Terrible Triad Injury or Complicated Triad Injury of Elbow: A Systematic Review
Weijun Guo1, Di Lu1, Jiqi Wang1, Peng Luo1, Miao Liu2*, Youming Zhao1*
1Department of Orthopedics, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou, China
2Department of Pathology, Brigham and Women’s Hospital, Harvard Medical School, Massachusetts, USA
*Corresponding Author: Miao Liu, Francis Street 75, Boston, Massachusetts, 02115, USA
Youming Zhao, Xueyuan West Road 109, Wenzhou, 325027, China
Received: 09 June 2020; Accepted: 22 June 2020; Published: 13 July 2020
Article Information
Citation:
Weijun Guo, Di Lu, Jiqi Wang, Peng Luo, Miao Liu, Youming Zhao. Terrible Triad Injury or Complicated Triad Injury of Elbow: A Systematic Review. Journal of Surgery and Research 3 (2020): 216-229.
View / Download Pdf Share at FacebookAbstract
Objectives: To summarize the changes of outcomes and complications of terrible triad injury (TTI) in patients who were treated by current surgical strategies. Our hypothesis was that with the application of current surgical protocols, clinical results were improved and complications reducing. However, risks still persisted and new challenges came to affect the prognosis.
Methods: We performed a systemic review of PubMed, MEDLINE, EMBASE, the Web of Science and Cochrane Library to identify all relevant studies. Studies of TTI patients treated based on current surgical protocols after 2004 were included. Outcomes evaluated were functional scores, the range of motion and complications.
Results: Eleven studies with 166 patients were included. With a mean follow-up of 14.8 to 41 months, average flexion arc was ranged from 99° to 127° with average forearm rotation of 80° to 156°. Mean Mayo Elbow Performance Score was 78 to 96. Mean Broberg- Morrey Score was 76 to 90. The most frequent complications were heterotopic ossification (0 to 31%) and posttraumatic osteoarthritis (0 to 38%), followed by nerve symptoms, dislocation or subluxation and stiffness.
Conclusions: Functional outcome after surgery for TTI indicates that current surgical protocols made TTI less terrible as it used to be. However, challenges still persisted and remained it a troublesome injury to treat. Clinicians should pay more attention to surgery unrelated factors and prosthesis-related complications to improve the outcomes.
Keywords
<p>Terrible triad; Elbow; Fracture- dislocations; Complications; Systematic review</p>
Article Details
1. Introduction
Elbow dislocation associated with both radial head and coronoid fractures, termed the “terrible triad injury” (TTI) by Hotchkiss [1], was notoriously challenging for decades because of the difficulties inherent in treatment and the consistently poor prognosis [2-4]. TTI was recorded as a severe injury with a lot of complications including recurrent instability, stiffness, arthritis, multiple reoperations, pain and functional limitations [4-6]. The aim of TTI treatment is to recover the stability of the elbow so as to allow early rehabilitation and reduce the risk of long-term joint stiffness or disability [7, 8]. Recently, with the improvement of elbow biomechanics and pathoanatomy knowledge, several systematic approaches for treatment were developed. In 2004, Pugh et al. proposed a standard surgical protocol to treat TTI [5], appeared to have yielded more favorable and reproducible clinical outcomes in recent studies [9-11]. Furthermore, a variety of modified surgical managements have been described for this injury [12-14]. Thus, most cases are treated surgically involving repair of the coronoid fracture and/or repair of the anterior capsule, fixation or replacement of the radial head, repair of the lateral
collateral ligament. Then, repair of medial collateral ligament and/or application of hinged external fixator in the event of residual instability after standard treatment [15, 16]. Such reports clearly reflected the outcomes and complications of TTI. We assumed that the application of current surgical protocols improved clinical results and reduced complications. Which made this injury no more as terrible as it used to be. On the other hand, additional challenges may persist and continue to affect the prognosis of TTI. As a consequence, we performed this systematic review to investigate the outcomes and complications in TTI patients treated by current surgical strategies after 2004.
