Impact of Mechanical Aortic Prostheses in hospital stay and anticoagulation related complications
Ana Lopez-Marco1,2, Stuart W Grant3, Saifullah Mohamed5, Chiara Proli2, Dheeraj Mehta1, Aprim Youhana2, Ragheb Hasan3, Yasir Abu-Omar4, Nicolas Nikolaidis5
1Department of Cardiothoracic Surgery, University Hospital of Wales, Cardiff, UK
2Department of Cardiothoracic Surgery, Morriston Hospital, Swansea, UK
3Department of Cardiothoracic Surgery, Manchester Royal Infirmary, Manchester, UK
4Department of Surgery, Papworth Hospital, Cambridge, UK
5Department of Cardiothoracic Surgery, Royal Wolverhampton Hospital, Wolverhampton, UK
*Corresponding Author:Saifullah Mohamed, Department of Cardiothoracic Surgery, Royal Wolverhampton Hospital, Wolverhampton, UK
Received: 12 March 2021; Accepted: 18 March 2021; Published: 05 April 2021
Article Information
Citation:
Ana Lopez-Marco, Stuart W Grant, Saifullah Mohamed, Chiara Proli, Dheeraj Mehta, Aprim Youhana, Ragheb Hasan, Yasir Abu-Omar, Nicolas Nikolaidis. Impact of mechanical aortic prostheses in hospital stay and anticoagulation related complications. Journal of Surgery and Research 4 (2021): 187-196.
View / Download Pdf Share at FacebookAbstract
Objective: Use of mechanical valves requires long-term anticoagulation, which carries additional risks of bleeding and thrombosis. The aim of the study was to investigate the impact of anticoagulation on length of postoperative stay and the incidence of anticoagulation-related complications.
Methods: A multicentre study of prospectively collected data, including all patients below 65 years of age undergoing aortic valve replacement (± concomitant non-valvular procedures) was performed. Exclusion criteria included preoperative atrial fibrillation and other indications for anticoagulation, previous cardiac surgery, emergency operations and infective endocarditis. Primary end-points were length of hospital stay and anticoagulation-related complications within 6 weeks of discharge.
Results: A total of 1973 patients were included over a 5-year period from 5 centres in the UK. Mean patient age was 59 years (range 17-65 years). Mechanical valves were implanted in 52% of patients. The use of mechanical prostheses was associated with significantly prolonged postoperative stay (median of 7 vs. 6 days with bioprosthesis, p < 0.001) being an independent predictor of prolonged postoperative stay (> 8 days; OR 1.55, 95% CI 1.27-1.90, p < 0.001). On subanalysis, 1.4% of patients with mechanical prosthesis required readmission for anticoagulation-related complications within 6 weeks of discharge (including late tamponade). An additional 2% required repeated hospital attendance for INR stabilisation.
Conclusion: Use of mechanical valves in patients below 65 years of age is associated with both increased hospital stay and anticoagulation-related complications compared to bioprosthesis. The clinical and health economic implications of prosthesis choice should be considered by both the heart team and patient.
Keywords
<p>Anticoagulation, Mechanical prosthesis, Hospital stay, Complications, Health costs</p>
Article Details
1. Introduction
Aortic valve replacement is one of the commonest cardiac operations carried worldwide and according the SCTS audit registry over 5000 procedures being carried annually in the United Kingdom at present [1]. The selection of the appropriate valve prosthesis is a complex decision influenced by both patient and surgeon preferences. On one hand the mechanical prosthesis valves are characterized by excellent structural durability but require lifelong systemic anticoagulation, which itself carries its own risks of thromboembolism and bleeding. On the other hand, the biological valve prosthesis may avoid lifelong anticoagulation and its complications but face structural valve degeneration, often requiring a reoperation 10 to 15 years after implantation, or even more rapidly in young patients.
The current 2017 ESC/EACTS guidelines on valvular heart disease reflect that the prosthesis choice is left to the desire of the informed patient providing there are no contraindications for anticoagulation [2]. However, they recommend the use of mechanical valve prosthesis in aortic position in patients at risk of accelerated structural valve deterioration (i.e. below 40 years of age, hyperparathyroidism) and state that a mechanical prosthesis should be considered in patients below 60 years of age, on patients already on anticoagulation because of a mechanical prosthesis in another valve position or high risk for thromboembolism (i.e. atrial fibrillation, previous thromboembolism, hypercoagulable state and severe LV systolic dysfunction) and patients with a reasonable life expectancy (i.e. more than 10 years) for whom future redo valve surgery would be at high risk [2].
