The Learning Curve for Laparoscopic Totally Extraperitoneal Herniorrhaphy by Logarithmic Function: Consecutive 291 cases Performed by a Single Surgeon
DuYeong Hwang, YongHae Baik*
Department of Surgery, Dongguk University Ilsan Hospital, Goyang, Korea
*Corresponding Author: YongHae Baik, Department of Surgery, Dongguk University Ilsan Hospital, Siksa-dong, Ilsandong-gu, Goyang 10326, Korea
Received: 02 May 2023; Accepted: 09 May 2022; Published: 30 May 2023
Article Information
Citation: DuYeong Hwang, YongHae Baik. The Learning Curve for Laparoscopic Totally Extraperitoneal Herniorrhaphy by Logarithmic Function: Consecutive 291 cases Performed by a Single Surgeon. Journal of Surgery and Research. 6 (2023): 221-226
View / Download Pdf Share at FacebookAbstract
Purpose: The Totally extraperitoneal (TEP) herniorrhaphy is not an easy technique for beginner surgeons because of the complexity of inguinal anatomy and narrow space of the operation field. The aim of this study is to estimate learning curve of laparoscopic TEP herniorrhaphy using logarithmic function model and the exponential function model. Revealing the number of cases needs to overcoming the early learning curve and minimizing the recurrence rate.
Methods: A retrospective analysis of the first 291 patient who underwent laparoscopic TEP herniorrhaphy by a single surgeon consecutively. A logarithmic function and an exponential function were derived from operating time data. The population was divided into three consecutive groups. Each groups assigned the starting point, the slope of the curve, and the plateau of the curve. We calculated how many operation numbers are needed to achieve reduction expected operating time to mean operating time.
Results: 291 patients underwent laparoscopic hernia repair. The mean operation time was 70.3 minutes for unilateral hernias. According to two learning curve models, the operation time was decreased less than mean operation time after the initial 88 cases was performed. As the operation time decreased, the recurrence rate decreased.
Conclusion: According to the two learning curve models, 88 cases are required to overcome the learning curve, minimize revision surgery, and achieve a qualified surgery. Further studies on learning curves and training methods are needed to enable a scientific approach to surgical education and quality improvement in surgical education for surgeons and medical services for patients.
Keywords
<p>Herniorrhaphy, Learning curve, Logarithmic Function model</p>
Article Details
Introduction
Herniorrhaphy is one of the most frequently performed operations in general surgery and many other techniques have been invented. There were two landmark revolutionary events in the history of hernia surgery. The first one was the introduction of the Lichtenstein tension-free technique [1] and the second one was the introduction of the laparoscopic approach to hernia surgery [2]. These technical revolutions provide for low postoperative pain, a low recurrence rate, and an early return to normal activity. There are two kinds of laparoscopic approaches. Transabdominal preperitoneal (TAPP) herniorrhaphy was invented prior to TEP in the 1990s. Since then, the TAPP approach gained popularity and soon became the standard for laparoscopic hernia repair. Many studies have shown that this technique had low recurrence rates of less than 1%. However, this technique requires entry into the abdominal cavity and accesses the posterior floor of the groin, so it is related to many complications such as internal hernias from the inappropriate closure of the peritoneum and injury to the viscera from trocars and needles [3]. The totally extraperitoneal (TEP) herniorrhaphy was introduced in 1992 by Dulucq [2]. Since this technique does not require entry into the abdominal cavity and is free from complications related to entering the abdominal cavity, it has gained popularity in the recent two decades [4]. This technique also has many strong points. It has recurrence rates equivalent to those of the open technique with less neural pain, lower hematoma occurrence, lower infection rates, and a shorter recovery period [5-7]. When TEP was compared to TAPP, TEP had a shorter operation time and lower possibility of damaging adjacent organs [8-10]. In this article, only TEP herniorrhaphy will be addressed. Although the postoperative complication rates are higher in the TAPP approach, most of the complications could be handled with conservative management. And the reoperation rates were similar in both approaches [11]. The newest opinion is that both approaches are acceptable, and although the postoperative complication rates are higher in the TAPP approach, most of the complications could be handled with conservative management so only in certain circumstances is one laparoscopic technique preferred to the other. In cases of an incarcerated hernia, for example, the TAPP approach is usually preferred because this approach permits a more accurate analysis of the contents of the hernia sac and viability, as well as providing for the safe reduction of the hernia contents [3]. Despite the many advantages of TEP hernia repair, the relatively long learning curve needed to acquire sufficient skill in the laparoscopic approach is an important challenge(12). The laparoscopic approach is not an easy technique for beginning surgeons because of the complexity of the inguinal anatomy and the narrow space of the operative field [13]. Overcoming the early learning curve is important because it is during that time that poorer clinical outcomes occur. However, the nature of the learning curve and the exact learning model or the number of procedures required to overcome the early learning curve are unclear [4]. According to previous studies, the learning curve status could be assessed by operating time, postoperative complications, and technical difficulties [14,15]. In this study, only the operating time was used as a parameter because it is a very objective parameter, easy to measure, and easy to utilize to produce mathematical models. The aim of this study was to estimate the learning curve of laparoscopic TEP herniorrhaphy using a logarithmic function model and minimize the reoperation rate, and achieve qualified surgery. Revealing the number of cases needed to overcome the early learning curve may help trainees and trainers.
