The Time-related role of early pH, Base excess and Lactate for the Development in Sepsis in Polytrauma patients. An analysis using the IBM Watson Trauma Pathway Explorer
Philipp Vetter1, Jan Hambrecht1, Cédric Niggli1, Hans-Christoph Pape1, Ladislav Mica1*
1Department of Trauma Surgery, University Hospital Zurich, 8091 Zurich, Switzerland
*Corresponding Author: Prof. Dr. med. Ladislav Mica, Department of Trauma Surgery, University Hospital Zurich, 8091 Zurich, Switzerland.
Received: 15 July 2023; Accepted: 24 July 2023; Published: 18 August 2023
Article Information
Citation: Philipp Vetter, Jan Hambrecht, Cédric Niggli, Hans-Christoph Pape, Ladislav Mica. The time-related role of early pH, base excess and lactate for the development in sepsis in polytrauma patients. An analysis using the IBM Watson Trauma Pathway Explorer. Journal of Surgery and Research. 6 (2023): 283-291.
View / Download Pdf Share at FacebookAbstract
The Time-related role of early pH, Base excess and Lactate for the Development in Sepsis in Polytrauma patients. An analysis using the IBM Watson Trauma Pathway Explorer
Keywords
<p>Watson Trauma Pathway Explorer, Polytrauma, Sepsis</p>
Article Details
1. Introduction
Triaging of polytrauma patients is essential after admission to trauma bay. Besides clinical evaluation, numerous laboratory parameters are considered to evaluate injury severity and risk of subsequent adverse events (AE) such as systemic Inflammatory Respiratory Syndrome (SIRS), sepsis and death [1-11]. Anticipation and awareness of such aspects may be helpful in treatment decisions, being pharmaceutical or operative. The Watson Trauma Pathway Explorer® represents an outcome prediction tool that prognosticates the occurrence of SIRS and sepsis within 21 days and death within 72h [2-8,12]. The tool is based on an internal data base from more than 3500 patients with ongoing admission. Its main advantage is the ability to reference values according to fixed time points since admission, thereby allowing for continuous re-assessment. Lactate is an established parameter in estimating the risk for sepsis and mortality of polytrauma patients [1,7,9-11]. It is often a sign of hypoperfusion [13] but can also suggest a disease state or adrenergic process, for example in polytrauma cases [14-17]. Here, trauma-caused cell debris may lead to an immunologic response resembled as SIRS [18]. This, in turn, can further complicate into sepsis in a severe or shock state, accompanied by multiple organ damage and hypotension [19,20]. The association between lactate levels and AE generally appears to be linear [10,21,22] and related to injury severity [23,24]. This could explain the heterogenic aspect of lactate cut-off values indicating a substantial risk for AE, including a threshold of > 2 [mmol/L] [25,26], intermediately elevated values (2.0 - 3.9 [mmol/L]) [9,27,28] and a value greater than 4.0 [mmol/L] [10,11]. In combination with changes over time in the posttraumatic course, decision making on the basis of this parameter can be very challenging. Base excess (BE) is a parameter for acid-base dysbalance and physiologically lies within -2 and +2 mmol/L. In the trauma setting, it often implies tissue hypoperfusion by means of acidosis [29-31] and was found to be a predictive factor for mortality in polytrauma patients [32]. pH, on the other hand, represents a direct parameter that comprises the effects of oxygen debt, metabolic dysbalance (e.g. indicated by BE) and compensatory mechanisms [33]. Its comprehensiveness makes acidotic values (< 7.35) indicative of a serious morbidity, although the high rate of confounding aspects makes it less sensitive to minor changes [30,34]. Our aim was to analyze the time-dependent of pH, BE and lactate for sepsis development in polytrauma patients.