There is a steady decline in usage of mechanical valve prosthesis, even in patients below 65 years of age. Possible reasons are improvement on the technology of the biological prosthesis, making them more resistant towards the structural valve degeneration, and the desires of the well-informed patients to avoid long-life anticoagulation over a redo valve operation [3-5].
The aim of our study was to investigate the impact of systemic anticoagulation on postoperative length of stay and to investigate the incidence of anticoagulation-related complications within 6 weeks of discharge. Our initial hypothesis was that patients who received mechanical valve prosthesis had an increased hospital stay compared to patients receiving a biological prosthesis due to the time needed to stabilize the INR before discharge.
2. Methods
We conducted a multicentre, retrospective observational study of prospectively collected data from the 5 cardiac surgical participating centres (University Hospital of Wales, Cardiff; Morriston Hospital, Swansea; Manchester Royal Infirmary, Manchester; Papworth Hospital, Cambridge and Royal Wolverhampton Hospital, Wolverhampton). The number of patients recruited in each centre is displayed in table 1.
Inclusion criteria were consecutive patients below 65 years of age who underwent an aortic valve replacement with or without any other non-valvular concomitant procedures within the last five years in the 5 participating centres.
Exclusion criteria included preoperative atrial fibrillation and/or other indications for anticoagulation, previous cardiac surgery, emergency operations and infective endocarditis. Each patient made the choice of aortic valve prosthesis individually after an informed conversation with the corresponding surgical team based on current recommendations from the ESC/EACTS guidelines on valve heart diseases [2].
|
N |
% |
|
|
Morriston Hospital |
252 |
13% |
|
Manchester Royal Infirmary |
296 |
15% |
|
Royal Wolverhampton Hospital |
314 |
16% |
|
University Hospital of Wales |
330 |
17% |
|
Papworth Hospital |
781 |
40% |
Table 1: Number of patients included in the study from each contributing centre
Postoperative anticoagulation regimes were comparable in all centres, with all the patients who received a mechanical prosthesis being discharged on Warfarin, with a target INR of 2.5 (range 2 – 3) and the patients receiving a biological prosthesis being discharged predominantly on Aspirin, unless other indication for anticoagulation was present (i.e. atrial fibrillation in the postoperative period).
The aim of the study was to investigate the impact of anticoagulation on postoperative stay comparing mechanical and biological prosthesis and the presence of anticoagulation-related complications within 6 weeks of discharge.
2.1 Statistical analysis
Continuous variables are expressed as median ± inter-quartile range (IQR) as per non-normal distribution of data. Comparison between groups was performed with the Mann-Whitney U test. Categorical variables are expressed as percentages and compared using Chi-square/Fisher exact test as appropriate. Statistical significance level was defined as p < 0.05. A multivariable logistic regression model was used to identify the best predictors affecting postoperative hospital stay. The results were expressed as odds ratios (OR) with corresponding 95% confidence intervals (CI).
3. Results
Between January 2011 and December 2016, a total of 1973 patients below 65 years of age underwent aortic valve replacement with or without a concomitant non-valvular procedure in the 5 participating centres and therefore, were included for analysis. A total of 1018 patients (52%) received a mechanical prosthesis and 955 patients (48%) received a biological prosthesis.
Overall median age was 59 years (IQR 51-63 years); those receiving a mechanical prosthesis had a median age of 55 years (IQR 48-60 years), while those receiving a biological prosthesis were significantly older (61 years, (IQR 57-64 years)), p < 0.001. The majority of our patients were between 50 and 65 years of age; the percentage of patients according different groups of age is displayed in Figure 1.
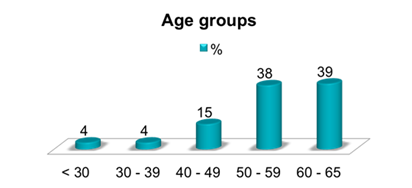
Figure 1: Percentage of patients according to age group.
