Barramundi - A Local Favourite as Cause of Fishbone Perforation of The Pylorus- 2 Case Reports and a Review of Literature
Article Information
Henry Liao*, Chinthaka Wijesurendere
Department of Surgery, Royal Darwin Hospital, Northern Territory, Australia
*Corresponding Author: Henry Liao, Department of Surgery, Royal Darwin Hospital, Northern Territory, Australia
Received: 19 March 2023; Accepted: 27 March 2023; Published: 20 April 2023
Citation: Henry Liao, Chinthaka Wijesurendere. Barramundi- A Local Favourite as Cause of Fishbone Perforation of The Pylorus- 2 Case Reports and a Review of Literature. Journal of Surgery and Research. 6 (2023): 153-155.
View / Download Pdf Share at FacebookKeywords
Fish bone, Perforation, Pylorus, Duodenum, Foreign body, Emergency surgery
Fish bone articles; Perforation articles; Pylorus articles; Duodenum articles; Foreign body articles; Emergency surgery articles
Fish bone articles Fish bone Research articles Fish bone review articles Fish bone PubMed articles Fish bone PubMed Central articles Fish bone 2023 articles Fish bone 2024 articles Fish bone Scopus articles Fish bone impact factor journals Fish bone Scopus journals Fish bone PubMed journals Fish bone medical journals Fish bone free journals Fish bone best journals Fish bone top journals Fish bone free medical journals Fish bone famous journals Fish bone Google Scholar indexed journals Perforation articles Perforation Research articles Perforation review articles Perforation PubMed articles Perforation PubMed Central articles Perforation 2023 articles Perforation 2024 articles Perforation Scopus articles Perforation impact factor journals Perforation Scopus journals Perforation PubMed journals Perforation medical journals Perforation free journals Perforation best journals Perforation top journals Perforation free medical journals Perforation famous journals Perforation Google Scholar indexed journals Pylorus articles Pylorus Research articles Pylorus review articles Pylorus PubMed articles Pylorus PubMed Central articles Pylorus 2023 articles Pylorus 2024 articles Pylorus Scopus articles Pylorus impact factor journals Pylorus Scopus journals Pylorus PubMed journals Pylorus medical journals Pylorus free journals Pylorus best journals Pylorus top journals Pylorus free medical journals Pylorus famous journals Pylorus Google Scholar indexed journals Duodenum articles Duodenum Research articles Duodenum review articles Duodenum PubMed articles Duodenum PubMed Central articles Duodenum 2023 articles Duodenum 2024 articles Duodenum Scopus articles Duodenum impact factor journals Duodenum Scopus journals Duodenum PubMed journals Duodenum medical journals Duodenum free journals Duodenum best journals Duodenum top journals Duodenum free medical journals Duodenum famous journals Duodenum Google Scholar indexed journals Foreign body articles Foreign body Research articles Foreign body review articles Foreign body PubMed articles Foreign body PubMed Central articles Foreign body 2023 articles Foreign body 2024 articles Foreign body Scopus articles Foreign body impact factor journals Foreign body Scopus journals Foreign body PubMed journals Foreign body medical journals Foreign body free journals Foreign body best journals Foreign body top journals Foreign body free medical journals Foreign body famous journals Foreign body Google Scholar indexed journals Emergency surgery articles Emergency surgery Research articles Emergency surgery review articles Emergency surgery PubMed articles Emergency surgery PubMed Central articles Emergency surgery 2023 articles Emergency surgery 2024 articles Emergency surgery Scopus articles Emergency surgery impact factor journals Emergency surgery Scopus journals Emergency surgery PubMed journals Emergency surgery medical journals Emergency surgery free journals Emergency surgery best journals Emergency surgery top journals Emergency surgery free medical journals Emergency surgery famous journals Emergency surgery Google Scholar indexed journals emergency department articles emergency department Research articles emergency department review articles emergency department PubMed articles emergency department PubMed Central articles emergency department 2023 articles emergency department 2024 articles emergency department Scopus articles emergency department impact factor journals emergency department Scopus journals emergency department PubMed journals emergency department medical journals emergency department free journals emergency department best journals emergency department top journals emergency department free medical journals emergency department famous journals emergency department Google Scholar indexed journals post-operative day articles post-operative day Research articles post-operative day review articles post-operative day PubMed articles post-operative day PubMed Central articles post-operative day 2023 articles post-operative day 2024 articles post-operative day Scopus articles post-operative day impact factor journals post-operative day Scopus journals post-operative day PubMed journals post-operative day medical journals post-operative day free journals post-operative day best journals post-operative day top journals post-operative day free medical journals post-operative day famous journals post-operative day Google Scholar indexed journals gastroscopy articles gastroscopy Research articles gastroscopy review articles gastroscopy PubMed articles gastroscopy PubMed Central articles gastroscopy 2023 articles gastroscopy 2024 articles gastroscopy Scopus articles gastroscopy impact factor journals gastroscopy Scopus journals gastroscopy PubMed journals gastroscopy medical journals gastroscopy free journals gastroscopy best journals gastroscopy top journals gastroscopy free medical journals gastroscopy famous journals gastroscopy Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals
Article Details
Cases
Barramundi, also known as the Asian sea bass or sea perch, inhabits the waterways, estuaries as well as the coastal regions of East Asia, Southeast Asia and northern Australia. Here, we present two unusual cases of fish bone perforation through the pylorus and duodenum from ingestion of this iconic Australian fish, a local favourite of the population of Darwin.