2. Methods
Patient cohort
Retrospective data from 3653 patients (1996-2022) from our institutional database, with ongoing implementation, were used for analysis in the Watson Trauma Pathway Explorer. We included polytrauma patients aged ≥ 16 years with an Injury Severity Score (ISS) ≥ 16 [35] retrospectively. Complete datasets were required. Excluded were patients that had not survived until admission or patients that were referred from external hospitals. According to the development of sepsis within the observational period of 21 days, two groups were formed. For all patients, pH, BE and lactate values were measured at previously defined time points (admission, 1, 2, 3, 4, 6, 8, 12, 24, and 48 h) after admission to our trauma bay at the University Hospital Zurich [5,7,8].
Definition of sepsis
Based on the most extreme values in leucocyte count, respiratory rate, heart rate and temperature, the SIRS score was calculated each day [36]. It was calculated for the time frame of hospitalization. Sepsis was defined as a SIRS score ≥ 2 with a focus of infection [19], and had to occur within the observational time frame of 21 days.
Laboratory analysis
Lactate levels [mmol/L] as well as pH and Base excess [mmol/L] were measured at the Institut für Klinische Chemie at the University of Zurich in a standardized blood gas analyzer (Radiometer ABL 825 Flex, Radiometer RSCH GmbH, Thalwil, Switzerland) The same procedure of measurement was applied at each time point.
Statistical analysis
Patients’ baseline characteristics are described as means with standard deviations (SD) for numerical variables, as medians with interquartile ranges (IQR) for ordinal data and as percentages for binary variables. An unpaired t-test for numerical variables and a Mood’s median test for ordinal variables were used for assessing differences between the two groups. Differences between groups according to the presence of sepsis were analyzed using the Mann-Whitney-U-Test due to a missing normal distribution according to a Q-Q-plot and an unequal variance.
Binary logistic regression was performed to analyze pH, BE and lactate as independent prediction factors for sepsis. Analysis was corrected for ISS, age and gender, as these factors were previously confirmed as notable factors [10,21, 22,37-39]. For this binary logistic regression, groups were split according to generally accepted threshold values of pH (< 7.35), BE (< -2 mmol/L) and lactate (> 2 or 4 mmol/L) [10,11,25,26].
Calculation of threshold values between the two groups (sepsis development) at each timepoint was performed according to the closest top-left threshold method, presenting the threshold point closest to the top-left corner of the receiver operating characteristic.
SPSS 29.0 (IBM SPSS Statistics 29) served for data analysis. The level of significance was set a p < 0.05.
Ethical approval
This study was conducted according to the guidelines for good clinical practice and the Helsinki guidelines. Research was based on the TRIPOD statement, representing a guideline for multivariable prediction model [40]. Ethical approval for analysis of patient data was granted by the ethical committee of the University Hospital Zurich and the government of Zurich upon the development of the database (Nr. StV: 1-2008) and reapproved for development of the Watson Trauma Pathway Explorer® (BASEC 2021-00391).
3. Results
Patient cohort
We included 3653 patients with a mean age of 45.8 ± 20.2 years, with 73.4% being male (Table 1). Sepsis cases displayed higher values for the (New) Injury Severity Score (NISS), Injury Severity Score (ISS) and the Acute Physiology and Chronic Health Evaluation (APACHE)-II-Score, as well as a younger age.