Methods
We performed a retrospective review of all patients who underwent laparoscopic TEP herniorrhaphy by a single surgeon consecutively at a single center from September 2008 to January 2020. This study includes the operator's first TEP herniorrhaphy case. Although this surgeon has 15 years of experience in upper gastrointestinal surgery, he has no experience in laparoscopic hernia surgery other than an open hernia. Prior to initiating TEP herniorrhaphy surgery, operators participated in animal surgery experiments and live surgery lectures. The clinical features, operating time, operative findings, and outcomes were reviewed in the medical records. To investigate the recurrence and reoperation rate, the patients were followed up by telephone or physical examination.
A total of 291 patients underwent laparoscopic TEP herniorrhaphy. Every operation was a scheduled operation. Patients with an inguinal hernia who underwent another surgical procedure at the same time were excluded. Finally, 257 patients were analyzed. We calculated how many surgeries were needed to achieve a reduction in the expected operating time to mean operating time ratio. A logarithmic function and an exponential function were derived from the operating time data by univariate cox regression analysis and graphs were generated. The number of surgeries was plotted along the X-axis and the operating time was plotted along the Y-axis (Figures 1 and 2). Then, we calculated how many surgeries were needed to achieve a reduction in the expected operating time to mean operating time ratio (Figures 1 and 2). Statistical analysis was performed using SPSS version 23.0.
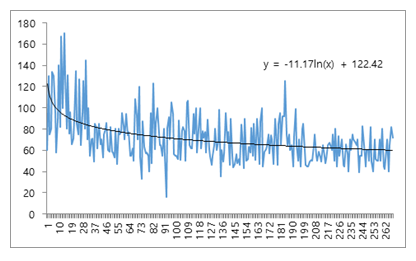
Figure 1: The logarithmic model and formula. *70 is the mean operation time (minutes).
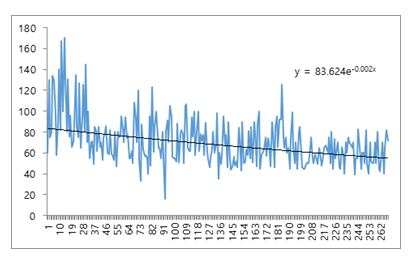
Figure 2: The exponential model and formula. *70 is the mean operation time (minutes).
Surgical technique
The patients were asked to empty their bladder before surgery. Under general anesthesia, all patients were placed in the supine position. The operator and the first assistant stood at the opposite side of the lesion. The main role of the first assistant was as the scopist. One 10-mm trocar and two 5-mm trocars were used. The 10-mm trocar was placed through the supraumbilical incision and one 5-mm trocar was placed at the suprapubic area and the other 5-mm trocar was placed between the two of them. A 10-mm balloon trocar was proceeded along the anterior side of the posterior rectus sheath beyond the arcuate line. After inflating the balloon catheter, Cooper’s ligament, the inferior epigastric vessel, and the hernia sac could be identified. the case of an indirect inguinal hernia, a hernia sac presents at the lateral side of the inferior epigastric vessel. Dissection of the medial side precedes dissection of the lateral side. Dissection of the lateral side starts from the lateral side of the inferior epigastric vessel and attempts to secure the pre-peritoneal space. The next step was the dissection of the spermatic cord and should be done carefully because, in an indirect hernia, the hernia sac is encapsulated with the spermatic cord. In the case of a direct hernia, the hernia sac usually is separated and reduced by inflation of the balloon trocar. In this case, the pseudo sac was fixed to Cooper’s ligament to distinguish it from relapse after surgery. After reducing the hernia sac, an artificial mesh (Parietex, 15x10 cm, Sofradium) was inserted between the abdominal wall and the peritoneum. The most important thing in this procedure is peritonization of the hernia sac and parietalization of the spermatic cord. The medial margin of the mesh was fixed on Cooper’s ligament with a tack. After thrombin spraying and deflation with the observation that the inserted mesh was in the proper position, the operation was completed.
