A Rare Case of Pancreatic Pseudocyst with Gastroduodenal Artery Aneurysm Secondary to Chronic Pancreatitis: A Case Report
Amol S Rathod*, Santosh D Thorat, Akshay C Mhase, Ashutosh S Patil, Rajendra N Wabale
Department of General surgery, PCMC’S PGI YCMH, Pimpri, Pune, Maharashtra, India
*Corresponding Author: Amol Shaligram Rathod, Department of General surgery, PCMC’S PGI YCMH, Pimpri, Pune, Maharashtra, India.
Received: 26 December 2023; Accepted: 03 January 2024; Published: 12 January 2024
Article Information
Citation: Amol Shaligram Rathod, Santosh Dashrathrao Thorat, Akshay Changdeo Mhase, Ashutosh Sanjay Patil, Rajendra Namdeo Wabale. A Rare Case of Pancreatic Pseudocyst with Gastroduodenal Artery Aneurysm Secondary to Chronic Pancreatitis: A Case Report. Journal of Surgery and Research. 7 (2024): 17-19.
View / Download Pdf Share at FacebookAbstract
Gastro-duodenal artery aneurysms (GDAAs) are a rare and potentially life-threatening vascular condition with pancreatitis as most common underlying condition. They often remain asymptomatic until rupture, which can lead to catastrophic haemorrhage and mortality. Clinical assessment and radiological.
Investigations should be implicated in timely fashion to diagnose such rare cases. We report a successfully managed case of gastroduodenal artery aneurysm in a patient with chronic pancreatitis.
Keywords
<p>Gastroduodenal artery aneurysm, Pancreatitis, Excision, Visceral artery aneurysm, Case report</p>
Article Details
Introduction
Visceral artery aneurysms are clinical entities labelled any artery that are intra abdominal other than aortoiliac axis .VAAs are rare clinical entities with 0.01%-0.2% incidence out of which 10% has been reported among chronic pancreatitis patients [1]. However, they could be lethal with potential of 25% risk of rupture; which consequently has a mortality rate of 70% [2,3]. Gastro duodenal artery (GDA) aneurysm is among the rarest VAAs; accounting only for 1.5% of the total. After inferior mesenteric artery aneurysm, gastroduodenal artery aneurysm lies on second highest position for its rarity [4]. GDA aneurysm have 75% risk of rupture representing it as a important subcategory of VAAs [5] with gastrointestinal bleeding being the presenting feature in up to 52% of cases [6].
Case Report
A 48 year male came in emergency with complains of pain in the abdomen since 8 days patient was chronic alcoholic and mentioned history of binge alcohol consumption in last 10 days with history of acute pancreatitis earlier. On physical examination, his abdomen was flat, soft, tenderness was present in epigastric region without guarding and rigidity . Laboratory data showed a red blood cell count of 440x104/|il, C-reactive protein (CRP) was elevated to 6.3 mg/dl (normal range, 0-0.5), total bilirubin (T-Bil) 1.7 mg/dl (0. 1-1.2) , asparate-aminotransferase (AST) 115 IU/L(12-33), alanine aminotransferase (ALT) 85 IU/L (5-35), alkaline phosphatase (ALP) 95 IU/L (90-298), y – glutamyl transpeptidase (y-GTP) 55 IU/L (12-75), serum amylase (S-Amy) 387 IU/L (40-130), serum lipase 395 IU/L.
ultrasonography report suggestive of acute necrotizing pancreatitis with peri pancreatic collection of size 9.5*10.2 cm.[App. Vol 150cc]
Contrast enhanced computer tomography suggestive of generalised atrophic pancreas with periphery enhancing cystic lesion of size 11.6*10.5*10.2 cm.
In distal pancreatic body. There is evidence of intensely enhancing lesion of size 2.7*3.6*3.8 cm noted in upper abdomen adjacent to head of pancreas and duodenum. This lesion is seen in continuation with the gastroduodenal branch of common hepatic artery suggestive of arterial aneurysm (Figure 2).
The diagnosis on clinical and radiological basis patient was optimised and planned for exploratory laparotomy for cysto-gastrostomy and GDA ligation and excision.
Operative procedure initiated with mid line laparotomy incision pancreatic bed accessed and pseudocyst visualise. Pseudocyst confirmed with needle aspiration and cysto-gastrostomy performed. Further dissection progressed to coeliac trunk visualisation. Celiac axis visualised and secured with further vascular dissection with visualisation of Right gastric artery, common hepatic artery, left and right hepatic artery, gastroduodenal artery along with its aneurysm visualised (Figure 1). Posterior feeding supply of aneurysm clipped with silicon haemoclip and redundant part excised en-bloc. Haemostasis was maintained throughout the surgery. Abdominal drain placed in pelvis and cysto-gastrostomy bed. Post operatively all routine labs evaluated on day 2 and are as follows HB-12 mg/dl, tlc-8000/ml, platelet- 126000. Drain amylase and lipase value evaluated on day 2 and values are as follows 20 and 28. Drain removed on day 3. Histopathology report was consistent with non specific inflammation with irregular walled congested vessel. The patient was discharged on day 6.