|
Baseline characteristic |
Overall patient sample N = 3653 |
Patients with developed Sepsis N = 547 |
Patients without developed sepsis N = 3106 |
p-value |
|
Age (mean, SD) |
45.8 ± 20.2 |
42.8 ± 18.1 |
46.3 ± 20.5 |
0.0002 |
|
Male |
73.4%; N=2681 |
78.6%; N=430 |
72.4%; N=2251 |
- |
|
Early death within 72h |
19.3%; N=708 |
1.46%; N=8 |
22.5%; N=700 |
- |
|
Blunt trauma |
91.3%; N=3336 |
94.7%; N=518 |
90.7%; N=2818 |
- |
|
Head injury |
38.3%; N=1400 |
44.8%; N=245 |
37.2%; N=1155 |
- |
|
BMI at admission (mean, SD) |
25 ± 4.4 |
25.9 ± 4.4 |
24.8 ± 4.3 |
<0.001 |
|
ISS (median, IQR) |
25 (17–34) |
30 (25–41) |
25 (17–34) |
<0.001 |
|
NISS (median, IQR) |
34 (25–50) |
41 (33–50) |
34 (24–48) |
<0.001 |
|
APACHE II at admission (median, IQR) |
14 (7–21) |
17 (11–21) |
13 (6–21) |
<0.001 |
|
GCS at admission (median, IQR) |
10 (3–15) |
3 (3–14) |
11 (3–15) |
<0.001 |
|
Temperature at admission (mean ± SD) |
35.5 ± 1.7 |
35.4 ± 1.7 |
35.6 ± 1.7 |
0.131 |
|
Systolic blood pressure at admission (mean ± SD) |
130.7 ± 27.6 |
128.5 ± 27.7 |
131.2 ± 27.5 |
0.0715 |
|
Prothrombin time at admission (median ± IQR) |
84 (65–97) |
80 (61–92) |
85 (66–98) |
0.1257 |
|
Hemoglobin at admission (mean ± SD) |
11.4 ± 4 |
11 ± 2.8 |
11.5 ± 4.2 |
0.005 |
|
CRP at admission (mean ± SD) |
13.74 ± 41.21 |
23.15 ± 62.96 |
11.94 ± 35.32 |
< 0.001 |
|
pH at admission (mean ± SD) |
7.31 ± 0.13 |
7.30 ± 0.15 |
7.32 ± 0.13 |
0.00632 |
|
pH at 1 h (mean ± SD) |
7.31 ± 0.15 |
7.29 ± 0.13 |
7.31 ± 0.15 |
< 0.001 |
|
pH at 2 h (mean ± SD) |
7.33 ± 0.12 |
7.32 ± 0.09 |
7.33 ± 0.13 |
0.002 |
|
pH at 3 h (mean ± SD) |
7.34 ± 0.14 |
7.33 ± 0.19 |
7.35 ± 0.13 |
0.003 |
|
pH at 4 h (mean ± SD) |
7.36 ± 0.14 |
7.35 ± 0.08 |
7.36 ± 0.15 |
0.003 |
|
PCT at admission (mean ± SD) |
1.23 ± 4.3 |
0.48 ± 0.56 |
1.15 ± 4.86 |
0.559 |
|
BE at admission (mean ± SD) |
-3.77 ± 5.27 |
-4.29 ± 4.97 |
-3.67 ± 5.32 |
< 0.001 |
|
BE at 1 h (mean ± SD) |
-4.57 ± 5.29 |
-5.23 ± 5.14 |
-4.40 ± 5.31 |
< 0.001 |
|
BE at 2 h (mean ± SD) |
-4.05 ± 4.51 |
-4.45 ± 4.32 |
-3.94 ± 4.56 |
0.009 |
|
BE at 3 h (mean ± SD) |
-3.67 ± 4.24 |
-4.16 ± 3.75 |
-3.54 ± 4.34 |
0.001 |
|
BE at 4 h (mean ± SD) |
-3.05 ± 3.81 |
-3.40 ± 3.89 |
-2.96 ± 3.79 |
0.034 |
|
Lactate at admission (mean, SD) |
2.94 +- 2.53 |
2.94 +- 2.27 |
2.94 +- 2.58 |
0.943 |
|
Lactate at 1 hours (mean, SD) |
2.76 +- 2.42 |
2.77 +- 2.15 |
2.75 +- 2.48 |
0.941 |
|
Lactate at 2 h (mean ± SD) |
2.63 ± 2.35 |
2.95 ± 2.45 |
2.54 ± 2.32 |
0.035 |
|
Lactate at 3 h (mean ± SD) |
2.58 ± 2.25 |
2.89 ± 2.32 |
2.50 ± 2.23 |
0.011 |
|
Lactate at 4 h (mean ± SD) |
2.51 ± 2.14 |
2.90 ± 2.33 |
2.41 ± 2.07 |
< 0.001 |
|
Lactate at 6 h (mean ± SD) |
2.33 ± 1.87 |
2.63 ± 1.85 |
2.24 ± 1.87 |
0.00123 |
|
Lactate at 8 h (mean ± SD) |
2.13 ± 2.44 |
2.46 ± 1.74 |
2.05 ± 2.59 |
0.00851 |
|
Lactate at 12 h (mean ± SD) |
1.69 ± 1.37 |
2.10 ± 1.55 |
1.58 ± 1.30 |
< 0.001 |
|
Lactate at 24 h (mean ± SD) |
1.38 ± 1.15 |
1.71 ± 1.17 |
1.30 ± 1.22 |
< 0.001 |
|
Lactate at 48 h (mean ± SD) |
1.19 ± 1.02 |
1.47 ± 1.00 |
1.09 ± 1.01 |
< 0.001 |
Table 1: Baseline characteristics of the total patient cohort and groups according to development of sepsis. pH, BE and lactate values are shown from admission onwards. Age [years], temperature [°C], Systolic blood pressure [mmHg], Prothrombin time [%], Hemoglobin [g/dL], CRP [mg/L], PCT [ng/mL], Lactate [mmol/L].
