A Retrospective Analysis of CPR effectiveness in confirmed or suspected COVID-19 patients
Kevin Stepanek*, Mohamad A. Hatahet
St Joseph Mercy Hospital. 44405 Woodward Ave, Pontiac MI 48341, USA
*Corresponding Author: Kevin Stepanek, St Joseph Mercy Hospital. 44405 Woodward Ave, Pontiac MI 48341, USA
Received: 19 February 2024; Accepted: 26 February 2024; Published: 05 March 2024
Article Information
Citation: Kevin Stepanek, Mohamad A. Hatahet. A Retrospective Analysis of CPR effectiveness in confirmed or suspected COVID-19 patients. Journal of Surgery and Research. 7 (2024): 107-111.
View / Download Pdf Share at FacebookAbstract
Background: The idea for this study is to investigate if patients with COVID-19 had worse cardiac arrest outcomes as compared to patients without COVID-19.
Objectives: Our goal is to compare cardiac arrest outcomes in the context of individual patient variables such as COVID-19 results, age, and comorbid condition. We hypothesize worse prognosis for COVID-19 patients, and this may be beneficial in discussions about prognosis and to help providers establish goals of care.
Methods: A retrospective review was conducted of 9,522 patients admitted between March 2020 and November 2021. Data collected included age, sex, COVID-19 PCR result, length of stay, CODE BLUE (cardiac arrest), result of code and hospitalization, and specific cardiac indices such as ejection fraction and cardiac biomarkers.
Results: This study found 3,392 patients (35.6%) were COVID-19 positive/suspected. There was a higher incidence of CODE BLUE (p = 0.01) in the COVID-19 positive / suspected group. There was a higher incidence of patient expiration in the COVID-19 positive / suspected group (p = 0.01). There was a significant association with expiration after CODE BLUE in COVID-19 positive/suspected patients. Patients with an elevated troponin or BNP had more cardiac arrests and worse post-arrest outcomes, regardless of COVID-19 result. There was no difference in Ejection Fraction and outcomes, regardless of COVID-19 result.
Conclusions: This study found a significantly higher incidence of cardiac arrest in patients with confirmed/suspected COVID-19. The post-arrest outcomes were also worse for COVID-19 positive/suspected patients. Elevated cardiac biomarkers correlate with more cardiac arrest and worse outcomes overall.
Keywords
<p>COVID-19, Cardiac Arrest, Cardiac Biomarkers</p>
Article Details
Abbreviations:
CODE BLUE interchangeable with cardiac arrest
Introduction
The purpose of this study is to evaluate the effectiveness of cardiopulmonary resuscitation (CPR) in patients affected by SARS-CoV-2. Our goal was to evaluate all patients who underwent cardiac arrest at our facility and compare their success rates and investigate if there were any significant differing characteristics in patients who tested positive or negative for COVID-19. Our hypothesis was that the success rate of patients undergoing cardiac arrest while also afflicted by COVID-19 would be worse than those patients who were negative for COVID-19. Cardiac arrest will be used interchangeably with “CODE BLUE” throughout the article, which refers to our facility’s in-house activation of the advanced life support team for a pulseless patient actively undergoing CPR.
Background
A study published in April 2020 evaluated how many COVID-19 patients suffered cardiac arrest while admitted to their facility and survived to discharge out of the hospital [1]. They reviewed 1,309 patients hospitalized with COVID-19 and found that none of the 54 documented cases of cardiac arrest survived to discharge [1]. There was an additional study conducted in September 2020 that reviewed 136 COVID-19 patients who suffered from in-hospital cardiac arrest. This single center study found that of the 136 patients who underwent CPR, only 18 of them (13%) achieved return of spontaneous circulation (ROSC) and only 1 patient (< 1%) had meaningful neurologic outcome after 30 days [3].