2. Material and Methods
This systematic review was conducted following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement [17]. A literature search of PubMed, MEDLINE, EMBASE, the Web of Science and Cochrane Library was undertaken in November 2017 using combinations of the following search terms: coronoid fracture, radial fracture, elbow, fracture, dislocation, complex dislocation and terrible triad. Only English papers were included and duplicates were removed. Articles were considered for inclusion if they met the following criteria: patients were all adult who suffered TTI after 2004. The treatment was according to current surgical protocols, the outcomes and complications were described adequately using validated assessment. Studies were excluded if they were published in the form of case reports, review papers, comments, editorials, letters, publications on congress or manuscripts with incomplete documentation of outcomes and details of the applied treatment.
The titles and abstracts of the search results were independently screened by 3 reviewers (W. G, P. L and
- W). In case of disagreement, the consensus was
reached by discussion and by consulting a fourth reviewer (Y. Z) if necessary. Two reviewers (W. G and
- L) independently extracted data: Author details, publication year, demographics of patients including the amount, gender and age, delay in treatment, the period of follow-up. Data on functional outcomes (especially for range of motion and detail of functional scores) and complications were likewise recorded.
3. Results
3.1 Study selection and characteristics
A total of 3730 articles were identified in the initial search. After removal of duplicates, 2320 articles were screened by abstract and title. Of the 32 studies that were eligible for full-text assessment, 21 were excluded because of various reasons (Figure 1). The remaining 11 articles were included for systematic review. The characteristics of each included study are summarized in Table 1. All studies were retrospective in design. There was a total of 166 patients enrolled in 11 studies. Most of them were male with an average follow-up of 14.8 to 41 months, mean age ranged from 33.6 to 52 years. With a mean follow-up of 14.8 to 41 months.
3.2 Functional outcomes
The functional outcomes are detailed in Table 2 and 3. The average flexion arcs ranged from 99° to 127° while the mean forearm rotations were 80° to 156°. Most patients had functional motion (at least 30° to 130° of flexion-extension, 50° of pronation, and 50° of supination), which was estimated by 6 studies. Of 11 studies, 6 accomplished Mayo Elbow Performance Scores(MEPS), which ranged(mean) from 78 to 96. According to the Mayo Elbow Performance Index(MEPI), most patients were assessed as excellent or good while only less than 9% were fair to poor. With regard to Broberg-Morrey Scores, 4 studies reported that approximately 83% patients had excellent or good score. The mean score, in 3 of them, were 76 to 90.
3.3 Complications
Heterotopic ossification, arthritis, nerve symptoms, dislocation or subluxation and stiffness were the main classes of complications (Table 4). The most frequent ones were heterotopic ossification and posttraumatic osteoarthritis, which respectively ranged from 0 to 31% and 0 to 38%. Most of them were mild and asymptomatic in records. However, in the report of Giannicola, 5 of 8 heterotopic ossifications were class I, based on Hastings and Graham classification. While 2 were class IIIB and 1 was class IIIB- IIA [18]. In the study reported by Winter, 1 patient appeared heterotopic ossification with stiffness and nerve symptom but refused surgery [19]. As for the arthritis, 1 patient had grade II arthrosis in each report of Wang [20] and Hatta [12]. There was no grade III arthritis except for one in the research of Giannicola, which also reported 4 grade II and 5 grade I arthrosis.
Except for one study, the incidence of dislocation or subluxation seemed to be a little higher than recent studies (0-15% cf 2% [21, 22]) (Table 4). However, 7 of 11 cases were ascribed to surgical un-related factors by authors including limited compliance, obesity and secondary injury [18, 19, 23]. Inadequate compliance has also been a major factor for stiffness of elbows. Which led to 7 of 10 stiff elbows, reported by 4 studies [9, 18, 19, 24]. In addition, all but two nerve symptoms recovered in few months [14, 19]. With respect to prosthesis-related complications, Giannicola reported that resorption of the radial neck was observed in 13 of 16 patients with radial head replacement, while 1 had bipolar prosthesis disassembly and another elbow experienced prosthesis overstuffing and oversizing [18]. Leigh reported 2 resorptions of radial neck [9]. Winter
reported that 1 displayed a radial head disassembly and 1 a prosthesis overstuffing [19]. Other complications are summarized in Tables 4 and 5. A total of 20 cases required reoperations in 5 studies. Overall, additional
procedures were typically because of problems related to implants, stiffness, heterotopic ossification and nonunion (Table 5).
