Learning Curve of Surgical Trainees Performing Laparoscopic Appendectomy and Effect on Patient outcome - A Register based Study
Nathalie Young*, Lennart Boström, Gabriel Sandblom, Hans Järnbert Pettersson
Department of Clinical Science and Education Södersjukhuset, Karolinska Institute, Stockholm, Sweden
*Corresponding Author: Nathalie Young. Department of Clinical Science and Education Södersjukhuset, Karolinska Institute, Stockholm, Sweden
Received: 22 August 2022; Accepted: 26 August 2022; Published: 08 November 2023
Article Information
Citation: Nathalie Young, Lennart Boström, Gabriel Sandblom, Hans Järnbert Pettersson. Learning Curve of Surgical Trainees Performing Laparoscopic Appendectomy and Effect on Patient outcome - A Register based Study. Journal of Surgery and Research. 6 (2023): 364-370.
View / Download Pdf Share at FacebookAbstract
Background: The purpose of this study was to analyse the learning curve of a cohort of surgical trainees, to investigate if there were any impact on complication rate and potential factors influencing the learning process.
Method: The study was based on a patient cohort extracted from the local appendectomy register at Södersjukhuset, Stockholm. The register includes patient characteristics, surgical method, operation time, and 30- day complications. First-year surgical trainees attending the hospital’s trainee programme were included and followed over five years of training. Trainees who had performed less than ten procedures during the period of the study were excluded. The learning curve was described using moving average of order ten for each trainee, studying the trend in operation time with increasing volume. The cumulative sum technique was used to chart changes in complication rates of the trainees. Multivariate analysis for investigating potential factors of influence.
Results: In total 586 procedures performed by 9 surgical trainees were included, of which 97.6% were performed laparoscopically. A plateau in operation time on the learning curve was reached at 60 procedures. For three of the trainees, the 30-day complication rate decreased after completing the learning curve, whereas for two others it increased. In a multivariate analysis, operation times differed more between the trainees than it did between procedures performed early or late in the programme. Shortest versus longest mean operation time (41 min versus 89 min).
Conclusion: At least 60 procedures are required to reach sufficient proficiency in laparoscopic appendectomy and a significantly higher complication rate during the early learning curve. This highlights the importance of meticulous selection of surgical trainees, structure of training programmes, feedback and assessment.
Keywords
<p>Operation time, Surgical trainee volume, Laparoscopic appendectomy, Appendectomy, Proficiency, Patient outcomes, Complication rate, Surgical training, Surgical education, Skills training</p>
Article Details
Background
Laparoscopic appendectomy is traditionally the first abdominal procedure that surgical trainees are expected to accomplish early on in their journey to becoming an independent surgeon. To guarantee patient safety, it is important to identify the surgical volume required to reach skills high enough to perform an appendectomy, and to gain better understanding of factors that influence the learning process. The surgical procedure itself involves a limited number of technical skills (accessing the abdomen, dissection of the meso-appendix, removal of the appendix and exiting the abdomen) compared to other abdominal procedures. Therefore, appendectomy is often considered as a basic and straight forward procedure. On the other hand, acute appendicitis is one of the most common causes of acute lower abdominal pain among patients attending the emergency department. The overall lifetime risk for appendicitis is around 7% with almost no difference between the sexes. Since the middle of the 19th century, the primary method of treatment has been surgical removal of the appendix. The recommended first line treatment is still surgery, though nowadays this is usually carried out laparoscopically [1,2]. For this reason, it is important to investigate if our Swedish way of teaching surgical trainees in the operating theatre are safe and efficient enough. Starting off by defining the learning curve for laparoscopic appendectomy in the Swedish setting may reveal areas in the surgical training system that need improvement. Practicing in a simulation-based environment has been shown to be helpful to facilitate learning curves. Nevertheless, there will always be a gap between virtual reality-based training and the operating theatre. A number of previous studies [3-7] have been conducted on smaller cohorts of patients and surgeons under training, showing that operation times decrease, reaching a plateau after around 20-30 [8-10]. A recent study on a larger cohort of 1173 patients undergoing laparoscopic appendectomy showed that there was no significant difference between surgical trainees and senior colleagues regarding operation time, length of stay, and complications [11]. Operation time in this context is often used as a surrogate to define learning curve, indicating the end of the learning curve when a plateau or a steady state in operation time is reached. The surgical training programme utilizes the same apprenticeship model for teaching surgical skills in the operating theatre as most other countries. However, the trainees are left alone in the operation theatre rather early on in their training, entrusted to have the judgement of calling for help when needed. Another tradition in Sweden is that the junior trainees need to be able to do most appendectomies independently before starting on-call out-of-hours work. There is no final examination before completing general surgery training in Sweden, and no nationally adopted department-based tool for assessing technical skill. Hence, no Swedish data for describing surgical volume and effect on patient outcome or factors potentially influencing the learning process. In order to contribute to this knowledge gap with this register-based study aimed to define the learning curve for laparoscopic appendectomy in a group of Swedish general surgery trainees, assess any relationship between surgeon volume and clinical outcome of appendicitis and potential factors influencing the learning process.