One of the other questions this raised was safety for providers in the event of cardiac arrest in a COVID-19 patient. Within the context of the COVID-19 pandemic, a February 2021 study investigated the effect chest compressions and defibrillation had on generating aerosols in a swine cardiac model [2]. That study found there was no significant increase in aerosol generation from chest compressions alone, however it showed that there was an increase in aerosol generation from the chest compressions immediately following defibrillation [2]. There are several societies that put forth guidelines regarding basic life support (BLS) and advanced cardiac life support (ACLS) in COVID-19 patients. The American Red Cross recommends wearing PPE including N95 mask (or equivalent), eye protection, disposable gloves and a disposable isolation gown [6]. They also recommend that a facemask be placed over the nose and mouth of the victim. To prevent disease transmission, Red Cross does not recommend rescue breaths in patients with confirmed or suspected COVID-19 due to risk of disease transmission. Additionally, they recommend visual assessment of breathing but not auditory or tactile assessment. As well, the American Heart Association has published updated BLS and ACLS algorithms for patients with suspected or confirmed COVID-19 that both began with ensuring proper personal protective equipment (PPE) and scene safety [7]. Additionally, once CPR begins they recommend a high-efficiency particulate air (HEPA) filter. Our facility guidelines as of January 2022 specify a difference between cardiac arrest that occurs in confirmed COVID-19 negative patients as compared to confirmed COVID-19 positive or suspected patients. If the patient has a confirmed negative COVID-19 PCR, our policy is to begin CPR as possible with current standard care PPE - surgical mask and eye protection. It is not recommended to delay compressions or resuscitative efforts to obtain an N95 or to apply a mask or nonrebreather to the patient. In the event of in-hospital cardiac arrest occurring in a patient who has a positive or pending COVID-19 PCR, it is not recommended for providers to enter the room until full PPE is applied. A full set of PPE includes a disposable gown, eye protection, gloves, and a N95 or PAPR. For oxygen supplementation, it is recommended to apply non rebreather at 100% until respiratory therapy arrives and can utilize an Ambu bag with viral filter. The recommendation to have a second provider to maintain a tight airway seal is unchanged. For compressions, the use of an automated chest compressor (LUCAS) can be considered to limit required personnel in the room and is frequently utilized in our critical care units.
Regarding cardiac implications in COVID-19, a July 2020 study reviewed 35 published articles and found that it was associated with worse prognosis [5]. Specifically, they found hypertension was strongly associated with SARS-CoV-2 infection and could worsen the pro-inflammatory state leading to worse prognosis [5]. In addition, they reviewed multiple cardiac complications including myocarditis, heart failure, myocardial infarction, Takotsubo cardiomyopathy, venous embolism, arrhythmias and medication side effects with respect to COVID-19 [5]. It was highlighted that serial troponins could serve as an important prognostic marker [5]. An August 2021 meta-analysis and systematic review examined 204 articles for an association between heart failure and worse prognosis in COVID-19 patients [4]. They found that patients with heart failure at a significantly increased risk of hospitalization, poor outcome and death from COVID-19. Additionally, it was found that the COVID-19 positive patients with heart failure had a significantly higher mortality than COVID-19 positive patients without heart failure [4].
Methods & Data Collection
This study employed a retrospective cohort for patients admitted to our facility between March 2020 and November 2021. All patients admitted between those dates (and to this date) require a COVID-19 PCR to be performed on admission to determine their destination unit. Our data was gathered with the assistance of the Data and Informatics Department and was analyzed by a statistician. Data gathered included patient age, sex, ethnicity, BMI, COVID-19 PCR result, length of stay, ICU consult, CODE BLUE event, deceased or expiration status, diagnosis of myocarditis, orders for intubation or mechanical ventilation, and results for ejection fraction, troponin, and BNP. Our data was subsequently sorted into 2 groups, COVID-19 positive or suspected and COVID-19 negative. This was because of high clinical suspicion in these cases, and if the patient's COVID-19 PCR resulted their status in our EMR would result from COVID-19 suspected to confirmed positive or negative. COVID-19 testing at our facility is performed via the SARS-CoV-2 RNA qualitative RT-PCR performed on the Abbott Alinity m system.