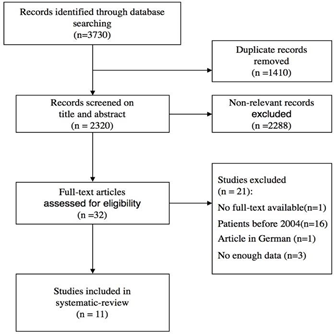
Figure 1: Flow Diagram of Study Selection.
|
Study |
Number of patients |
Gender (M/F) |
Age, years (range) |
Delay in treatment, days (range) |
Follow-up, months (range) |
|
Zhang [23] |
13 |
9/4 |
46.4 (35-79) |
12.6 (3-20) |
27.7 (12-NA) |
|
Hatta [12] |
14 |
10/4 |
46.5 (25-73) |
NA |
17 (12-36) |
|
Giannicola [18] |
26 |
13/13 |
52 (28-81) |
3 (2-6),40 |
31 (12-87) |
|
Chen [41] |
12 |
8/4 |
33.6 (22-55) |
4.6 (2-13) |
15.5 (12-27) |
|
Brigato [42] |
15 |
9/5 |
39 (NA) |
NA |
14.8 (NA) |
|
Zhang [14] |
21 |
17/4 |
38.4 (17-63) |
4 (2-8) |
32 (24-48) |
|
Papatheodorou [26] |
14 |
6/8 |
52 (32-58) |
3 (1-5) |
41 (24-56) |
|
Leigh [9] |
24 |
12/11 |
43.5 (19-67) |
<10 |
40.6 (16-73) |
|
Wang [20] |
8 |
6/2 |
39 (20-52) |
NA |
20 (11-35) |
|
Winter [19] |
13 |
9/4 |
40 (18-77) |
1.9 (1-4) |
25 (15-48) |
|
Pai [24] |
6 |
6/0 |
33.7 (26-54) |
NA |
2.2year (1-3) |
NA, not available
Table 1: Characteristics of the Included Studies.
MEPS-Mayo Elbow Performance Scores; DASH-Disabilities of the Arm, Shoulder and Hand; ASES-American Shoulder and Elbow Surgeons Score; HSS-Hospital for Special Surgery elbow assessment score; NA-not available; MCL-r: medial collateral ligament repaired; MCL-n: Medial collateral ligament non-repaired; E-excellent; G-good; F-fair; P- poor
Table 2: Functional Scores.
Functional motion, at least 30° to 130° of flexion-extension, 50° of pronation, and 50° of supination
Table 3: Range of Motion.
Instability, dislocation or subluxation
Table 4: Complications.
|
Study |
Other Complications |
Reoperations |
||
|
No. |
Details |
No. |
Details |
|
|
Zhang [23] |
3 |
2 coronoid nonunion, 1 radioulnar synostosis. |
- |
- |
|
Hatta [12] |
- |
- |
- |
- |
|
Giannicola [18] |
7 |
3 radioulnar synostosis, 1 radial head and 1 coronoid malunion, 2 K wires loosening and olecranon bursitis. |
6 |
4 arthrolysis because of stiffness, 2 removed the K wires |
|
Chen [41] |
- |
- |
- |
- |
|
Brigato [42] |
1 |
Infection. |
- |
- |
|
Zhang [14] |
2 |
1 radial head nonunion, 1 infection. |
1 |
debridement |
|
Papatheodorou [26] |
- |
- |
- |
- |
|
Leigh [9] |
4 |
2 radial head nonunion, 1 infection, 1 K wire migrated. |
6 |
2 replaced radial head due to nonunion, 1 removed the K wire, 1 repaired lateral collateral ligament, 2 released capsular. |
|
Wang [20] |
2 |
1 K wire broken, 1 experienced pain and extension deficit due to plate in olecranon |
2 |
1 removed broken K wire, 1 removed fixation plate in the olecranon. |
|
Winter [19] |
- |
- |
5 |
2 revised radial head prosthesis, 2 underwent arthrolysis, 1 closed reduction because of fall |
|
Pai [24] |
- |
- |
- |
- |
Table 5: Detail of Other Complications and Reoperations.