Methods
The cohort of general surgical trainees evaluated were selected from the register by identifying those who carried out their first appendectomies as primary surgeon during the first six months of the study period 1-12-2015 to 31-12-2020. We chose to exclude the procedures, where the trainees were assisting surgeon since it is impossible from the register to define who did most of the procedure. Surgical trainees, who had carried out less than 10 procedures during the study period were also excluded since we could not follow their learning for a sufficient period. These trainees were from other surgical specialties on a shorter rotation at the general surgical department or general surgical trainees transferring to another hospital. During the first six months of the study period there were nine first-year general surgery trainees employed at the surgical department of Södersjukhuset. These trainees had about the same pre-surgical knowledge and skills. In Stockholm region most surgical trainees have done about six months of rotation at a surgical department before applying for a surgical trainee position. None of the nine trainees included had gone through a simulation-based or wetlab course prior to acceptance at their trainee position. The cohort of surgical trainees were followed during their five-year residency period. The accumulated number of procedures carried out by the trainee was defined as surgeon volume. The main outcome was operation time. Secondary outcome rate of complications and tertiary outcome factors that might influence the learning process.
All data for this study was extracted from a local appendectomy register. The study was approved by the Swedish Ethics Review Authority (2019-05976). The register covers all patients >aged 9 years with acute appendicitis admitted from the emergency department for further treatment at Södersjukhuset in Stockholm. Data from appendectomies were collected from the surgical planning software (Orbit 5, Evry) and transferred to a database. The register was validated through a retrospective review of the medical records. Three people at the surgical department with a medical education were responsible for the validating the register. All procedures coded “JEA00” and “JEA01” (ICD-10 classification for appendectomy and laparoscopic appendectomy) were identified and then sorted by primary surgeon.
Definition of Complications
The complications in the register were specified in text retrieved from a medical chart review. This was done to specify which type of complication. A bleeding complication was defined as bleeding that required follow-up, additional haemoglobin testing, radiology, or reoperation. Postoperative mechanical ileus was defined as a condition requiring oral contrast and or surgery. Postoperative paralytic ileus was defined as absence of bowel movements longer than expected and verified radiologically or clinically. A surgical site infection was defined as a wound complication needing additional or prolonged antibiotics, or wound debridement. Intra-abdominal abscess was defined as an abscess verified with radiology, with or without percutaneous drainage. Other complications such as urinary tract infection and wound dehiscence were registered based on the judgement of the reviewers.
Surgical technique
The routine surgical technique for laparoscopic appendectomy at Södersjukhuset is diathermy hooking plus stapling of the appendix base. Intraoperative antibiotic prophylaxis is generally given. To begin with, surgery is performed by a trainee as primary surgeon with the assistance of a senior colleague holding the camera. When considered capable, the trainee performs the procedure independently, though there is always a senior surgeon who can be called in for assistance.
Statistical analysis
The method of moving average of order 10 was used to build learning curves for each trainee and to study how the trend in operation time followed increase in experience. The cumulative sum (CUSUM) technique was utilised to chart changes in the complication rates of the trainees. The CUSUM technique uses a sequential probability ratio test recognising the importance of time as a “hidden variable” in clinical studies and thus avoiding the statistical problems associated with repeated significance testing [12]. Moreover, the CUSUM technique detects clusters of surgical failures during the patient care process rather than after an arbitrary unit of time, thus alerting the trainee to suboptimal performance. In this study, CUSUM was defined as- Sn (Sn+1=max (0, Sn+xi, x0)) in which xi 1 for “failure” (complication) and xi 0 for “success” (no complication), whereas x0 is the reference or target value. In this study, x0 for the conversion rate was set at 0.05, indicating that the target complication rate was 5%. When plotting outcomes on the CUSUM curve, the slope of the curve reveals trend in performance relative to the target complication rate. A positive slope implies that the target is not being me whereas, a negative slope implies that the target is has been exceeded and a level slope indicates that the target is being met and maintained. We applied a classification tree to identify factors associated with operation time and to stratify groups of patients with similar operation times. We used the CHAID algorithm to build the tree [13]. A chi-squared automatic interaction detection (CHAID) analysis starts with all data in one group. The test then finds the factor split that leads to the strongest association with the main outcome: operation time (continuous). Nine possible independent factors were chosen (Table 1). The resulting groups were split until one of the following stop criteria was reached: tree depth was limited to three levels, no groups with less than 15 patients were formed, and no split with a Bonferroni adjustment of less than 0.05 was executed. Statistical analyses were carried out in SPSS version 27 and R Core Team (2020).