Within our variables, a BNP was considered to be positive if its value was greater than 100. For troponin, we consider a positive troponin to be >20. For Ejection Fraction, there were no cutoff values and the percentages were compared directly to each other. Additionally, we looked to further define what constitutes a successful result from in-hospital cardiac arrest. Specifically, we examined if the patient survived the CODE BLUE, if they were discharged from the hospital, and what their discharge destination was. Our facility uses CODE BLUE and in-hospital cardiac arrest interchangeably, and the activation of the rapid response / code team comes from a bedside provider (i.e. RN, resident, attending, physical or occupational therapist). As part of our data collection, we looked to identify patients who did not survive their CODE BLUE. Our EMR allows multiple ways for patient death to be coded, namely they can have a “discharge as expired” order, their chart can reflect “deceased” status, or expiration can be listed separately in a discharge summary or elsewhere in the chart. We attempted to utilize all of these possible avenues in our data collection to accurately determine the result of the CODE BLUE event for each patient. Overall, it appeared that having a “deceased'' status attached to the chart was the most accurate reflection of a patient’s current status.
Results
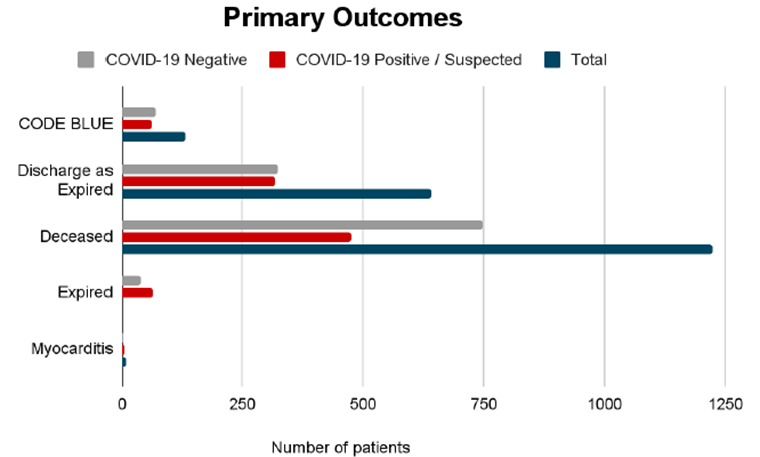
We reviewed 9,522 admitted patients in total. From the SARS-CoV-2 PCR result, 6,130 patients (64.4%) were confirmed COVID-19 negative and 3,392 patients (35.6%) were COVID-19 confirmed positive or COVID-19 suspected. There was a significantly higher incidence of CODE BLUE (p = 0.01) in the COVID-19 positive/suspected group (1.8%) as compared to the COVID-19 negative group (1.2%). There was a significantly higher incidence of "discharge as expired" orders (p < 0.0001) in the COVID-19 positive/suspected group as compared to the COVID-19 negative group (5.3%). There was a significantly higher incidence of deceased status (p = 0.01) in the COVID-19 positive/suspected group (14.0%) as compared to the COVID-19 negative group (12.2%). There was a significant association between CODE BLUE that led to discharge/expiration status in the COVID-19 positive/expected group (p < 0.0001). Of the 62 COVID-19 positive/suspected patients who underwent CODE BLUE, 54 of them (87.1%) did not survive the hospital admission. This was significantly higher than the COVID-19 positive/suspected patients who expired without a CODE BLUE (422/3330, or 12.7%). There was no significant association between COVID-19 result and a diagnosis of myocarditis (p = 0.143). Please refer to Figure 1 below for illustration of these results.
The average Ejection Fraction in COVID-19 positive/suspected patients are displayed in table 1, with those who did not undergo CODE BLUE averaging 55.43%, and in those who did undergo CODE BLUE averaging 57.67%. As seen in table 2, we found that in the COVID-19 positive/suspected group, there was no significant difference in ejection fraction in relation to CODE BLUE (p = 0.367), deceased or not (p = 0.231) or expired status (p = 0.749). There was a significant association in the relationship between BNP and CODE BLUE or deceased/expired status in all patients, regardless of COVID-19 status. Those with a positive BNP were more likely to have a CODE BLUE (COVID negative p < 0.0001, COVID positive/suspected p = 0.002, all patients p < 0.0001) and were more likely to expire in their hospital course (p <0.0001). There was a significant association in the relationship between troponin and CODE BLUE and deceased/expired status, regardless of COVID-19 status. Those with a positive troponin were more likely to have a CODE BLUE (COVID negative p = 0.03, COVID positive/suspected p < 0.0001), all patients (p < 0.0001) and were more likely to expire in the hospital course (p < 0.0001).