4. Discussion
This systematic review evaluated 11 retrospective studies, including 166 TTI patients treated after 2004, shows that most patients obtained excellent-good functional scores. Functional range of elbow motion (30° to 130° of flexion-extension, 50° of pronation, and 50° of supination), estimated by 6 studies, was observed in the majority of patients. The most common complications were arthritis and heterotopic ossification, followed by stiffness, instability and nerve symptoms.
In 1996, Hotchkiss first clearly described this complex type of fracture-dislocation. The incidence of repeated dislocation or subluxation persisted at a high level (4- 38%) [10, 18, 25-28]. Which made the ‘Terrible Triad Injury’ earn its eponym and resulted in arthrosis and stiffness [4]. Although dislocation or subluxation was once a scourge of the management for TTI, improved understandings of this injury and modern surgical protocols seemed to have turned it into an infrequent event [21]. We found that the risk of subluxation or dislocation related to the current surgical protocols was lower in the last decade (0-15%). Six studies included in our review did not report any patients had subluxation or dislocation after operations. Recently, there were only 2% recurrent dislocations and no subluxation reported by Zhang [21] when surgery was performed within 2 weeks of injury.
Furthermore, most patients had satisfactory outcomes with a functional range of elbow motions. With regards to MEPS and Broberg-Morrey scores, more than 85% patients had good or excellent scores. These findings support our assumption, indicate that current surgical protocols made TTI much less terrible than before. The term ‘terrible’ was very eye-catching and rarely seen in other medical terminology. It somewhat reflects both
patients and their doctors and may cause unnecessary anxieties and negative attitudes in the rehabilitation period. On the basis of the planned behavior theory, behavior is dominated by the attitudes and beliefs that a person has concerning the potential consequences of the behavior [29]. Incompliance may be caused by discouragement and leads to a poor prognosis. Moreover, the attitudes and beliefs about health and illness held by doctors are important for the approach they take in treatments [30]. Therefore, in order to induce positive behaviors, we endorse the recommendation of Xiao et al. [31] that ‘the complicated triad injury of the elbow’ may be more suitable for the clinic.
Whereas, challenges still persisted and continued to affect the prognosis of TTI. The highest complications recorded in our review were heterotopic ossification and arthritis. The incidence of heterotopic ossification oscillated between 0-38%. Which were comparable to other studies [18, 32]. Recently, Yang published a meta- analysis summarizing several significant risk factors for heterotopic ossification, i.e. male gender, combined radius/ulna fractures, overall fracture dislocation, ulnohumeral fracture dislocations, terrible triad, floating elbow and delay from injury to surgery [33]. Given the frequency and clinical impact of heterotopic ossification, prophylactic approaches have been advocated, such as NSAIDs and low-dose radiation therapy. Arthritis is also a well-documented complication of the elbow injury. According to the Broberg and Morrey classification for assessment of arthrosis, most elbows only had grade 0 to 1 changes in our review. All of them were asymptomatic. Wysocki indicated that the main cause of post-traumatic arthritis is the initial injury, especially due to intra-articular fracture or malunion of fracture [34]. Severe post- traumatic osteoarthritis often leads to pain, heterotopic
ossification and loss of motion and function [35]. Hence, long-term follow-ups are needed to clarify whether advanced grades will occur.