Incidence of diabetes was significantly higher among the group of patients who received a biological valve. Regarding concomitant cardiac procedures, those who received a mechanical aortic prosthesis had associated surgery of the aorta more frequently than those who received a biological valve, whom in other hand received more concomitant coronary surgery. The rest of preoperative demographic characteristics were equivalent between the two groups and are reflected in similar EuroScore for the two groups. A detailed record of preoperative characteristics, ventricular function, urgency of the operation and the need for concomitant procedures are depicted in Table 2.
|
Mechanical N = 1018 (52%) |
Biological N = 955 (48%) |
P value |
|
|
Age (median, IQR) |
54.6 (48 – 60) |
61.4 (57 – 64) |
< 0.001 |
|
Female sex |
296 (29%) |
259 (27%) |
0.34 |
|
Renal failure |
18 (2%) |
18 (2%) |
0.87 |
|
COPD |
174 (17%) |
163 (17%) |
1 |
|
Diabetes |
145 (14%) |
181 (19%) |
0.005 |
|
NYHA III-IV |
413 (41%) |
399 (42%) |
0.61 |
|
CCS Angina III-IV |
137 (13%) |
117 (12%) |
0.46 |
|
Recent MI |
57 (6%) |
74 (8%) |
0.06 |
|
Impaired LV function |
244 (24%) |
251 (26%) |
0.25 |
|
Urgent surgery |
250 (24%) |
213 (22%) |
0.24 |
|
Concomitant CABG |
207 (20%) |
286 (30%) |
< 0.001 |
|
Concomitant aortic surgery |
267 (26%) |
152 (16%) |
< 0.001 |
|
Logistic EuroScore (median, IQR) |
2.3 (1.5 – 4.6) |
2.3 (1.5 - 4.4) |
0.96 |
Table 2: Demographic preoperative characteristics
IQR: interquartile range; COPD: Chronic obstructive pulmonary disease, NHYA: New York Heart Association Class; CCS: Canadian Cardiovascular Society Angina Class; MI: myocardial infarct.
The need for concomitant non-valvular cardiac surgery might have had an impact on the choice of the valve prosthesis. Those who required concomitant coronary revascularization, chose more frequently a biological prosthesis (30% vs. 20%) and those who underwent concomitant aortic surgery, chose more frequently a mechanical prosthesis (26% vs. 16%), p < 0.001 (Table 2).
3.1. Postoperative length of stay
We defined as ‘normal postoperative stay’ a length of 7 days or shorter, ‘prolonged postoperative stay’ as 8 days or longer and ‘very prolonged postoperative stay’ as 14 days or longer.
The overall median length of stay was 7.1 days (IQR 6.0 – 10.1 days) for the patients receiving a mechanical prosthesis and significantly shorter for those receiving a biological prosthesis (median 6.3 days (IQR 5.2 – 9.2 days), p = 0.001) (Table 3).
Patients who received a mechanical prosthesis had a significantly increased rate of prolonged length of stay (45%) compared to biological prosthesis (36%), p < 0.001 (Table 3).
|
Mechanical N = 1018 |
Biological N = 955 |
P value |
|
|
Length of stay (days, median, IQR) |
7.1 (6.0 - 10.1) |
6.3 (5.2 - 9.2) |
0.001 |
|
Prolonged LOS (≥ 8 days) |
460 (45%) |
341 (36%) |
< 0.001 |
|
Very prolonged LOS (≥ 14 days) |
137 (13%) |
115 (12%) |
0.42 |
Table 3: Postoperative length of stay (in days) for the patients receiving a mechanical aortic prosthesis or a biological aortic prosthesis.
However, the very prolonged postoperative stay (14 days or more) was not influenced by the choice of valve prosthesis (13% of patients who received a mechanical valve vs. 12% of those receiving a biological valve stayed 14 days or more, p = 0.42).