3.1 Parameter levels according to the development of sepsis
Between the two groups according to sepsis development, differences in pH existed from admission on and persisted for slightly more than four hours (Figure 1). Similar results were observed for BE, which differed over roughly six hours.
Lactate, on the other hand, showed no initial differences between groups, but differed from the second hour onwards until the end of the observational period of 21 days.
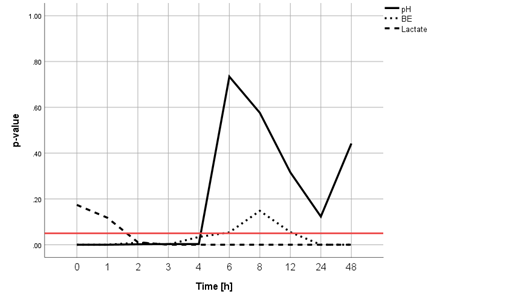
Figure 1: Comparison of parameter levels between the sepsis and non-sepsis group. There were significant differences in pH (continuous line) from admission onwards, which persisted for slightly more than 4 hours. Similar results were observed for BE (dotted line), which differed over roughly 6 hours. Lactate (dashed line), on the other hand, showed no initial differences between groups, but differed from the second hour onwards. The straight horizontal red line indicates the level of significance (p = 0.05).
3.2 Parameters as independent predictors for sepsis
Binary logistic regression revealed pH (< 7.35; p = 0.035), lactate (> 4 mmol/l; p = 0.006) at 4 h and BE at 6 h (< - 2 mmol/L; p = 0.022) as independent predictors (Figure 2), representing a statistically significant model (p = 0.037). There was a tendency for lactate with a cut-off of 2 mmol/l at 2 h to also be significantly predictive (p = 0.052).
pH, BE and lactate showed a correlation with each other (pH – lactate: r = -0.654; p <0.001; pH – BE: r = 0.804; p < 0.001; BE – lactate: r = -0.730; p < 0.001).
Analysis was corrected for ISS, age and gender, as each parameter at admission showed a correlation with the ISS (pH: r = - 0.256; p < 0.001; BE: r = -0.247; p < 0.001; lactate: r = 0.193; p < 0.001) and age (pH: r = 0.048; p = 0.016; BE: r = 0.06; p = 0.002; lactate: r = - 0.049; p = 0.007), Additionally, lactate and pH at admission were higher in men (lactate: p < 0.001; pH: p < 0.001).
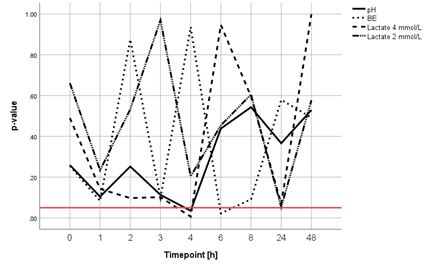
Figure 2: Significance of pH (continuous line), BE (dotted line) and lactate (dashed line/mixed dashed and dotted line) being independent predictors of sepsis adjusted for ISS, age and gender. Binary logistic regression revealed a pH < 7.35 and lactate > 4 mmol/L at 4 h after admission and a BE < -2 mmol/L 6 h after admission as independent predictors of sepsis. The straight horizontal red line indicates the level of significance (p = 0.05).