Interestingly, with the knowledge of elbow biomechanics and new excogitation of implant has improved, more and more clinicians applied replacements to treat comminuted radial head fractures [36, 37]. Meanwhile, complications including resorption of the radial neck, loosening or overstuffing of the implants increased. The radial head plays a key role as a stabilizer against owing to the medial collateral ligaments is usually torn. Lengthening or shortening of the prosthesis will alter the pressure and kinematics of humeroradial joint, which can cause stiffness, pain or varus-valgus laxity of elbow [38]. Therefore, the learning curve should be noted to avoid oversizing and overstuffing the radial head prosthesis [39]. Radial head resorption was attributed to the stress shielding around the prostheses [40]. Recently, this has been reported as a common phenomenon and does not appear to affect the prognosis [11]. However, long-term researches are welcomed to illustrate the causes and the clinical significance of it. Moreover, surgery un-related factors like inadequate compliance, secondary injury and obesity constantly represented negative factors for prognosis. In our systematic review, limited or none compliance reported by 3 articles, resulted in 7 of 10 elbow stiffness and 3 of 11 subluxations [18, 19, 23]. Two dislocations being due to another fall happened after surgery [18, 19]. And Giannicola attributed another two subluxations to the obesity of patients [18]. Anyway, all these complications and new challenges require more attention of clinicians.
Our systematic review has some limitations. Firstly, the strength of evidence is not of the highest quality due to all studies were retrospective. Secondly, the overall
number of patients was only 166, with average follow- up of 14.8-41 months. Several complications needed more time to observe their impact on the quality of life. Finally, because terrible triad injuries of the elbow were not sufficiently common, data of interest were not enough for analyzing separately according to the different type of fractures or soft tissue injuries. Which might affect both functional outcomes and complications. Therefore, long-term prospective articles with large sample would be welcome to validate our results.
5. Conclusion
This systematic review indicated that current surgical protocols made TTI less terrible as it used to be. However, challenges still persisted and remained it a troublesome injury to treat. Due to the surgery un- related factors like limited compliance, secondary injury and obesity constantly affecting prognosis, further refinements in postoperative management are required to improve outcomes. Besides, more attention needs to be paid to reducing prosthesis-related complications.
Compliance with Ethical Standards
Conflicts of Interest and Source of Funding: Each author, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Funding
This study was supported by Wenzhou Science and Technology Bureau Project (Y20190270).
References
- Hotchkiss R. Rockwood and Green’s fractures in adults. Philadelphia: Lippincott-Raven (1996).
- Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71 (1989): 1348-1354.
- Terada N, Yamada H, Seki T, et al. The importance of reducing small fractures of the coronoid process in the treatment of unstable elbow dislocation. J Shoulder Elbow Surg 9 (2000): 344-346.
- Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am 84-a (2002): 547-551.
- Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 86-a (2004): 1122-1130.
- Egol KA, Immerman I, Paksima N, et al. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis 65 (2007): 263-270.
- Pipicelli JG, Chinchalkar SJ, Grewal R, et al. Rehabilitation considerations in the management of terrible triad injury to the elbow. Tech Hand Up Extrem Surg 15 (2011): 198-208.
- Dodds SD, Fishler T. Terrible triad of the elbow. Orthop Clin North Am 44 (2013): 47- 58.
- Leigh WB, Ball CM. Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elbow Surg 21 (2012): 1336-1341.
- Chemama B, Bonnevialle N, Peter O, et Terrible triad injury of the elbow: how to improve outcomes? Orthop Traumatol Surg Res 96 (2010): 147-154.
- Lindenhovius AL, Jupiter JB, Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am 33 (2008): 920-926.
- Hatta T, Nobuta S, Aizawa T, et al. Comparative analysis of surgical options for medial collateral ligament repair in terrible triad injury of the elbow. Orthop Rev (Pavia) 8 (2016): 89-93.
- Pierrart J, Begue T, Mansat P. Terrible triad of the elbow: treatment protocol and outcome in a series of eighteen cases. Injury 46 (2015): 8-12.
- Zhang C, Zhong B, Luo CF. Treatment strategy of terrible triad of the elbow: experience in Shanghai 6th People's Hospital. Injury 45 (2014): 942-948.
- Fitzgibbons PG, Louie D, Dyer GS, et al. Functional outcomes after fixation of "terrible triad" elbow fracture dislocations. Orthopedics 37 (2014): 373-376.