|
Ejection Fraction |
CODE BLUE? |
Total # |
Avg EF |
Standard Deviation |
Standard Error Mean |
|
No |
607 |
55.43% |
13.205 |
0.536 |
|
|
Yes |
30 |
57.67% |
14.211 |
2.595 |
Table 1: Total Ejection Fraction results in COVID-19 Positive/Suspected patients.
|
Reduced Ejection |
CODE BLUE |
No |
607 |
|
Yes |
30 |
||
|
P-value |
0.367 |
||
|
Deceased Status |
No |
489 |
|
|
Yes |
148 |
||
|
P-value |
0.231 |
||
|
Discharge to Expired |
No |
528 |
|
|
Yes |
109 |
||
|
P-value |
0.749 |
Table 2: Reduced Ejection Fraction in COVID-19 Positive / Suspected cases as it correlates with incidence of CODE BLUE, Deceased Status, Discharge to Expired.
Discussion
Given that there was a significantly higher incidence of CODE BLUE and death in the COVID-19 positive/suspected group as compared to the COVID-19 negative group, we considered a few theories as to why this occurred. Namely, we suspect that the poor outcome for these patients can be attributed to the severe, muti-faceted nature of a severe SARS-CoV-2 infection requiring hospitalization. On average, patients being treated for COVID-19 were some of the sickest in our facility at any given time. When cases were at their peak during any wave of the pandemic, there were critically ill patients being treated for COVID-19 and occupying most rooms in five units throughout our facility. This included isolation areas in the Emergency Department, an entire wing of the Intensive Care Unit (sometimes with additional overflow), and two entire med-surg floors and an additional half floor with COVID-19 patients in isolation. This severe patient volume became very taxing for every healthcare system across the country, and our hospital went into “pandemic” mode for part of 2020. During this time, there were no elective surgeries, the hospital had additional outside intensivists coming in to round on patients, and the Internal Medicine Residency Program focused solely on COVID-19 patients and rounding due to high hospital demand, with some residents even coming in while on pre-scheduled vacation. Whenever our number of COVID-19 cases increased, it was only natural that a higher percentage of cardiac arrests were going to occur in those patients.
Our facility and larger societies including American Red Cross and American Heart Association include proper PPE as the initial step in resuscitation efforts. The extra steps required to don a gown, eye protection, gloves, and an N95 before entering a COVID-19 isolation room raised questions about delay of care or increased time to having enough providers bedside for effective and appropriate resuscitative efforts. As it is understandable to protect the healthcare providers as they enter the room, we recognize that all current society guidelines list proper PPE as the first component of advanced life support in COVID-19 cases - so it is certainly a commonality in all healthcare facilities across the country. Given that COVID-19 patients would only regularly have one provider in their room at any usual time, i.e. their RN for that shift or a floor tech helping to reposition the patient, transfer the patient, or deliver food, they would be the first point of contact to recognize arrest, impending arrest, or pulselessness. Every room in our facility includes more than one way of activating the hospital-wide CODE BLUE or rapid response system.
One proposed solution to help identify abnormal rhythms faster is to place all COVID-19 patients with isolation orders on telemetry monitoring. As it stands now, any patient on telemetry is under careful observation by our telemetry department, who are excellent at recognizing acute changes in a patient's cardiac rhythm and notifying the nurse directly to immediately check on them. Unfortunately, this solution is limited primarily by staffing, and it assumes there is a robust telemetry system capable of monitoring every bed in the hospital (497 at our facility). Additionally, there are telemetry monitors at all of the nursing stations that provide constant readings for the nearby patient rooms. Unfortunately, proper recognition of an abnormal rhythm on the floor monitors could require additional staffing or assume the staff had downtime to sit, chart and review the monitor. During our peak COVID-19 numbers, our staff was typically so busy that it would not be common for them to have time to sit at these nursing stations for any prolonged period of time and review the telemetry.
From our secondary outcomes, we found positive findings in several cardiac findings to increase the likelihood of cardiac arrest and death. Namely, patients with an elevated BNP or Troponin suffered significantly more cardiac arrests and had significantly worse outcomes than those without elevated levels. There was no statistically significant difference in Ejection Fraction relative to CODE BLUE and patient expiration, and there was no significant association between COVID-19 and a diagnosis of myocarditis. Given the typical presenting scenario of acute respiratory failure from COVID-19, routine testing for Troponin and/or BNP was more common in patients where the disease was found to be positive or suspected. There are no current recommendations regarding routine Troponin and BNP testing in patients presenting with suspected COVID-19, but it is something that can be considered going forward as a prognostic tool.