Results
The surgical trainee cohort (n=9) performed 586 procedures as primary surgeon. Laparoscopic appendectomy was performed in 97.6% of procedures. In figure 1, the learning curve reached a plateau phase in operation time after approximately 60 procedures. Shortest versus longest mean operation time (41 min versus 89 min). Furthermore, table 1 shows the tree analysis of exposure variables associated with operation time. The most influential impact factor was the pervading technical performance of the individual surgical trainee.
|
Count |
n% |
||
|
Age |
<18 |
179 |
30.4% |
|
19-30 |
128 |
21.8% |
|
|
31-45 |
135 |
23.0% |
|
|
46-65 |
94 |
16.0% |
|
|
>65 |
51 |
8.7% |
|
|
Gender |
Female |
263 |
44.9% |
|
Male |
322 |
54.9% |
|
|
ASA-class |
1 |
331 |
56.5% |
|
2 |
209 |
35.7% |
|
|
3 |
21 |
3.6% |
|
|
Trainees |
Missing |
25 |
4.3% |
|
Trainee 1 |
82 |
14.0% |
|
|
Trainee 2 |
56 |
9.6% |
|
|
Trainee 3 |
98 |
16.7% |
|
|
Trainee 4 |
56 |
9.6% |
|
|
Trainee 5 |
90 |
15.4% |
|
|
Trainee 6 |
35 |
6.0% |
|
|
Trainee 7 |
55 |
9.4% |
|
|
Trainee 8 |
44 |
7.5% |
|
|
Trainee 9 |
70 |
11.9% |
|
|
Operation approach |
Laparoscopic |
572 |
97.6% |
|
Open |
14 |
2.4% |
|
|
Perforation |
No |
400 |
68.3% |
|
Yes |
186 |
31.7% |
|
|
Cumulative number of procedures performed |
<10 |
90 |
15.4% |
|
Nov-20 |
90 |
15.4% |
|
|
21-30 |
90 |
15.4% |
|
|
31-40 |
85 |
14.5% |
|
|
41-50 |
74 |
12.6% |
|
|
>51 |
157 |
26.9% |
|
|
Time (days) from last operation |
<15 |
426 |
73.8% |
|
16-30 |
76 |
13.2% |
|
|
31-45 |
23 |
4.0% |
|
|
46-60 |
21 |
3.6% |
|
|
>61 |
31 |
5.4% |
|
Table 1: Patient characteristics. Tree analysis of exposure variables associated with operation time. Mean age 33 years, and standard deviation 19.
This factor was stronger than the accumulated experience of the whole group. In figure 2, for the trainees in Nodes 1 and 2, the second strongest factor influencing operation time was perforation of the appendix, while for those in Node 3 the second strongest influencing factor was accumulated experience. This shows that the factor with strongest impact on operation time is the technical skill of the trainee and not the case complexity, comorbidity, time of day, or time elapsed since the previous procedure. In figure 3, the CUSUM-analysis of complications, most of the trainees were found to have more complications during the first half of the learning curve whereafter rates gradually decreased. However, two trainees continued to have high complications rates throughout the training period. From the local appendectomy register the complication rate was 6.6% for laparoscopic appendectomy and 10.5% for open appendectomy.
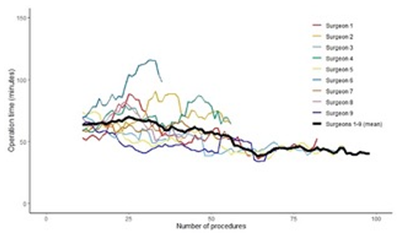
Figure 1: Change in operation time (MA10 moving averages, order 10) according to each trainee, as well as mean operation time. The graph shows a decrease in mean operation time with increasing surgeon volume. Large differences between trainees can be seen.