- Rodriguez-Martin J, Pretell-Mazzini J, Andres- Esteban EM, et al. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. [Review]. Int Orthop 35 (2011): 851-860.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj 339 (2009):
- Giannicola G, Calella P, Piccioli A, et al. Terrible triad of the elbow: is it still a troublesome injury? Injury 46 (2015): 68-76.
- Winter M, Chuinard C, Cikes A, et al. Surgical management of elbow dislocation associated with non-reparable fractures of the radial head. Chir Main 28 (2009): 158-167.
- Wang YX, Huang LX, Ma SH. Surgical treatment of "terrible triad of the elbow": technique and outcome. Orthop Surg 2 (2010): 141-148.
- Zhang D, Tarabochia M, Janssen S, et al. Risk of Subluxation or Dislocation After Operative Treatment of Terrible Triad Injuries. J Orthop Trauma 30 (2016): 660-663.
- Gupta A, Barei D, Khwaja A, et al. Single- staged treatment using a standardized protocol results in functional motion in the majority of patients with a terrible triad elbow injury. Clin Orthop Relat Res 472 (2014): 2075-2083.
- Zhang JR, Tan M, Kwek EBK. Outcomes of coronoid-first repair in terrible triad injuries of the elbow. Arch Orthop Trauma Surg 137 (2017): 1239-1245.
- Pai V, Pai V. Use of suture anchors for coronoid fractures in the terrible triad of the elbow. J Orthop Surg (Hong Kong) 17 (2009): 31-35.
- Garrigues GE, Wray WH, Lindenhovius AL, et al. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg Am 93 (2011): 1873-1881.
- Papatheodorou LK, Rubright JH, Heim KA, et al. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res 472 (2014): 2084-2091.
- Toros T, Ozaksar K, Sugun TS, et al. The effect of medial side repair in terrible triad injury of the elbow. Acta Orthop Traumatol Turc 46 (2012): 96-101.
- Watters TS, Garrigues GE, Ring D, et al. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res 472 (2014): 2128-2135.
- Ajzen I. Nature and operation of attitudes. Annu Rev Psychol 52 (2001): 27-58.
- Gardner T, Refshauge K, Smith L, et al. Physiotherapists' beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother 63 (2017): 132-143.
- Xiao K, Zhang J, Li T, et al. Anatomy, definition, and treatment of the "terrible triad of the elbow" and contemplation of the rationality of this designation. Orthop Surg 7 (2015): 13-18.
- Hong CC, Nashi N, Hey HW, et al. Clinically relevant heterotopic ossification after elbow fracture surgery: a risk factors study. Orthop Traumatol Surg Res 101 (2015): 209-213.
- Yang YJ, Zhao X, Dong TH, et al. A meta- analysis of risk factors for heterotopic ossification after elbow trauma. Int J Clin Exp Med 9 (2016): 5308-5317.
- Douglas K, Cannada LK, Archer KR, et al. Incidence and risk factors of heterotopic ossification following major elbow trauma. Orthopedics 35 (2012): 815-822.
- Kim SJ, Kim JW, Lee SH, et al. Retrospective Comparative Analysis of Elbow Arthroscopy Used to Treat Primary Osteoarthritis With and Without Release of the Posterior Band of the Medial Collateral Ligament. Arthroscopy 33 (2017): 1506-1511.
- Chen X, Wang SC, Cao LH, et al. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop 35(2011): 1071- 1076.
- Grewal R, MacDermid JC, Faber KJ, et al. Comminuted radial head fractures treated with a modular metallic radial head Study of outcomes. J Bone Joint Surg Am 88 (2006): 2192-2200.
- Van Glabbeek F, Van Riet RP, Baumfeld JA, et al. Detrimental effects of overstuffing or understuffing with a radial head replacement in the medial collateral-ligament deficient elbow. J Bone Joint Surg Am 86-a (2004): 2629-2635.
- Yan M, Ni J, Song D, et al. Radial head replacement or repair for the terrible triad of the elbow: which procedure is better? ANZ J Surg 85 (2015): 644-648.
- Chanlalit C, Shukla DR, Fitzsimmons JS, et al. Stress shielding around radial head prostheses. J Hand Surg Am 37 (2012): 2118-2125.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 