In both unadjusted analysis and adjusted analysis, the use of mechanical valve prosthesis was associated with a significantly increased postoperative length of stay. The adjusted analysis (by centre, demographics and postoperative complications) confirmed the use of mechanical valve prosthesis as an independent risk factor for prolonged postoperative stay (OR 1.55, 95% CI 1.3 – 1.9, p < 0.001). Other independent risk factors for prolonged postoperative stay identified by the adjusted analysis were: female sex (OR 1.4, 95% CI 1.1 – 1.7, p = 0.006), previous myocardial infarct (OR 1.55, 95% CI 1.3 – 2.1, p = 0.006), preoperative pulmonary disease (OR 1.9, 95% CI 1.5 – 2.5, p < 0.001), preoperative left ventricular dysfunction (OR 1.2, 95% CI 1.1 – 1.4, p = 0.02), urgent operation (OR 1.6, 95% CI 1.3 – 2.1, p < 0.001), other non-valvular concomitant cardiac procedure (OR 2.0, 95% 1.2 – 3.2, p = 0.005), reoperation for bleeding (OR 2.3, 95% CI 1.5 – 3.5, p < 0.001) and postoperative haemofiltration (OR 4.6, 95% CI 2.1 – 9.8, p < 0.001).
3.2. Anticoagulation-related complications within 6 weeks of discharge
The analysis of anticoagulation-related complications was performed in a subgroup of 1677 patients (the patients from Manchester Royal Infirmary were excluded as data was not available by the time of the analysis).
Immediate re-exploration for bleeding was defined as re-opening of the chest within 24 hours of the original operation, and as expected, it was equivalent for the two groups, independently of the type of prosthesis received (2% for the mechanical group and 3% for the biological group, p = 0.24). Re-exploration for tamponade was defined as re-opening of the chest beyond the first 24 hours and during the same admission. We found that the incidence of tamponade was higher in those who received a mechanical valve (1.5% vs. 0.6%), but the difference was not statistical significant (p = 0.06). We also analysed the incidence of anticoagulation-related complications within 6 weeks of discharge exclusively in the mechanical prosthesis group. We subdivided them in major complications, defined as those requiring a surgical procedure, or minor complications, defined as those that require re-admission in the primary cardiac centre but no surgical procedure.
From those who received a mechanical prosthesis, 11 patients (1.4%) were re-admitted for a major complication: 9 patients (1.1%) presented with delayed cardiac tamponade, managed with percutaneous drainage or surgical evacuation; 2 patients (0.2%) presented with large pleural effusions, managed with percutaneous drainage.
The analysis of minor complications was limited to patients who received a mechanical prosthesis in the two centres in Wales (n = 582). Six patients (2%) required re-admission in the primary cardiac centre for intravenous administration of heparin to treat a sub therapeutic INR. The length of these admissions varied between 2 and 4 days. Twenty-three patients (8%) required several visits to the primary cardiac centre ward for INR check and adjustment of anticoagulation doses. These extra ward attendances visits varied from 1 to 7 times per patient.
4. Discussion
The proportion of aortic mechanical prosthesis inserted has declined in the recent years, and that trend seems to be also applicable for patients below 65 years of age [3-5]. Possible factors towards and increase shift to biological prosthesis are to avoid the adverse effects associated with lifetime anticoagulation, the late generation of biological valves being less prone to degeneration, the lower risks of reoperation and the new emerging promising technologies such as the percutaneous ‘valve-in-valve’ implantation for possible re-dos. In our cohort of patients, the trend of use of aortic mechanical prosthesis with respect to biological prosthesis in patients below 65 years of age has also been declining, having been below 50% for the last 2 years (Figure 2).
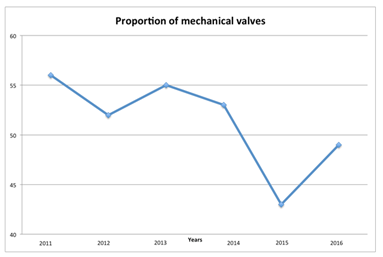
Figure 2: Percentage of aortic mechanical prosthesis inserted in patients below 65 years of age (with respect to biological prosthesis) for each year of the study.
Survival comparison between mechanical and biological valve prosthesis was conducted many years ago with 3 randomized control trials, two of them conducted in the 1970-80s and assessing first-generation valve prosthesis. Both the Veteran Affairs Cooperative Study and the Edinburgh randomized trials reported superior survival for mechanical over biological prosthesis although this results need to be interpreted carefully as they also reported higher perioperative mortality than the current standards and the valves analysed are not longer available in the market [6-8]. However, data from a most recent randomized control trial, meta-analysis and the SCTS Registry, also confirmed longer survival with mechanical aortic valves and several observational studies have examined late survival after AVR using contemporary biological and mechanical valves, specifically in cohorts of patients below 60, 65 and 70 years of age, also confirming a survival benefit for those receiving a mechanical valve [9-14].