A fit and healthy 37-year-old man presented to the emergency department with a 3-day history of band like epigastric abdominal pain that was sharp and constant. Prior to the onset of symptoms, the patient recalls a meal containing barramundi but no recollection of fishbone ingestion specifically. Physical examination revealed a tender, locally peritonitic epigastrium. Laboratory tests showed elevated white cell count and C-reactive protein. A contrast computed tomography (CT) abdomen and pelvis revealed minor inflammation centred around the pylorus and first part of the duodenum with a hyper-enhancing curvilinear structure- initially reported as the gastroduodenal artery (Figure 1). Further review with the radiology department concluded it was more likely an eroding 28mm fishbone. Initial gastroscopy to D4 showed no endoscopic evidence of foreign body injury and the patient proceeded to a laparoscopy. A Small 2-3mm perforation was found at D1 from erosion of the fishbone. There were small amounts of local peritonitis and fibrin that was walled off by the omentum. The fishbone was removed with graspers, the duodenal defect was oversewn with 3-0PDS and an omental patch was anchored to the repair. The patient recovered well with no complications and was discharged on post-operative day (POD) five.
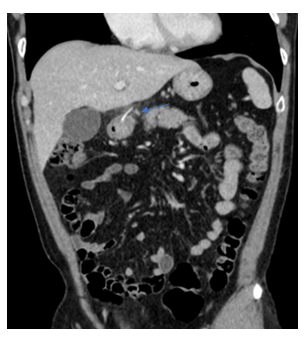
Figure 1: Coronal contrast enhanced CT image of Patient One demonstrating hyperdense curvilinear foreign body penetrating the gastric pylorus/ first part of the duodenum (arrow).

Figure 2: Coronal contrast enhanced CT image of Patient Two demonstrating hyperdense curvilinear foreign body penetrating the pylorus (arrow).
The second case was a 68-year-old man who presented to his family doctor in remote Northern Territory with a 1 month history of unspecific symptoms including weight loss, loss of appetite and general malaise. The patient had a history of ischaemic heart disease, chronic obstructive pulmonary disease and type two diabetes mellitus. The patient was booked for upper and lower endoscopic investigations and CT of the chest, abdomen and pelvis to rule out malignancy. CT demonstrated a 34mm linear hyperdense structure traversing the posterior wall of the gastric pylorus with minimal adjacent fat stranding but no free fluid or free gas; representing ingested fishbone and chronic in nature (Figure 2). On arrival via low acuity transfer, physical examination revealed no abdominal pain. The patient had normal laboratory findings. Initial gastroscopy was normal to D2 and showed no evidence of foreign body perforation and the patient proceeded to a laparoscopy. The fishbone was identified within a fibrous capsule of fatty fibrinous tissue posterosuperior to the pylorus. Close inspection of the pylorus after removal of fishbone by graspers showed no defect. The fishbone had completely eroded through and the pylorus had sealed off spontaneously. The patient recovered well with no complications and was discharged POD six.
Discussion
Foreign body (FB) ingestion is a common clinical presentation to the emergency and surgical departments. Large retrospective studies show that most ingested FBs passes through the gastrointestinal tract (GIT) spontaneously, around 10-20% require endoscopic removal and <1% develops perforation within the GIT and may necessitate surgical intervention [1,2]. Sharp FBs such as fishbone account for large proportion of perforations, as high as 84% in some studies, especially in coastal populations where fish accounts for a large part of the diet, as is the setting of the two cases presented [3,4]. The main risk factor is dentures in the elderly due to loss of tactile feedback, but also include mental retardation, alcohol abuse and age at both extremes [2].
Sites of fishbone perforation vary and has been reported throughout the GIT in its entirety from the cricopharyngeus to the anus; with unusual perforations through Meckel’s diverticulum and appendix reported [4,5]. The most frequent sites are the ileum, ileocecal valve and rectosigmoid junction as well as the lesser curvature of the stomach and duodenum- areas of sharp angulation and where mobile and immobile segments of the GIT meet [1,2,4,6,7]. The sharp FB penetrates the mucosa, impaction causes local ischemia which leads to perforation. The FB can completely penetrate through the bowel wall and cause localized sepsis or abscesses. Complications include hepatic abscesses, fistulas, vascular injury or pseudoaneurysms including to the aorta [8-11].