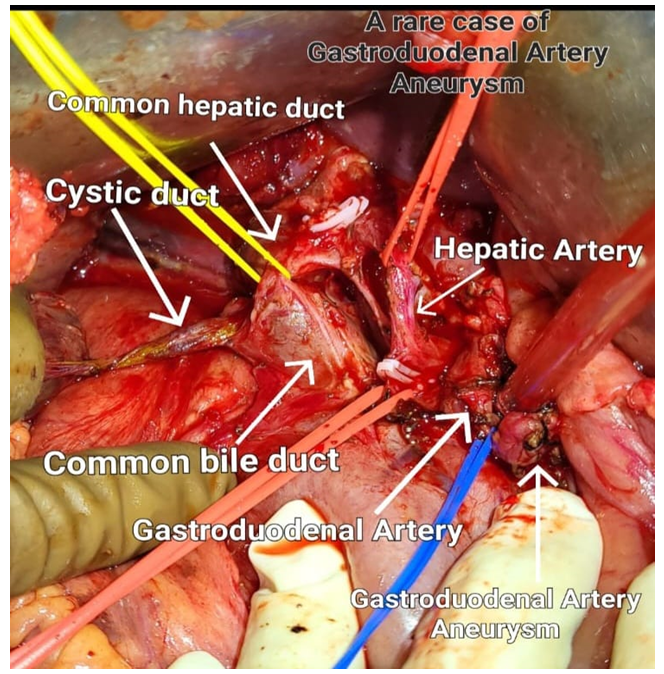
Figure 1: Intra operative image showing visceral arteries and aneurysmal part of gastroduodenal artery.
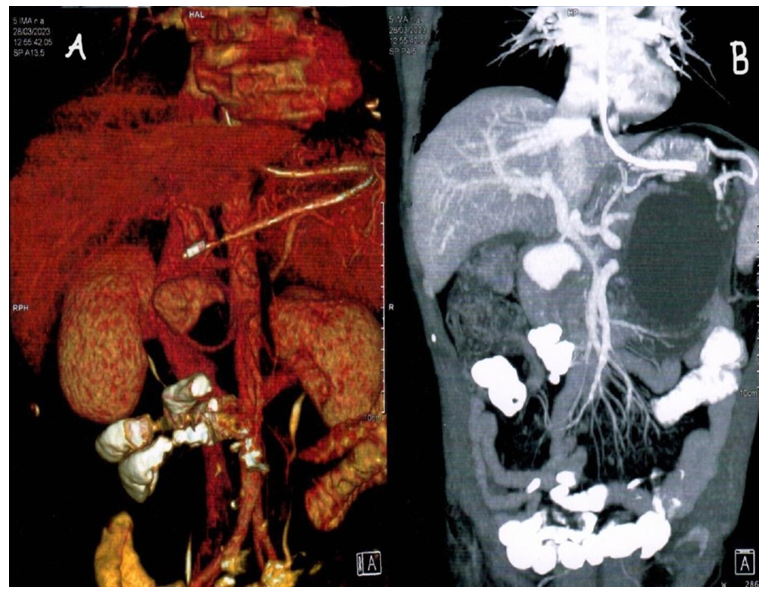
Figure 2: CECT images with vascular reconstruction showing pancreatic pseudocyst with GDA aneurysm.
2A: Vascular reconstruction of computed tomography demonstrating gastroduodenal artery aneurysm; 2B: CECT image demonstrating pancreatic pseudocyst with GDA aneurysm.
Discussion
Gastroduodenal artery aneurysm reported to be rare form. Depending on morphology GDA aneurysm is classified into false and true aneurysm. Common causes reported for GDA aneurysm are chronic pancreatitis, arteriosclerosis, surgical trauma. Other causes are congenital absence of celiac axis, iatrogenic injury during biopsy of head of pancreas and tuberculous infection. In this case repeated bouts of pancreatitis formed to be the underlying cause as it is also associated with pancreatic pseudocyst and leakage of proteolytic enzymes due to pancreatitis leads to vessel wall damage and formation of pseudo aneurysm .If the patient is hemodynamically stable endovascular embolization is gold standard method [7]. Once diagnosed, a GDA must be definitively treated even if small or asymptomatic. On account of its potential to rupture; a drastic event which seems to be unrelated to size. The optimal management approach depends on the mode of presentation and hemodynamic status of the patient [8]. But in this case a pancreatic pseudocyst formed a additional pathology needed to be managed and it can also lead to alter the prognosis. To avail this open surgical procedure is preffered in this case.
Conclusion
Gastroduodenal artery aneurysm are rare entity most common secondary to chronic pancreatitis. As this condition is latent with sudden grave consequences excision of the aneurysm is feasible and safer.
Disclosure statement
All authors have no conflict of interest.
References
- Røkke O, Søndenaa K, Amundsen S, et al. The diagnosis and management of splanchnic artery aneurysms. Scand J Gastroenterol 31 (1996): 737-743.
- Panayiotopoulos YP, Assadourian R, Taylor PR. Aneurysms of the visceral and renal arteries. Ann R Coll 3 of 4 Surg Engl 78 (1996): 412-419.
- Gehlen JM, Heeren PA, Verhagen PF, et al. Visceral artery aneurysms. Vasc Endovascular Surg 45 (2011): 681-687.
- Edogawa S, Shibuya T, Kurose K, et al. Inferior mesenteric artery aneurysm: case report and literature review. Ann Vasc Dis 12 (2013): 98-101.
- Harris K, Chalhoub M, Koirala A. Gastroduodenal artery aneurysm rupture in hospitalized patients: An overlooked diagnosis. World J Gastrointest Surg 27 (2010): 291-294.
- Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res 16 (2013): 4.
- Morita Y, Kawamura N, Saito H, et al. Diagnosis and embolotherapy of aneurysm of the gastroduodenal artery. Rinsho Hoshasen 33 (1988): 555-561.
- McGuire A, Capron B. Outpatient Management of Gastroduodenal Artery Aneurysm. Cureus 28 (2021): 19091.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 