercular therapy [23]. So antitubercular drugs can eliminate M. tuberculosis efficiently even there is an implant. Even TB is reactivated after TKA, the disease can be controlled by antitubercular drugs alone or in combination with debridement without removal of the prosthesis in most cases [11,13,19,24]. As for postoperative antitubercular therapy our opinion is in line with others [11-14,16,18]. We recommend a long-term postoperative antitubercular therapy for at least 12 months. Once recurrence of TB is detected a longer antitubercular course is recommended until TB is cured. Debridement with or without removal of implants may be needed sometimes. Complete debridement of the infected tissues is considered to be the mainstay of the treatment to lower the potential risk of reactivation of TB [11-14]. Wide surgical debridement can eradicate the necrotic and infected tissues, and postoperative antituberculous therapy controls the residual foci. An aggressive debridement may decrease the need for a prolonged postoperative chemotherapy treatment. Complete debridement may require removal of the entire joint, including metaphyseal femoral and tibial bone proximal and distal to the joint line and sometimes the patellar bone. In this situation revision prosthesis may be needed [12]. Some authors recommend two-stage TKA for the patients with active tuberculous arthritis of the knee for fear increased reactivation risk of TB infection [12,18,25]. However, two-stage TKA may cause stiffness of the knee and continuous bone loss after the first-stage surgery and increase the difficulty of the operation of TKA. This may also impair the function of the knee and the life of the implant [12,25]. In our series, two-stage TKA was performed in two cases due to a popliteal abscess in one patient and a discharging sinus tract in another. The operation of two-stage TKA was more difficult than that of one-stage TKA due to the stiffness caused by less movement of the knee and adhesion after the first-stage surgery. At final follow-up, although no recurrence of TB was found the function of the knee of these two patients was poorer than that of the patients treated with one-stage TKA (Table 1). In our opinion, two-stage TKA for active tuberculosis of the knee is not recommended unless there is a discharging sinus tract or an extra-articular abscess that is unable to be removed with the single surgical approach which is needed for arthroplasty [12]. In fact, whether the patients with a discharging sinus tract or an extra-articular abscess could be treated with one-stage TKA safely deserves further study. Many investigators thought that the level of ESR implied a state of tuberculous arthritis. ESR is typically at above normal levels in recent-onset tuberculosis and at normal levels in the chronic or quiescent stage. The level of ESR is also considered as an indicator of the efficacy of antitubercular drugs [11,18]. We agree with these points. All patients in our case series had elevated ESR before surgery, suggesting activity of tuberculosis of the knee. In our study TKA was not performed until the level of ESR decreased more than 20% or below 50mm/h after at least two-week antitubercular therapy. This implies that the preoperative antitubercular therapy is effective. Normal ESR levels are not prerequisite for TKA because the level of ESR will decrease to a normal level with a combination of debridement and antitubercular therapy. The present study revealed that the level of ESR decreased to a normal level within six months in all cases.
5. Conclusions
TKA for advanced active tuberculosis of the knee is a safe procedure providing symptomatic relief and functional improvement. A long infection-free interval is not a prerequisite for TKA. Wide surgical debridement and adequate postoperative antitubercular chemotherapy are the mainstay to eradicate the infection and reduce the risk of reactivation of TB.
References
- For the WHO recommendations (2019).
- Adigun R, Singh R. Tuberculosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2020).
- Held MFG, Hoppe S, Laubscher M, et al. Epidemiology of Musculoskeletal Tuberculosis in an Area with High Disease Prevalence. Asian Spine J 11 (2017): 405-411.
- Johansen IS, Nielsen SL, Hove M, et al. Characteristics and clinical outcome of bone and joint tuberculosis from 1994 to 2011: a retrospective register-based study in Denmark. Clin Infect Dis. 61 (2015): 554-562.
- Qian Y, Han Q, Liu W, et al. Characteristics and management of bone and joint tuberculosis in native and migrant population in Shanghai during 2011 to 2015. BMC Infect Dis 18 (2018): 543.
- Sultan AA, Cantrell WA, Rose E, et al. Total knee arthroplasty in the face of a previous tuberculosis infection of the knee: what do we know in 2018? Expert Rev Med Devices 15 (2018): 717-724.
- Tang X, Zhu J, Li Q, et al. Knee arthrodesis using a unilateral external fixator combined with crossed cannulated screws for the treatment of end-stage tuberculosis of the knee. BMC Musculoskelet Disord 16 (2015): 197.
- Lim HC, Bae JH, Hur CR, et al. Arthrodesis of the knee using cannulated screws. J Bone Joint Surg Br 91 (2009): 180-184.
- Tuli SM. General Principles of Osteoarticular Tuberculosis.Clin Orthop Relat Res 398 (2002): 11-19.
- Bae DK, Yoon KH, Kim HS, et al. Total knee arthroplasty in stiff knees after previous infection. J Bone Joint Surg Br 87 (2005): 333-336.
- Su JY, Huang TL, Lin JY. Total knee arthroplasty in tuberculous arthritis. Clin Orthop Relat Res 323 (1996): 181-187.
- Oztürkmen Y, Uzümcügil O, Karamehmeto?lu M, et al. Total knee arthroplasty for the management of joint destruction in tuberculous arthritis. Knee Surg Sports Traumatol Arthrosc 22 (2014): 1076-1083.
- Kim YH. Total knee arthroplasty for tuberculous arthritis. J. Bone Joint Surg. Am 70 (1988): 1322-1330.
- Habaxi KK , Wang L, Miao XG, et al. Total knee arthroplasty treatment of active tuberculosis of the knee: a review of 10 cases. Eur Rev Med Pharmacol Sci 18 (2014): 3587-3592.
- Watts HG, Lifeso RM. Tuberculosis of bones and joints. J. Bone Joint Surg. Am 78 (1996): 288-298.
- Gale DW, Hading ML. Total knee arthroplasty in the presence of active tuberculosis. J Bone Joint Surg Br 73 (1991): 1006-1007.
- Wang Y, Wang J, Xu Z, et al. Total hip arthroplasty for active tuberculosis of the hip. Int Orthop 34 (2010): 1111-1114.
- Zeng M, Xie J, Wang L, et al. Total knee arthroplasty in advanced tuberculous arthritis of the knee. Int Orthop 40 (2016): 1433-1439.
- Eskola A, Santavirta S, Konttinen YT, et al. Arthroplasty for old tuberculosis of the knee. J Bone Joint Surg Br 70 (1988): 767-769.
- Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res 398 (2002): 93-99.
- Besser MI. Total knee replacement in unsuspected tuberculosis of the joint.Br Med J 280 (1980): 1434.
- Moon MS. Tuberculosis of spine: current views in diagnosis and management. Asian Spine J 8 (2014): 97-111.
- Ha KY, Chung YG, Ryoo SJ. Adherence and biofilm formation of Staphylococcus epidermidis and Mycobacterium tuberculosis on various spinal implants. Spine 30 (2005): 38-43.
- Haan JD, Vreeling AWJ, Hellemondt GGV. Reactivation of ancient joint tuberculosis of the knee following total knee arthroplasty after 61 years: a case report. Knee 15 (2008): 336-338.
- Leclere LE, Sechriest?VF, Holley KG, et Tuberculous arthritis of the knee treated with two-stage total knee arthroplasty. A case report. J Bone Joint Surg Am 91 (2009): 186-191.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 