Regarding prosthetic valve complications, the old randomized control trials reported reoperation due to structural valve degeneration being more frequent in patients receiving a biological prosthesis, and bleeding being more frequently in those receiving a mechanical prosthesis, with no differences in thromboembolic complications or endocarditis [6-8]. More recent studies, have reported equivalent bleeding rates, which can also be explained by the fact that some of the patients receiving a biological prosthesis are kept on anticoagulation [12-14]. The risk of haemorragic stroke associated with Warfarin has been reported to be independent of age, however other major bleeding events seem to be higher in patients above 60 years of age [15].
The structural valve degeneration associated with the biological prosthesis has been broadly studied. A meta-analysis reported that biological prosthesis can be used for patients as young as 56 years of age without adverse impact on their life expectancy, and events-free life expectancy is expected up to age of 63 years [16]. Ferrari and colleagues, analysed clinical outcomes of biological aortic valve replacement in patients below 65 years of age and reported that the reoperation for structural valve degeneration occurred exclusively among patients below 56 years of age, with the median interval to reoperation being 13 years for those between 40 and 60 years of age and 8 years for those below 40 years [17].
The microstimulation model created by Takkemberg et al. to weigh the anticoagulation-related events versus the reoperation risk concluded that despite an equivalent total life expectancy with both biological and mechanical prosthesis, the event-free life expectancy is better with a bioprosthesis, mainly because of the lower risk of bleeding. They reported a 25% risk of reoperation for structural valve degeneration for patients of 60 years of age compared to a 41% lifetime risk of bleeding with a mechanical prosthesis. Also, the mortality from bleeding was reported as high as 22% compared to 7% mortality risk after reoperation [18].
In our study, we were not focused on the clinical outcomes but on the impact of the choice of valve prosthesis in the length of hospital stay. We identified the choice of a mechanical prosthesis as an independent risk factor for increased postoperative length of stay, increasing the stay a median of 0.8 days. The overall median length of stay was 7.1 days (IQR 6.0-10.1 days) for the patients receiving a mechanical prosthesis and 6.3 days (IQR 5.2-9.2 days), for those receiving a biological prosthesis, p = 0.001.
Contributing factors to this increase in hospital stay are the need for long-life anticoagulation with Warfarin in patients who received a mechanical prosthesis, requiring at least two consecutive days of stable therapeutic INR (> 2.0) before considering discharge the patients to the community INR clinic. Timing the removal of the temporary epicardial pacing wires to the warfarin dosage is paramount to avoid unnecessary delays in discharge due to high INRs prohibiting the removal of pacing wires. In all the participating centres, treatment with warfarin is started on postoperative day 1, with pacing wire removal planned for day 4 unless need for pacing. The INR thresholds accepted for the removal of the pacing wires varied between centres and consultants, with an INR range of acceptance between 2.0-2.5.
Discharge from the hospital is accepted in the majority of the centres once the INR has been within therapeutic range (INR > 2.0), with the target INR for current aortic mechanical prosthesis being 2.5 (2.0-3. 0). However, not in all regions, the community services accept managing patients with suboptimal INR (either sub-therapeutic requiring intravenous heparin infusion or supra-therapeutic requiring reversal with vitamin K), hence the rate of re-admissions to the primary cardiac centre to treat those anticoagulation-related problems.
The figures of anticoagulation-related complications are most probably underestimated, as some of these patients would have been treated in their local referring center for most of the complications analysed apart from the cardiac tamponade. Also the existence of a valve clinic in some of the participating centres allows an accurate control of the INR minimizing or even elimination the need for the patients to be re-admitted in the ward or generate extra costs of INR monitoring in the primary cardiac ward.
Conc5.lusion
The use of mechanical valve prosthesis in patients below 65 years of age is associated with increased postoperative hospital stay compared to use of biological prosthesis. We also identified the presence of significant anticoagulation-related complications within 6 weeks of discharge that implied re-admission or revisiting the original cardiac centre for treatment, with the correspondent health economic implications.
Therefore, we conclude that not only clinical but also health-economic reasons should be considered by both the heart team and the patient when making the informed decision on valve prosthesis choice.