3.3 Time-dependent threshold values for sepsis.
The threshold values for pH were in the acidic range (< 7.35) for the first two hours after admission before reaching the lower limit of the normal range and turning more neutral thereafter (Figure 3).
For BE, threshold values initially revolved around – 4 mmol/L in the first four hours before reaching the lower limit of the normal range at around six hours, from there on also trending towards the central neutral range (Figure 4).
Lactate has been analyzed in a previous study [7] regarding this aspect and is therefore not depicted in an analogous manner.
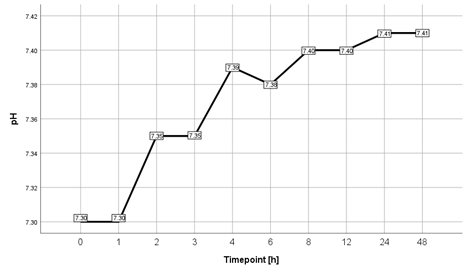
Figure 3: Time-dependent threshold values for pH for sepsis according to the closest top-left threshold method. Values were acidic for the first two hours after admission before reaching the lower limit of the normal range and turning more neutral thereafter.
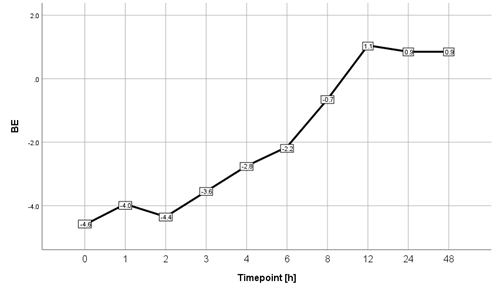
Figure 4: Time-dependent threshold values of BE for sepsis according to the closest top-left threshold method. After initial values of around -4 mmol/L, values reaching the lower limit of the normal range at around 6 hours and from there on trended towards more neutral ranges. Values are given as [mmol/L].
4. Discussion:
After previous analyses [5-8], the Watson Trauma Pathway Explorer® allowed time-dependent insights on the role of pH, BE and lactate regarding the prediction of sepsis in polytrauma patients. The main finding of our study are the early differences in pH, BE and lactate for patients developing sepsis after polytrauma. More specifically, acidic values in pH, BE and lactate were found to be relevant independently within six hours after admission. Threshold values also showed that pH and BE normalized within three to six hours. The parameters are confirmed in their (early) clinical relevance in association with posttraumatic complications [29-34, 41-45], as values differed early, while corrected for injury severity according to the ISS, age and gender [10,21,22,37-39]. There was a respective correlation between the three factors of interest. pH, due to its comprehensiveness, is interpreted as a value affected by BE and lactate. However, it is not only seen in the mere light of bleeding [33], but must also be seen in a multifactorial etiology, associated with the immune system related to complement pathway activation [46-48]. Regarding the time course, threshold values could be defined, being less severe than values in studies reporting on mortality rates [30,32-34]. These intermediately altered parameters may help the treating trauma team to assume when values should return to the normal range, which appears to revolve around the 6 h mark [30]. It appears that this time frame of 4 to 6 h after admission represents the time window of avoiding sepsis. Besides facilitated immediate treatment or prevention measures, being pharmaceutical (fluids, pain relievers, antibiotics, vasopressors or corticosteroids) or surgical (damage-control surgery vs. early total care), the outcome prediction tool allows for constant re-assessment when the patient may have been stabilized hemodynamically but is yet subject to major treatment. In this case, treatment should also be aimed at avoiding an exuberant physiologic response, possibly manifesting in the form of immunosuppression-triggered sepsis. Ultimately, the regression of the researched laboratory parameters to physiological ranges is concordant with the theory of SIRS and CARS (Compensatory Anti-inflammatory Response Syndrome) [49,50], as the early inflammatory response (SIRS) is followed by CARS. Limitations of this study mainly include the non-consideration of patient related confounding variables (e.g. morbidities, injuries according to body region) as well as changes in treatment methods over the long time-frame of inclusion. Restricting confounding was intended by correcting for age, gender and ISS. The short time period for recording the values of interested is due to their exclusive measurement on our interne intensive care units. Our insights ought to provide guidance for the treatment of polytrauma patients in reference to the analyzed parameters. In doing so, anticipation and timely measures shall be facilitated to maximize therapeutic effects while minimizing the risk for complications. Despite the advancements in polytrauma patient analysis using the Watson Trauma Pathway Explorer®, analysis and inclusion of further surrogative parameters is required to warrant a more precise prediction.
