Changing Trends in the Decompression of Tension Pneumothorax
Sherreen Yehia Elhariri1*, Hassan Mohamed2, Ismail AS Burud1, Ahmed Elhariri3
1Department of Surgery, International Medical University, Clinical Campus, Seremban, Negeri sembilan, Malaysia
2Maadi Armed Forces Medical Complex, Cairo, Egypt
3Ain Shams University Hospitals, Cairo, Egypt
*Corresponding Author: Sherreen Yehia Elhariri, Surgical Department, International Medical University (IMU), Clinical campus, Jalan Rasah, Seremban, Negeri Sembilan, P.O 70300, Malaysia
Received: 31 October 2019; Accepted: 18 November 2019; Published: 22 November 2019
Article Information
Citation: Sherreen Yehia Elhariri, Hassan Mohamed, Ismail AS Burud, Ahmed Elhariri. Changing Trends in the Decompression of Tension Pneumothorax. Journal of Surgery and Research 2 (2019): 261-266.
View / Download Pdf Share at FacebookAbstract
Tension Pneumothorax (TP) is one of the commonest complication of chest trauma. For many years the management for tension pneumothorax decompression was the immediate insertion of a wide bore Cather (14-16 gauge) into the 2nd intercostal space (ICS) in mid-clavicular line (MCL) followed by the insertion of a chest tube in the 5th ICS anterior to the mid-axillary line (MAL). In 2018 the Advanced Trauma life support (ATLS) guidelines has changed and the ideal place for tension pneumothorax decompression is at the 5th intercostal space anterior to the MAL. The thickness of the chest wall is significantly less at the 5th intercostal space MAL when compared to 2nd ICS in MCL, and that an 8 cm length Cather has a better efficacy in comparison to 5 cm catheter, as proved by radiographic
measurements. In our article we reviewed the literature in response to the new policy in different countries.
Keywords
<p>Chest wall thickness, Needle decompression location, Needle thoracostomy, Tension pneumothorax</p>
Article Details
1. Introduction
Tension Pneumothorax (TP) is one of the commonest complications of chest trauma, often sustained from fractured ribs. It occurs when a “one-way valve” air leaks from the lung or through the chest wall forcing air into the pleural space eventually collapsing the underlying lung and displacing the mediastinum to the opposite side. This causes a decrease in the venous return and compressing the opposite lung and hence reduction in cardiac output [1]. The pathophysiological manifestations are tachypnea, chest pain, hypoxia, extreme dyspnea and altered level of consciousness. On examination patients have hypotension, tachycardia, cyanosis, distended neck veins, tracheal deviation away from the affected hemi-thorax, hyper resonance on percussion and absent breath sounds on the affected side. Diagnosis must be based entirely on clinical findings, and emergency treatment without delay for radiological confirmation is required [1].
2. Current Management of Tension Pneumothorax
For many years the guideline for tension pneumothorax management was the immediate insertion of a wide bore Cather 14-16 gauge into the 2nd intercostal space (ICS) in mid-clavicular line (MCL) followed by insertion of a chest tube in the 5th ICS anterior to the Mid axillary line (MAL) [2]. This has changed as per ATLS guidelines 2018 10th edition recently. Now the ideal site for insertion of a 14-16 gauge Cather 8 cm length is the 5th ICS anterior to mid-axillary line (MAL). Depending on the patient’s body built, using needles as long as 8 cm is mandatory to perform the technique effectively [3]. In the prehospital treatment the anterior site provides direct stabilization and continued observation more easily in a moving ambulance. Catheters placed at the lateral site may be dislodged by the patient's arm or may be obstructed [4]. As shown in (Figure 1) the chest wall thickness (CWT) influences the likelihood of success with needle decompression. Evidence of successful penetration of the pleura by a 5 cm over-the-needle catheter is >50% of the time, whereas an 8 cm over the-needle catheter has success in >90% of the time. In one comparative study, longer (8 cm) compared with shorter (5 cm) needles were associated with a significant improvement in success rates [5]. Studies have also demonstrated that over the-needle catheter placement in the prehospital field into the anterior chest wall by paramedics was too medial in 44% of patients. A standard-length 14 or 16 gauge catheter is nearly always successful. However, the risk of lung injury is increased with a longer needle [5].
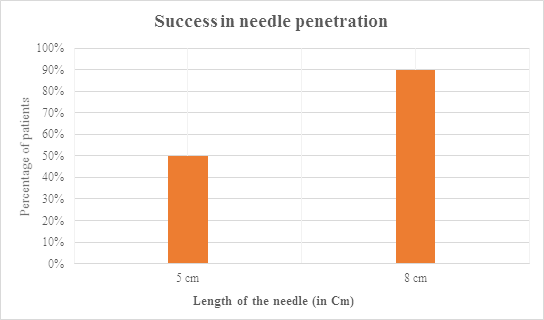
Figure 1: A figure showing that longer (8 cm) compared with shorter (5 cm) needles were directly proportional improvement in success rates.