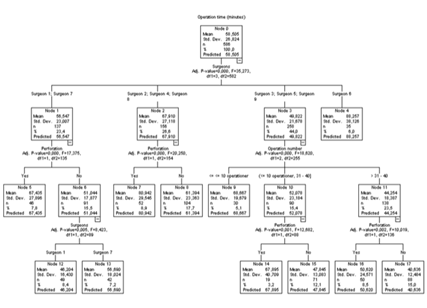
Figure 2: Operation time was associated with trainee performing the procedure (irrespective of surgeon volume), appendix perforation and cumulative number of procedures. Shortest operation times (mean 40.6 minutes) were found for trainees 3,5 and 9 after they had carried out more than 30 procedures without perforation. In contrast, the longest operation times (mean 80.9 minutes) were found among trainees 2,4,8 with perforation. Operation time was not related to time elapsed since previous procedure performed, ASA, gender, laparoscopic or open appendectomy, or age.
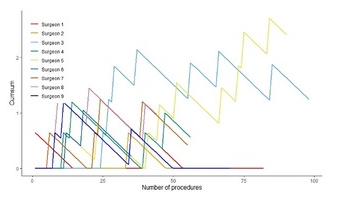
Figure 3: Complications according to trainee (CUSUM analysis). The graph shows differences between complications according to trainee. No falling trend with number of procedures is seen for trainees 3 and 5.
Discussion
In the present study the learning curve was set to about 60 procedures since the trainees reached a steady state in operation time. Although individual variation was large during the learning phase, after 60 procedures times became more congruent. The estimated surgical volume required to acquire proficiency in this study is higher than in other studies [14-16]. As previously mentioned in the introduction, this may be because the Swedish way of training surgeons is structurally different to other countries. In for instance the U.S there is always a more experienced surgeon present in the operating theatre during the critical part of the procedure. This may create shorter learning curves since the route from trainee’s thought to technical execution is faster if someone more experienced is present in the operating theatre. At the time this study was carried out, there was no systematic evaluation tool to objectively test the trainees’ readiness. It is possible that such a tool would have revealed those trainees left without supervision too early. There was a higher rate of complications in the early part of the learning curve. This has also been demonstrated in another setting of surgical volume and time to tumour recurrence [17]. In the tree diagram trainees 3 and 5 were in node 3 with fastest mean operation time but had the highest complication rates after the learning curve. They were also two out of three trainees who in total had the greatest total surgical volume. We can only speculate that it may be to impaired judgement or repeated technical mistake. One of the major limitations of this study is that the extent of guidance during the early phase of the learning curve was not registered. There may have been situations where the trainee at some point needed help by a more experienced surgeon. Another limitation is the choice of main outcome with operation time as a surrogate for defining the learning curve. A more optimal way might have been to use a rating tool for surgical proficiency where extent of guidance (autonomy), trainee performance and case complexity were measured. This may be objectives for future studies, since the use of a national rating tool is not yet implemented at a large scale in clinical practice for general surgery. As it was in this study design, a trainee with a steep learning curve could be assumed to have reached autonomy earlier, which may have influenced the complication rate. Another factor that might have influenced the complication rate is the operation time per se. It is known that the risk for complications increases if the operation time is long. On the other hand, complication rates may be moderated by the fact that trainees are usually assisted by a senior colleague in the very first part of the learning curve. On the other hand, the strength of this study is that the trainees as a group had similar surgical skills experience at the start of the study period and followed throughout their whole residency of five years at the same surgical clinic. All the trainees could be tied to their surgeries and respectively patient outcome, illustrating the individual differences and the actual patient outcome of the surgical education practiced at the time.
Conclusion
To summarize, it is most important to have a well-defined structure for educating the trainees in the operating theatre. The factor having greatest impact on operation time and complication rate was the technical performance of the individual trainee. This study highlights the importance of individually adopted surgical training, even for less complex procedure like appendectomy. This would likely lead to improving the patient’s outcome. How to teach surgical skills in the operating theatre and continuously evaluate the surgical performance of the trainees’ remains a great challenge. This area is of most importance since it is an obvious target for improving patient safety.