5. Conclusion
Between the two groups according to the development of sepsis, differences in pH existed within the first 4 hours, compared to BE within the first 6 hours. Lactate showed no initial differences between groups but differed from the second hour onwards. Binary logistic regression identified pH (< 7.35) and lactate (> 4 mmol/l) at 4 h as well as BE at 6 h (< - 2 mmol/L; p = 0.022) as independent predictors for sepsis. Threshold values for pH between groups were acidic for the first two hours after admission before reaching the lower limit of the normal range. For BE, threshold values initially revolved around – 4 mmol/L in the first 4 hours before reaching the lower limit of the normal range at around 6 hours. Our insights ought to provide guidance for the treatment of polytrauma patients in reference to the analyzed parameters. In doing so, anticipation and timely measures shall be facilitated to maximize therapeutic effects while minimizing the risk for complications. Despite the advancements in polytrauma patient analysis using the Watson Trauma Pathway Explorer®, analysis and inclusion of further surrogative parameters is required to warrant a more precise prediction.
Comment: Watson Trauma Pathway Explorer © by Ladislav Mica and IBM®.
Author contributions
P.V.: Data curation, Formal analysis, Investigation, Software, Visualization, Writing – original draft.
J.H.: Data curation, Project administration, Software, Writing - review & editing.
C.N.: Data curation, Project administration, Software, Writing - review & editing.
H.-C.P: Data curation, Project administration, Software, Writing - review & editing.
L.M.: Conceptualization, Data curation, Investigation, Methodology, Project administration,
Resources, Supervision, Validation, Writing - review & editing.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or nonfinancial interest in the subject matter or materials discussed in this paper. The authors declare no conflict of interest related to the submitted study.
References
- Billeter A, Turina M, Seifert B, et al. Early serum procalcitonin, interleukin-6, and 24-hour lactate clearance: useful indicators of septic infections in severely traumatized patients. World J Surg 33 (2009): 558-566.
- Mica L, Furrer E, Keel M, et al. Predictive ability of the ISS, NISS, and APACHE II score for SIRS and sepsis in polytrauma patients. Eur J Trauma Emerg Surg 38 (2012): 665-671.
- Mica L, Vomela J, Keel M, et al. The impact of body mass index on the development of systemic inflammatory response syndrome and sepsis in patients with polytrauma. Injury 45 (2014):253-258.
- Mica L, Rufibach K, Keel M, Trentz O. The risk of early mortality of polytrauma patients associated to ISS, NISS, APACHE II values and prothrombin time. J Trauma Manag Outcomes 7 (2013): 6.
- Mica L, Pape HC, Niggli P, et al. New Time-Related Insights into an Old Laboratory Parameter: Early CRP Discovered by IBM Watson Trauma Pathway Explorer© as a Predictor for Sepsis in Polytrauma Patients. J Clin Med 10 (2021): 5470.
- Niggli C, Pape HC, Niggli P, et al. Validation of a Visual-Based Analytics Tool for Outcome Prediction in Polytrauma Patients (WATSON Trauma Pathway Explorer) and Comparison with the Predictive Values of TRISS. J Clin Med 10 (2021): 2115.
- Vetter P, Niggli C, Hambrecht J, et al. The Role of Lactate for Sepsis in Polytrauma Patients, a Time related Analysis using the IBM Watson Trauma Pathway Explorer®. J Surg Res (Houst) 5 (2022): 618-624.