Recent evidence recommends that placing a 14-16 gauge, 8 cm long catheter at the 5th ICS slightly anterior to the MAL. However, even with an over-the-needle catheter of suitable size, there is still a minimal chance of failure. In view of the risk of subsequent pneumothorax as a result of the maneuver continual assessment of the patient is necessary. Tube thoracostomy is mandatory after decompression of the chest [6].
3. Discussion and Review of Literatures
On review of literatures, using the key words tension pneumothorax, decompression sites, chest wall thickness evaluated radiologically in different population, Length of the needle used in TP, from January 2005 till August 2019 in all articles, titles and abstracts written in English language, using the search agents likes PubMed, MEDLINE and Cochrane library databases we found the following information.
In Singapore, Goh et al. [7], conducted a retrospective review from 2011-2015 on 583 patients who underwent computed tomography (CT) of the chest in patients with TP Four measurements of CWT were taken at the 2nd ICS and 5th ICS at MAL in both sides which includes the whole chest wall thickness and Successful needle thoracostomy (NT) was defined radiologically as CWT ≤ 5 cm. In Asian patients the use of lateral approach and longer catheter is likely to have a higher success rate. Failure of NT is related to higher BMI especially for an anterior approach.
In Japan, Yamagiwa et al. [8] designed a study in trauma patient who underwent CT scan to measure the CWT and determine the accessibility to the pleural space with a 5 cm catheter CWT at 94.3% of sites were <5.0 cm (mean CWT at 2nd ICS at the MCL, 3.06 cm). CWT of women was apparently more than men (P-value (P) <0.05), and they concluded that >94% of trauma patients can be treated with a 5 cm catheter.
In Germany, Hecker et al. [9] found that the use of a 7 cm needle in length is necessary to decompress a tension pneumothorax in the 2nd ICS at the MCL, which might successfully decompress more than 90% of the patients. In this study, in the anterior approach special caution must be taken to avoid injury of internal mammary vessels which run 2 cm from the lateral border of the sternum.
In France, Lamblin et al. [10] used ultrasound in 122 soldiers to measure the CWT on both sides at the second and fourth intercostal space. The study concluded that the CWT was greater than 5 cm in 24.2% of the cases at the second ICS and 4.9% of cases at the fourth ICS (p<0.001). The current practice taught in the French army for NT insertion in 2nd ICS at the MCL had high failure rate which can be improved by using the lateral approach at the 4th ICS.
In Turkey, Akoglu et al. [11] conducted a study that in one third of females and one tenth of males trauma patients the pleural access using a 5 cm catheter is unlikely to be successful irrespective of the puncture site. This can be improved if NT is performed at the 5th ICS at the MAL using 8cm catheter where the CWT is thinner.
In Canada, Zengerink et al. [12] conducted a study that confirmed a catheter length of 4.5 cm may not penetrate the chest wall of a substantial population group dependent of age and gender (9.9%-35.4%). It demonstrated that for the relief of tension pneumothorax in certain population group may require a different needle length to improve the effectiveness of NT.
In USA, when Harcke et al. [13] measured CWT in army soldiers in the second right ICS at the MCL. In comparison to what was reported previously it was noted that the CWT was greater the mean horizontal thickness was 5.36 cm (standard deviation (SD) equal 1.19 cm) with angled (perpendicular) thickness slightly less with a mean of 4.86 cm (SD 1.10 cm). In 99% of the subject in this study an 8 cm catheter would successfully reach the pleural space. Radiologic evaluation by computed tomography-based analysis of chest wall thickness, concluded that failure rate of NT was 42.5% at the 2nd ICS in the MCL in comparison to 16.7% at the 5th ICS at the AAL. The chest wall thickness was 1.3 cm thinner at the 5th ICS at the AAL and may be an ideal location for needle thoracostomy decompression.
Inaba et al. [4] showed a gradual increase in CWT across all BMI quartiles at each site of measurement (2nd ICS at the MCL and 5th ICS at the AAL). Likewise, Powers et al. [14] found that BMI increases proportionally to an increasing CWT. However, their study evaluated CWT only at 2nd ICS at the MCL. This information could be used to select an appropriate needle length for needle thoracostomy. In this study a catheter length of 6-6.5 cm showed higher success in most patient with tension pneumothorax. Ultrasound measurements demonstrate that CWT less than 4.5 cm in most patients and not be the cause of increase in failure rate of needle decompression in tension pneumothorax [15].
Tension pneumothorax decompression using a 3 cm catheter was failed in up to 65% of cases, when a larger 5 cm catheter was used 4% failed [16]. A 5 cm catheter is not suitable for needle thoracostomy in most patient’s whatever of puncture site or gender. Penetration of the pleural space with a catheter length of 6.44 cm was successful in 95% of the patient requiring NT [17]. Pleural decompression has better results with the use of 8 cm catheter in comparison with 5 cm catheter Steeper angle of entry at 4th ICS AAL improves 8 cm non-injury rates to more than 91% [18]. Systematic review and meta-analysis comparing anatomic sites in needle thoracostomy as evident from observational studies suggests that the 4th/5th ICS-AAL has the lowest predicted failure [19]. There was no difference in the mortality of the patients requiring NT with regards to the timing, location of insertion and length of needle [20].