Funding statement
This study was supported by an Educational Grant from Edwards Lifesciences.
References
- Blue Book. The Society for Cardiothoracic Surgery in Great Britain and Ireland. Results from 2006 to 2015. Available online at www.bluebook.scts.org.
- 2017 ESC/EACTS guidelines for the management of valvular heart disease. Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ et al. Eur Heart J 38 (2017): 2739-2786.
- Suri RM, Schaff HV. Selections of aortic valve prostheses: contemporary reappraisal of mechanical versus biologic valve substitutes. Circulation 128 (2013): 1372-1380.
- Kaneko MD, Cohn LF, Aranki SF. Tissue valve is the preferred option of patients aged 60 and older. Circulation 128 (2013): 1365-1371.
- Niclauss, von Segesser LK, Ferrari E. Aortic biological valve prosthesis in patients younger than 65 years of age: transition to a flexible age limit? Interact Cardiovasc Thorac Surg (2013): 501-508.
- Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, et al. Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial. J Am Coll Cardiol 36 (2000): 1152-1158.
- Bloomfield P, Wheatley DJ, Prescott RJ, Miller HC. Twelve-year compari- son of a Bjork-Shiley mechanical heart valve with porcine bioprostheses. N Engl J Med 324 (1991): 573-579.
- Oxenham H, Bloomfield P, Wheatley DJ, lee RJ, Cunningham J, et al. Twenty year comparison of a Bjork-Shiley mechanical heart valve with porcine bioprostheses. Heart 89 (2003): 715-721.
- Stassano P, Di Tommaso L, Monaco M, Iorio F, Pepino P, et al. Aortic valve replacement: a prospective randomized evaluation of mechanical versus biological valves in patients ages 55 to 70 years. J Am Coll Cardiol 54 (2009): 1862-1868.
- Dunning J, Gao H, Chambers J, Moat N, Murphy G, et al. Aortic valve surgery: Marked increases in volume and significant decreases in mechanical valve use an analysis of 41,227 patients over 5 years from the society for cardiothoracic surgery in Great Britain and Ireland national database. J Thorac Cardiovasc Surg 142 (2011): 776-782.
- lund O, Bland M. Risk-corrected impact of mechanical versus bioprosthetic valves on long-term mortality after aortic valve replacement. J Thorac Cardiovasc Surg 132 (2006): 20-26.
- Weber A, Noureddine H, Englberger l, Dick F, Gahl B, et al. Ten-year comparison of pericardial tissue valves versus mechanical prostheses for aortic valve replacement in patients younger than 60 years of age. J Thorac Cardiovasc Surg. 144 (2012): 1075-1083.
- Badhwar V, Ofenloch JC, Rovin JD, Van Gelder HM, Jacobs JP. Noninferiority of closely monitored mechanical valves to bioprostheses overshadowed by early mortality benefit in younger patients. Ann Thorac Surg 93 (2012): 748-753.
- Brown Ml, Schaff HV, Lahr BD, Mullany CJ, Sundt TM, et al. Aortic valve replacement in patients aged 50 to 70 years: Improved outcome with mechanical versus biologic prostheses. J Thorac Cardiovasc Surg. 135 (2008): 878-884.
- Swinkels BM, de Mol BA, Kelder JC, Vermeulen FE, Berg JM. Long-term bleeding events after mechanical aortic valve replacements in patients under the age of 60. Neth Heart 23 (2015): 111-115.
- Stoica S, Goldsmith K, Demiris N, Punjabi P, Berg G, et al. Microsimulation and clinical outcomes analysis support a lower age threshold for use of biological valves. Heart 96 (2010): 1730-1736.
- Chan V, lam BK, Rubens FD, Hendry P, Masters R, et al. Long-term evaluation of biological versus mechanical prosthesis use at reoperative aortic valve replacement. J Thorac Cardiovasc Surg 144 (2012): 146-151.
- Van Geldorp MWA, Jamieson WRE, Kappetein AP, Ye J, Fradet GJ, Eijekemans MJC et al. Patient outcome after aortic valve replacement with a mechanical or biological prosthesis: weighing lifetime anticoagulant related event risk against reoperation risk. J Thorac Cardiovasc Surg 137 (2009): 881-886.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 