- Niggli C, Vetter P, Hambrecht J, et al. IBM WATSON Trauma Pathway Explorer© as a Predictor for Sepsis after Polytrauma - Is Procalcitonin Useful for Identifying Septic Polytrauma Patients? J Surg Res (Houst) 5 (2022): 637-644.
- Mikkelsen ME, Miltiades AN, Gaieski DF, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med 37 (2009): 1670-1677.
- Shapiro N I, Howell M D, Talmor D, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Annals of Emergency Medicine 45 (2005): 524-528.
- Trzeciak S, Dellinger RP, Chansky ME, Arnold RC, Schorr C, Milcarek B, Hollenberg SM, Parrillo JE. Serum lactate as a predictor of mortality in patients with infection. Intensive Care Med 33 (2007): 970-977.
- Mica L, Niggli C, Bak P, et al. Development of a Visual Analytics Tool for Polytrauma Patients: Proof of Concept for a New Assessment Tool Using a Multiple Layer Sankey Diagram in a Single-Center Database. World J Surg 44 (2020): 764-772.
- Mizock BA, Falk JL. Lactic acidosis in critical illness. Crit Care Med 20 (1992): 80-93.
- Qvisth V, Hagström-Toft E, Enoksson S, et al. Catecholamine regulation of local lactate production in vivo in skeletal muscle and adipose tissue: role of -adrenoreceptor subtypes. J Clin Endocrinol Metab 93 (2008): 240-246.
- Wardi G, Brice J, Correia M, et al. Demystifying Lactate in the Emergency Department. Ann Emerg Med 75 (2020): 287-298.
- Brealey D, Brand M, Hargreaves I, et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet 360 (2002): 219-223.
- Gibot S. On the origins of lactate during sepsis. Crit Care 16 (2012): 151.
- Wutzler S, Lustenberger T, Relja B, et al. Pathophysiologie des Polytraumas: Intensivmedizin und "Timing" der Versorgung [Pathophysiology of multiple trauma: intensive care medicine and timing of treatment]. Chirurg 84 (2013) 753-758.
- Levy MM, Fink MP, Marshall JC, et al. SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31 (2003): 1250-1256.
- Shankar-Hari M, Phillips GS, Levy ML, et al; Sepsis Definitions Task Force. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315 (2016): 775-787.
- del Portal DA, Shofer F, Mikkelsen ME, et al. Emergency department lactate is associated with mortality in older adults admitted with and without infections. Acad Emerg Med 17 (2010): 260-268.
- Song YH, Shin TG, Kang MJ, et al. Predicting factors associated with clinical deterioration of sepsis patients with intermediate levels of serum lactate. Shock 38 (2012): 249-254.
- Coats TJ, Smith JE, Lockey D, et al. Early increases in blood lactate following injury. J R Army Med Corps 148 (2002): 140-143.
- Cerovic O, Golubovic V, Spec-Marn A, et al. Relationship between injury severity and lactate levels in severely injured patients. Intensive Care Med 29 (2003): 1300-1305.
- Khosravani H, Shahpori R, Stelfox HT, et al. Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. Crit Care 13 (2009): R90.
- Mitra B, Roman C, Charters KE, et al. Lactate, bicarbonate and anion gap for evaluation of patients presenting with sepsis to the emergency department: A prospective cohort study. Emerg Med Australas 32 (2020): 20-24.
- Puskarich MA, Illich BM, Jones AE. Prognosis of emergency department patients with suspected infection and intermediate lactate levels: a systematic review. J Crit Care 29 (2014): 334-339.
- Shetty AL, Thompson K, Byth K, et al. Serum lactate cut-offs as a risk stratification tool for in-hospital adverse outcomes in emergency department patients screened for suspected sepsis. BMJ Open 8 (2018): e015492.
- Wilson M, Davis DP, Coimbra R. Diagnosis and monitoring of hemorrhagic shock during the initial resuscitation of multiple trauma patients: a review. J Emerg Med 24 (2003): 413-422.