List of abbreviations:
ICD: International classification of diseases
CUSUM: Cumulative sum
CHIAD: Chi-Square Automatic Interaction Detector
SPSS: Statistical Package for the Social Sciences
MA: Moving average
Declarations
Ethics approval and consent to participate
The study was approved by the Swedish Ethics Review Authority (2019-05976). Written and verbal information about the register was given to the patients. As the study was purely observational and all patient data were analysed in pseudonymised form, the ethical review authority did not request written consent to the registration.
Consent for publication
Not applicable
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
The study was supported by Stockholm County innovation fund.
Authors' contributions
NY contributed to the design of the work, interpretation of data and major contributor in writing the manuscript.
LB created the patient register, collected the data, validated the register, and helped revising the manuscript.
GS collected the data, contributed to the conception and design of the work, interpretation of data and substantively revised the manuscript.
HPJ contributed to the statistical design, carried out the analysis of the data and drafted the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Peter Cox for skilful language editing
References
- Lin KB, Lai KR, Yang NP, et al. Epidemiology and socioeconomic features of appendicitis in Taiwan: a 12-year population-based study. World J Emerg Surg 10 (2015): 42.
- Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15 (2020): 27.
- Ahlborg L, Weurlander M, Hedman L, et al. Individualized feedback during simulated laparoscopic training:a mixed methods study. Int J Med Educ 6 (2020): 93-100.
- Ahlborg L, Hedman L, Nisell H, et al. Simulator training and non-technical factors improve laparoscopic performance among OBGYN trainees. Acta Obstet Gynecol Scand 92 (2013): 1194-201.
- Hagelsteen K, Langegård A, Lantz A, et al. Faster acquisition of laparoscopic skills in virtual reality with haptic feedback and 3D vision. Minim Invasive Ther Allied Technol MITAT Off J Soc Minim Invasive Ther 26 (2017): 269-277.
- Hagelsteen K, Sevonius D, Bergenfelz A, et al. Simball Box for laparoscopic training with advanced 4D motion analysis of skills. Surg Innov 23 (2016): 309-316.
- Hagelsteen K, Langegård A, Lantz A, et al. Faster acquisition of laparoscopic skills in virtual reality with haptic feedback and 3D vision. Minim Invasive Ther Allied Technol MITAT Off J Soc Minim Invasive Ther 26 (2017): 269-77.
- Mán E, Németh T, Géczi T, et al. Learning curve after rapid introduction of laparoscopic appendectomy: are there any risks in surgical resident participation? World J Emerg Surg 11 (2016): 17.
- Kim SY, Hong SG, Roh HR, et al. Learning curve for a laparoscopic appendectomy by a surgical trainee. J Korean Soc Coloproctology 26 (2010): 324-328.
- Lin YY, Shabbir A, So JBY. Laparoscopic appendectomy by residents: evaluating outcomes and learning curve. Surg Endosc 24 (2010): 125-130.
- Ussia A, Vaccari S, Gallo G, et al. Laparoscopic appendectomy as an index procedure for surgical trainees: clinical outcomes and learning curve. Updat Surg 73 (2021): 187-195.
- Kass GV. An exploratory technique for investigating large quantities of categorical data. J R Stat Soc Ser C Appl Stat 29 (1980): 119-127.
- Bilén K, Ponzer S, Ottosson C, et al. Deliberate self-harm patients in the emergency department: who will repeat and who will not? Validation and development of clinical decision rules. Emerg Med J 30 (2013): 650-656.
- De Wijkerslooth EML, Van den Boom AL, Wijnhoven BPL. Disease burden of appendectomy for appendicitis: a population-based cohort study. Surg Endosc 34 (2020): 116-125.
- Bos C, Doumouras AG, Akhtar-Danesh GG, et al. A population-based cohort examining factors affecting all-cause morbidity and cost after pediatric appendectomy: Does annual adult procedure volume matter? Am J Surg 218 (2019): 619-623.
- Neugebauer E, Troidl H, Kum CK, et al. The E.A.E.S. Consensus Development Conferences on laparoscopic cholecystectomy, appendectomy, and hernia repair. Consensus statements- September 1994. The Educational Committee of the European Association for Endoscopic Surgery. Surg Endosc 9 (1995): 550-563.
- Gottlieb-Vedi E, Mackenzie H, Van Workum F, et al. Surgeon Volume and Surgeon Age in Relation to Proficiency Gain Curves for Prognosis Following Surgery for Esophageal Cancer. Ann Surg Oncol 26 (2019): 497-505.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 