Due to the variable sites of impaction or perforation, patients often present with acute abdominal symptoms mimicking other pathologies such as cholecystitis, peptic ulcer disease, appendicitis or diverticulitis. Some have non-specific systemic symptoms of malaise, weight loss or fever as was the case with Patient 2 [12,13]. Whilst plain radiograph have been reported to identify fishbone FBs, it has a low sensitivity of 33% [1,14]. The majority of fishbone are radiolucent and is species dependent from varying bone densities [15]. Computed tomography (CT) is the definitive imaging modality due to its quick acquisition and technological advancements. CT has a reported sensitivity of 71-100% with thin slice thickness of 1.5-2mm allowing accurate localization of the FB in patients with unspecific symptoms [4,12,16]. Pitfalls to consider however, include the use of oral contrast obscuring the fishbone, cricoid cartilage calcification, artefacts from colonic faecal matter, and contrast enhanced small blood vessels, as was initially misreported with Patient 2 [16].
Management of fishbone perforation range from conservative to surgical and is dependent on location and patient’s biochemical and clinical signs of peritonitis or sepsis. Non-operative management with antibiotics for micro perforations have been reported [7,17]. Endoscopic removal is also safe, and adequate in 98% of patients in a large series of 358 patients [1].
Developments in endoscopic submucosal dissection (ESD) techniques have allowed completely embedded fishbones, localized with pre-operative CTs, showing no or minimal endoscopic evidence of foreign body perforation, to be removed via endoscopic mucosal incision. Eleven such case reports are found in the literature in recent years [18].
Surgery is indicated in perforations complicated by bowel or vascular involvement, gross peritonitis, abscess formation, migration or fistulation into adjacent structures. Simple repair versus segmental resection is dependent on the size of perforation, the location and condition of the affected bowel and degree of the contamination. Early intervention should be considered to prevent potentially severe morbidity and mortality associated with GIT perforations [19].
Conclusion
Fishbone perforation from ingestion is an uncommon occurrence. Presentation and symptoms can be widely varied and present a diagnostic dilemma. Detailed history taking is required regarding food intake. Computed tomography should be used to localize and correlate areas of interest being cognisant of the potential pitfalls. Early intervention in cases of complicated perforation reduces further morbidity and mortality for the patients.
References
- Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 211 (1990): 459-462.
- Velitchkov NG, Grigorov GI, Losanoff JE, et al. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg 20 (1996): 1001-1005.
- Leong HK, Chan RK. Foreign bodies in the upper digestive tract. Singapore medical journal 28 (1987):162-165.
- Venkatesh SH, Venkatanarasimha Karaddi NK. CT findings of accidental fish bone ingestion and its complications. Diagn Interv Radiol 22 (2016): 156-160.
- Santos B, Pinto A, Barbosa B, et al. Perforation of Meckel's diverticulum by a swallowed fish bone: case report and literature review. J Surg Case Rep 2019 (2019): rjz003.
- Goh BK, Chow PK, Quah HM, et al. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg 30 (2006): 372-377.
- Ward MA, Tews MC. Small bowel perforation secondary to fish bone ingestion managed non-operatively. J Emerg Med 43 (2012): e295-298.
- Bekki T, Fujikuni N, Tanabe K, et al. Liver abscess caused by fish bone perforation of stomach wall treated by laparoscopic surgery: a case report. Surg Case Rep 5 (2019): 79.
- Choi Y, Kim G, Shim C, et al. Peritonitis with small bowel perforation caused by a fish bone in a healthy patient. World J Gastroenterol 20 (2014): 1626-1629.
- Konishi T, Hamabe A, Tabata H. Esophageal Perforation by Fish Bone Complicated with Pseudoaneurysm. Intern Med 59 (2020): 2197.
- Mora-Guzman I, Valdes de Anca A, Martin-Perez E. Intra-abdominal abscess due to fish bone perforation of small bowel. Acta Chir Belg 119 (2019): 66-67.
- Ichikawa S, Onishi H, Motosugi U. Computed Tomography Findings of Emergency Cases Resulting From Fish Bone Ingestion. Canadian Association of Radiologists journal 72 (2021): 432-437.
- Paixao TS, Leao RV, De Souza N, et al. Abdominal manifestations of fishbone perforation: a pictorial essay. Abdom Radiol (NY) 42 (2017): 1087-1095.
- Su FJ, Lin IL, Yan YH, et al. Fishbone perforation of the gastrointestinal tract in patients with acute abdominal pain: diagnosis using plain film radiography. BMJ Case Rep (2014).
- Ell SR, Sprigg A. The radio-opacity of fishbones- species variation. Clin Radiol 44 (1991): 104-107.
- Goh BK, Tan YM, Lin SE, et al. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol 187 (2006): 710-714.
- Kuo CC, Jen TK, Wen CH, et al. Medical treatment for a fish bone-induced ileal micro-perforation: a case report. World J Gastroenterol 18 (2012): 5994-5998.
- Koito Y, Asano T, Matsumoto S, et al. Endoscopic Mucosal Incision to Remove a Fish Bone Completely Embedded Under the Esophageal Mucosa: A Case Report and Literature Review. Am J Case Rep 23 (2023): e936773.
- Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma 50 (2001): 289-296.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 