4. Conclusion
The ideal site for tension pneumothorax decompression is at 5th ICS at the anterior to Mid-axillary line (MAL) as the thickness of chest wall is significantly less than thickness at 2nd ICS MCL. An 8 cm catheter has a better chance of pleural decompression when compared with 5cm catheter, as proved by radiographic measurements.
Authors’ Contributions
All the authors critically reviewed the manuscript for its content, contributed to the interpretation and presentation of the review, and approved the final version of the same before submission. Specific contributions by the authors individually has been highlighted below:
Sherreen Elhariri constructed the idea for the article, prepared the manuscript, organized and supervised the course of the article. Hassan Mohamed helped in the preparation and critically reviewed the article before submission, reviews the references, check for plagiarism and critical appraisal. Ismail A.S. Burud critically reviewed the article before submission for its intellectual content and reviews the references. Ahmed Elhariri helped in the preparation and critically reviewed the article before submission for its intellectual content.
Conflict of Interest
There is no conflict of interest or financial support involved in this article.
References
- John Barliz, Faram Baklin, Thomas A Scaletta, et al. Emergency Management of Trauma, Chest Trauma, (3rd) McGraw Hill companies 12 (2011): 149-150.
- Tina Binesh Marvasti, Sydney McQueen. Toronto notes for medical students, Emergency Medicine, chest trauma, (34th) Toronto notes for medical students inc., Toronto, Ontario, Canada (2018): 190.
- Stevens RL, Rochester AA, Busko J, et al. Needle thoracostomy for tension pneumothorax: failure predicted by chest computed tomography. Prehosp Emerg Care 13 (2009): 14-17.
- Inaba K, Karamanos E, Skiada D, et al. Cadaveric comparison of the optimal site for needle decompression of tension pneumothorax by prehospital care providers. J Trauma Acute Care Surg 79 (2015): 1044-1048.
- Aho JM, Thiels CA, El Khatib MM, et al. Needle thoracostomy: Clinical effectiveness is improved using a longer angiocatheter. J Trauma Acute Care Surg 80 (2016): 272.
- ATLS Students course manual (10th Edn). Thoracic Trauma American college of surgeons, Chicago, USA 4 (2018): 66.
- Goh S, Xu WR, Teo LT. Decompression of tension pneumothoraces in Asian trauma patients: greater success with lateral approach and longer catheter lengths based on computed tomography chest wall measurements. Eur J Trauma Emerg Surg 44 (2018): 767-771.
- Yamagiwa T, Morita S, Yamamoto R, et al. Determination of the appropriate catheter length for needle thoracostomy by using computed tomography scans of trauma patients in Japan. Injury 43 (2012): 42-45.
- Hecker M, Hegenscheid K, Völzke H, et al. Needle decompression of tension pneumothorax: Population-based epidemiologic approach to adequate needle length in healthy volunteers in Northeast Germany. J Trauma Acute Care Surg 80 (2016): 119-124.
- Lamblin A, Turc J, Bylicki O, et al. Measure of chest wall thickness in French soldiers: which technique to use for needle decompression of tension pneumothorax at the front? MilitaryMedicine 179 (2014): 783-786.
- Akoglu H, Akoglu EU, Evman S, et al. Determination of the appropriate catheter length and place for needle thoracostomy by using computed tomography scans of pneumothorax patients. Injury 44 (2013): 1177-1182.
- Zengerink I, Brink PR, Laupland KB, et al. Needle thoracostomy in the treatment of a tension pneumothorax in trauma patients: what size needle? J Trauma 64 (2008): 111-114.
- Harcke HT, Pearse LA, Levy AD, et al. Chest wall thickness in military personnel: implications for needle thoracentesis in tension pneumothorax. Mil Med 172 (2007): 12603.
- Powers WF, Clancy TV, Adams A, et al. Proper catheter selection for needle thoracostomy: a height and weight-based criteria. Injury 45 (2014): 107-111.
- McLean AR, Richards ME, Crandall CS, et al. Ultrasound determination of chest wall thickness: implications for needle thoracostomy. Am J Emerg Med 29 (2011): 1173-1177.
- Chad GB, Amy DW, Andrew WK, et al. Thoracic needle decompression for tension pneumothorax: clinical correlation with catheter length. Can J Surg 53 (2010): 184-188.
- Clemency BM, Tanski CT, Rosenberg M, et al. Sufficient catheter length for pneumothorax needle decompression: a meta-analysis, Prehosp Disaster Med 30 (2015): 249-253.
- Chang SJ, Ross SW, Kiefer DJ, et al. Evaluation of 8 cm needle at the fourth anterior axillary line for needle chest decompression of tension pneumothorax. Trauma Acute Care Surg 76 (2014): 1029-1034.
- Laan D, Trang D, Cornelius A, et al. Chest Wall Thickness and Decompression Failure: A Systematic Review and Meta-analysis Comparing Anatomic Locations in Needle Thoracostomy. Injury 47 (2016): 797-804.
- Weichenthal LA, Owen S, Stroh G, et al. Needle Thoracostomy: Does Changing Needle Length and Location Change Patient Outcome?. Prehosp Disaster Med 33 (2018): 237-244.


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 