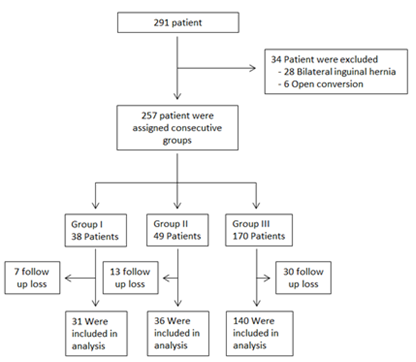
Figure 3: Flow diagram of study
Results
Between September 2008 and Jan 2020, 291 patients underwent laparoscopic hernia repair in our institute by a single surgeon. Among these, 34 patients were excluded because they met the exclusion criteria and 257 patients were finally included in the study. The study group included 268 male and 23 female patients. The mean age of the patients was 55.1 years. There were 166 cases of right-sided hernia and 99 cases of left-sided hernia. The mean length of the hospital stay was 2.35 days (range, 1 to 23 days) (Table 1). Four patients stayed in the hospital for an exceptionally long time. Two patients stayed 8 days, and one patient stayed 23 days. One 8-day stay patient just wanted a longer hospital stay. The other 8-day stay patient requested treatment from another department (dermatology for warts). The 23-day stay patient was treated for an incidentally found hepatocellular carcinoma after TEP herniorrhaphy. There were no specific complications related to TEP herniorrhaphy that needed reoperation or a longer hospital stay. Eighty percent of all patients had follow-up by telephone or physical examination, but 20% did not (Table 2). The recurrence and reoperation rate was 2.33%. The recurrence rate decreased according to consecutive groups. The follow-up period was 12-144 months. Two learning curve models were used, the logarithmic function model and the exponential function model described in figures 1 and 2. The mean operation time was 70 minutes. After the initial 87 cases were performed, according to the logarithmic function model, the operation time decreased to lower than the mean time, whereas in the exponential function model, 88 cases were needed. According to our previous research and this data, the population was divided into three consecutive groups. Each groups assigned the starting point, the slope of the curve, and the plateau of the curve. The end point of the starting point was set to 38 cases and the endpoint of the slope of the curve was set to 87 cases. According to the two endpoints, the patients were divided into three consecutive groups. The clinical features and follow-up results in each group were analyzed (Table 2). The average operation time and hospital stay decreased over time in the three consecutive groups. As the operation time decreased, the rate of recurrence and reoperation decreased.