- Abt R, Lustenberger T, Stover JF, et al. Base excess determined within one hour of admission predicts mortality in patients with severe pelvic fractures and severe hemorrhagic shock. Eur J Trauma Emerg Surg 35 (2009): 429-436.
- Zakrison T, McFarlan A, Wu YY, et al. Venous and arterial base deficits: do these agree in occult shock and in the elderly? A bland-Altman analysis. J Trauma Acute Care Surg 74 (2013): 936-939.
- Ibrahim I, Chor WP, Chue KM, et al. Is arterial base deficit still a useful prognostic marker in trauma? A systematic review. Am J Emerg Med 34 (2016): 626-635.
- Frantz TL, Gaski GE, Terry C, et al. The effect of pH versus base deficit on organ failure in trauma patients. J Surg Res 200 (2016): 260-265.
- Ross SW, Thomas BW, Christmas AB, et al. Returning from the acidotic abyss: mortality in trauma patients with a pH < 7.0. Am J Surg 214 (2017): 1067-1072.
- Copes WS, Champion HR, Sacco WJ, et al. The Injury Severity Score revisited. J Trauma 28 (1988): 69-77.
- American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20 (1992): 864-874.
- Schoeneberg C, Schmitz D, Schoeneberg S, et al. Gender-specific differences in therapy and laboratory parameters and validation of mortality predictors in severely injured patients--results of a German level 1 trauma center. Langenbecks Arch Surg 400 (2015): 781-790.
- Cannon CM, Miller RT, Grow KL, et al. Age-adjusted and Expanded Lactate Thresholds as Predictors of All-Cause Mortality in the Emergency Department. West J Emerg Med 21 (2020): 1249-1257.
- Johansson PI, Henriksen HH, Stensballe J, et al. Traumatic Endotheliopathy: A Prospective Observational Study of 424 Severely Injured Patients. Ann Surg 265 (2017): 597-603.
- Collins GS, Reitsma JB, Altman DG, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350 (2015): g7594.
- Weinberg DS, Narayanan AS, Moore TA, Vallier HA. Assessment of resuscitation as measured by markers of metabolic acidosis and features of injury. Bone Joint J 99-B (2017): 122-127.
- Jyoti D, Kumar A, Halim T, et al. The Association Between Serum Lactate Concentration, Base Deficit, and Mortality in Polytrauma Patients as a Prognostic Factor: An Observational Study. Cureus 14 (2022): e28200.
- Qi J, Bao L, Yang P, et al. Comparison of base excess, lactate and pH predicting 72-h mortality of multiple trauma. BMC Emerg Med 21 (2021): 80.
- Childs BR, Verhotz DR, Moore TA, et al. Presentation Coagulopathy and Persistent Acidosis Predict Complications in Orthopaedic Trauma Patients. J Orthop Trauma 31 (2017): 617-623.
- Bieler D, Paffrath T, Schmidt A, et al; Sektion NIS of the German Trauma Society. Why do some trauma patients die while others survive? A matched-pair analysis based on data from Trauma Register DGU®. Chin J Traumatol 23 (2020): 224-232.
- Huber-Lang M, Kovtun A, Ignatius A. The role of complement in trauma and fracture healing. Semin Immunol 25 (2013): 73-78.
- Denk S, Neher MD, Messerer DAC, et al. Complement C5a Functions as a Master Switch for the pH Balance in Neutrophils Exerting Fundamental Immunometabolic Effects. J Immunol 198 (2017): 4846-4854.
- Karasu E, Nilsson B, Köhl J, et al. Targeting Complement Pathways in Polytrauma- and Sepsis-Induced Multiple-Organ Dysfunction. Front Immunol 21 (2019): 543.
- Bone RC. Sir Isaac Newton, sepsis, SIRS, and CARS. Crit Care Med 24 (1996): 1125-1128.
- Sauaia A, Moore FA, Moore EE. Postinjury Inflammation and Organ Dysfunction. Crit Care Clin 33 (2017): 167-191.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 