Conclusion
This study showed that there was a significantly higher incidence of in-hospital cardiac arrest for patients with confirmed or suspected SARS-CoV-2 infection as compared to those who tested negative. Additionally, it showed that these patients were more likely to have worse outcomes from their CODE BLUEs, namely expiration or death. Although limited by current policy for provider safety, we believe it is important to additionally consider the time it takes for PPE donning as well as ways to improve quick recognition of patient decline in isolation rooms. There was no statistically significant difference in regards to Ejection Fraction and cardiac arrest, and there was not a significantly increased incidence of myocarditis in COVID-19 patients. From a cardiovascular biomarker perspective, this data supports elevated Troponin and/or BNP as indicating a worse prognosis and increased likelihood of in hospital cardiac arrest and death regardless of COVID-19 result [5]. Although prior studies found heart failure led to higher mortality in COVID-19 patients, our findings did not support this [4].
We propose that the worse outcomes in these patients can be attributed in part to the severity of the SARS-CoV-2 infection and the disseminated effects it can have on multiple organ systems.
As more patients survive COVID-19 hospitalization and they are then seen in outpatient settings, more data can be collected regarding varying levels of recovery. This can be evidenced by the 2020 study that found only 1 of the 136 COVID-19 patients who suffered in-hospital cardiac arrest had demonstrated meaningful neurologic recovery on follow up [3]. We believe further studies will be useful in identifying more of the long-term sequelae of COVID-19 infections on a multitude of fronts including re-admissions, long term Cardiac Arrest complications and cardiovascular pathologies. It is our hope that further data like this can be used to guide conversations regarding critically-ill patients who are diagnosed with COVID-19 when it comes to goals of care, short term prognosis, long term prognosis, and post-hospitalization recovery.
Limitations
In review of our data, we believe that it comes with several limitations to be mindful of. First, it is certainly possible that a patient could have had multiple cardiac arrests in the same hospitalization. The way our data collection was structured, the number of CODE BLUEs per patient was not quantified. Additionally, we did not collect data on where in the hospital the CODE BLUE occurred, so we can not comment on if the different patient to nursing ratios (i.e. ER vs med-surg vs ICU) contributed to outcomes. As well, CODE BLUE documentation does not include if a LUCAS automatic chest compressor was used. Therefore, we could not compare cardiac arrests treated with a LUCAS to those without and cannot comment on its effectiveness in our data set. In further studies we would like to conduct analysis of vaccination status as they pertain to these findings, but again we found there to be limitations in how each patient’s vaccination status was coded into their chart. For example, sometimes an admitted patient would not be able to provide you with information regarding exactly when and how many COVID-19 vaccinations they received, or they may not be able to communicate with you or their family may not have that information.
References
- Thapa SB, Kakar TS, Mayer C, et al. Clinical outcomes of in-hospital cardiac arrest in COVID-19. JAMA Intern Med 181 (2021): 279-281.
- Cindy HH, Mohamad HT, André LB, et al. Aerosol generation during chest compression and defibrillation in a swine cardiac arrest model, Resuscitation 159 (2021): 28-34.
- Modes ME, Lee RY, Curtis JR. Outcomes of cardiopulmonary resuscitation in patients with COVID-19 Limited Data, but Further Reason for Action. JAMA Intern Med 181 (2021): 281-282.
- Yonas E, Alwi I, Pranata R, et al. Effect of heart failure on the outcome of COVID-19 - A meta analysis and systematic review. Effect of heart failure on the outcome of COVID-19 - A meta analysis and systematic review. Am J Emerg Med 46 (2021): 204-211.
- Azevedo RB, Botelho BG, Hollanda JVG, et al. Covid-19 and the cardiovascular system: a comprehensive review. J Hum Hypertens 35 (2021): 4-11.
- First Aid/CPR/AED care during COVID-19. Red Cross (2023).
- Coronavirus (COVID-19) Resources for CPR Training. American Heart Association CPR & First Aid (2022).


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 