|
Variable |
No. |
|
Patients no. |
291 |
|
Age (years), Mean ± SD |
55.1 ± 14.9 |
|
Sex, no. |
|
|
Male |
268 |
|
Female |
23 |
|
Site of hernia |
|
|
Right inguinal |
166 |
|
Left inguinal |
99 |
|
Bilateral inguinal |
26 |
|
Hospital stay (days), Mean |
2.35 |
Table 1: Clinical features
|
Group |
|||
|
Variable |
I |
II |
III |
|
Patients no. |
38 |
49 |
170 |
|
Mean age, yr |
53.13 ± 13.20 |
52.14 ± 14.14 |
56.17 ± 15.77 |
|
Gender, male:female ratio |
34.4 |
48:01:00 |
154:16:00 |
|
Hernia laterally, right:left ratio |
24:14:00 |
29:20:00 |
109:61 |
|
Mean operation time, minutes |
96.92 ± 32.03 |
71.63+19.19 |
56.17 ± 15.77 |
|
Hospital stay, days |
3.42 ± 2.29 |
2.87±3.19 |
1.97 ± 0.32 |
|
After follow up |
|||
|
Follow up rate, no (%) |
31 (81%) |
36 (73%) |
140 (82%) |
|
Follow up period, months |
120-144 |
98-118 |
12-98 |
|
Recurrence rate, no. (%) |
2 (6.45%) |
2 (5.55%) |
2 (1.42%) |
|
Average recurrence periods, yr |
8.5 |
4.5 |
2.5 |
|
Reoperation rate. no. (%) |
2 (6.45%) |
2 (5.55%) |
2 (1.42%) |
Table 2: Clinical features and follow-up results in three consecutive groups
Discussion
Inguinal hernia is one of the most common conditions in general surgery and more than 700,000 cases of inguinal herniorrhaphy are performed in the United States and more than 33,000 cases are performed in Korea [2,16]. As inguinal hernias are common, herniorrhaphy has an extensive history and techniques have advanced continuously from premodern techniques to the current laparoscopic tension-free techniques. The patient’s burden has been lightened by these advances. However, laparoscopic herniorrhaphy is not an easy technique for surgeons, especially for beginners, because of the complexity of the anatomy and the narrow operative field. Every surgeon has early unskilled periods. Overcoming the early learning curve is important because this early unskilled period is associated with high complication and recurrence rates [15]. The learning curve is a function that describes the improvement in results from continued practice. The learning curve is composed of 3 components, the starting point, the slope of the curve, and the plateau of the curve [17]. The slope of the curve is a steep section from the starting point to the plateau. After the slope of the curve, a practitioner becomes stable and produces better results than previously. In this study, we assumed that the shape of the learning curve followed a logarithmic or exponential function. The logarithmic regression model shows the shape mentioned in the former sentence, but the exponential model shows a linear shape. Revealing the shape of the learning curve and the number of cases needed to overcome the slope will help in developing a training course. For example, according to Liem MS et al. [15], the beginner surgeon who had little backup from an experienced surgeon had more early recurrences. The approximate number of cases to overcome the early slope of the learning curve will help to determine how long the supervision by an experienced surgeon is needed and when complication rates will decrease during the early learning phase. The logarithmic model and the exponential model showed that the number of cases need to overcome the learning curve was 87.9 and 88.9, respectively. Many studies on the learning curve of TEP herniorrhaphy have demonstrated various methods and different results. Jong Won Lim et al. [14] used the moving average method to deduce the learning curve and divided the learning period and experienced period at 30 cases. Another study reported that 60 cases were necessary [18]. However, there is no detailed description of how to calculate that value. The European Hernia Society 2009 Guidelines suggest that 50 to 100 cases are necessary, with the first 30 to 50 being critical [19]. A formal training course, close intra-operative supervision, and assistance provided to the surgeon by other well-trained staff may shorten the learning curve [20]. Appropriate patient selection is an important parameter for successful surgery during the early learning period [4,21]. In the early period, TEP hernia repair may prudently avoid patients with irreducible hernias and those with previous lower quadrant surgery. The strength of the study was the application of mathematical models. The application of mathematical models enables an objective derivation of the number of cases needed to gain adequate expertise. Our previous studies confirmed that the initial learning curve required 35 to 37 cases to minimize complications and operation time [22]. In this study, at least 87-88 cases were needed to overcome the TEP hernia learning curve, minimize the reoperation rate, and achieve qualified surgery. Studies have suggested several ways to reduce the number of cases needed to overcome the learning curve. Clarification of the learning curve and the learning process of a surgeon would help in the development of training courses. And effective training courses are important not only to surgeons but also to patients who undergo surgery performed by a surgeon in the early learning curve. Further studies on learning curves and training methods are needed to enable a scientific approach to surgical education and quality improvement in surgical education for surgeons and medical services for patients.
Limitations
As a limitation of this retrospective study, follow-up for recurrence and reoperation rate was not investigated during the same period. If there are no special abnormalities, outpatients do not visit again after 1st visit after surgery. Therefore, the recurrence and reoperation rate were confirmed at the beginning of the study. Also, there was no significant difference between recurrence and reoperation rate in each group, and it was difficult to use as an index to evaluate safety and efficacy. Therefore, surgery time was used as a new evaluation index using logarithmic and exponential functions.
Acknowledgements
Not applicable.
Authors’ contributions
Study conception and design: DH and YB. Acquisition of data: DH. Analysis and interpretation of data: DH and YH. Drafting of manuscript: DH. Critical revision of manuscript and editing: DH and YB.
Funding
This study was supported by the Dongguk University Research fund of 2016
Availability of data and materials
The datasets of the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
All the procedures were implemented based on the principles of the Declaration of Helsinki, and the design of the work was reviewed and approved by the Ethics Committee of Dongguk university hospital. A This study was conducted using retrospective data obtained for clinical purposes. This study does not include studies with human participants conducted by the authors. the need for patient consent was exempted by our institutional ethic committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty. The American Journal of Surgery 157 (1989): 188-193.
- Dulucq JL, Wintringer P, Mahajna A. Laparoscopic totally extraperitoneal inguinal hernia repair: lessons learned from 3,100 hernia repairs over 15 years. Surg Endosc 23 (2009): 482-486.
- EL F. Laparoscopic inguinal hernia repair. LL S, NJ S, M L, editors: Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health (2014) pp: 574-588.
- Hasbahceci M, Basak F, Acar A, et al. A New Proposal for Learning Curve of TEP Inguinal Hernia Repair: Ability to Complete Operation Endoscopically as a First Phase of Learning Curve. Minim Invasive Surg (2014): 528517.
- Taylor CJ, Wilson TJAjos. Long-term results of laparoscopic totally extraperitoneal inguinal herniorrhaphy 75 (2005): 637-639.
- Thill V, Simoens C, Smets D, et al. Long-term results of a non-ramdomized prospective mono-centre study of 1000 laparoscopic totally extraperitoneal hernia repairs 108 (2008): 405-408.
- Myers E, Browne KM, Kavanagh DO, et al. Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes 34 (2010): 3059-3064.
- Eklund AS, Montgomery AK, Rasmussen IC, et al. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg 249 (2009): 33-38.
- Liem MS, Van der Graaf Y, Van Steensel CJ, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med 336 (1997): 1541-1547.
- Felix E, Harbertson N, Vartanian SJSe. Laparoscopic hernioplasty 13 (1999): 328-331.
- Kockerling F, Bittner R, Jacob DA, et al. TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc 29 (2015): 3750-3760.
- Schouten N, Simmermacher R, Van Dalen T, et al. Is there an end of the “learning curve” of endoscopic totally extraperitoneal (TEP) hernia repair? 27 (2013): 789-794.
- Lange J, Rooijens P, Koppert S, et al. The preperitoneal tissue dilemma in totally extraperitoneal (TEP) laparoscopic hernia repair 16 (2002): 927-930.
- Lim JW, Lee JY, Lee SE, et al. The learning curve for laparoscopic totally extraperitoneal herniorrhaphy by moving average. J Korean Surg Soc 83 (2012): 92-96.
- Liem MS, Van Steensel CJ, Boelhouwer RU, et al. The learning curve for totally extraperitoneal laparoscopic inguinal hernia repair. Am J Surg 171 (1996): 281-285.
- National Health Insurance Corporation. Top 20 Frequent Diseases by Operation [Internet]. Daejeon: National Health Insurance Corporation (2019)
- Harrysson IJ, Cook J, Sirimanna P, et al. Systematic review of learning curves for minimally invasive abdominal surgery: a review of the methodology of data collection, depiction of outcomes, and statistical analysis. Ann Surg 260 (2014): 37-45.
- Choi YY, Kim Z, Hur KY. Learning curve for laparoscopic totally extraperitoneal repair of inguinal hernia. Can J Surg 55 (2012): 33-36.
- Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 13 (2009): 343-403.
- Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol 11 (2005): 7508-7511.
- Schouten N, Elshof J, Simmermacher R, et al. Selecting patients during the “learning curve” of endoscopic Totally Extraperitoneal (TEP) hernia repair 17 (2013): 737-743.
- Kwon OC, Baik YH, Oh MG, et al. The Learning Curve for Laparoscopic Totally Extraperitoneal Herniorrhaphy by Logarithmic Function. The Journal of Minimally Invasive Surgery 19 (2016): 126-129.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 