Cherry Fruit-Stem Stapled into J-J anastomoses during Roux-en-Y Gastric Bypass: A Case Report of a Rare Complication
Logan D Glosser1*, Alexander Young1, Justin Smith1, Conner V Lombardi1, Abdullah Alalwan2, Motaz Al-yafi2, Stephen Stanek3
1University of Toledo College of Medicine and Life Sciences, Toledo, Ohio, USA
2University of Toledo College of Medicine, Department of General Surgery, Toledo, Ohio, USA
3Promedica Toledo Hospital, Department of General surgery, Toledo, Ohio, USA
*Corresponding Author: Logan D Glosser, University of Toledo College of Medicine and Life Sciences, Toledo, Ohio, USA
Received: 22 March 2022; Accepted: 29 March 2022; Published: 18 April 2022
Article Information
Citation: Logan D Glosser, Alexander Young, Justin Smith, Conner V Lombardi, Abdullah Alalwan, Motaz Al-yafi, Stephen Stanek. Cherry Fruit-Stem Stapled into J-J anastomoses during Roux-en-Y Gastric Bypass: A Case Report of a Rare Complication. Journal of Surgery and Research 5 (2022): 194-201.
View / Download Pdf Share at FacebookAbstract
Introduction
Roux-en-Y gastric bypass (RYGB) surgery is the gold standard intervention for weight loss in patients with morbid obesity. Although the mortality associated with the procedure is reduced compared to no intervention, complications account for a high percent of associated morbidity.
Case Presentation
A 63-year-old female with a history of laparoscopic RYGB 2 years prior presented with a 3-month history of crampy abdominal pain. A CT scan showed an intra-luminal mass near the jejunojejunostomy (JJ) site. Surgical excision of the mass revealed a stalk of tissue stapled into the JJ anastomosis that was identified as a cherry fruit-stem. Unfortunately, the patient returned 3 months later suffering from an incisional hernia, requiring mesh repair.
Discussion
RYGB is one of the most commonly performed procedures in bariatric surgery. Common complications from this that result in abdominal pain include anastomotic leaks or strictures, cholecystitis, gastrointestinal bleeding, internal herniation, and marginal ulceration. No prior literature discusses intermittent obstructive symptoms secondary to a foreign body anchored by the anastomotic staples. Furthermore, there are currently no universal dietary guidelines for patients in the immediate pre-operative period with regard to avoiding certain foods that could get stapled during the anastomotic construction.
Conclusion
There are two main take-away lessons from this case. First, this case denotes an unusual complication following RYGB surgery requiring surgical intervention in which the stem of a cherry fruit was stapled into the JJ anastomosis causing obstruction
Keywords
<p>Roux-en-y gastric bypass, Anastomosis complications, Case report, Small bowel obstruction, Incisional hernia</p>
Article Details
1. Case Report
1.1 Introduction
The obesity epidemic in the US is rampant, with approximately 42% of adults affected [1]. Despite global education and treatment with diet, exercise, and pharmaceutical management, bariatric surgery remains the most effective intervention for weight loss [2]. The current gold standard operation for weight loss is the laparoscopic Roux-en-Y gastric bypass (RYGB). RYGB provides safe and sustainable weight-loss in comparison to alternative approaches such as gastric banding, sleeve gastrectomy, and biliopancreatic diversion [3-5]. RYGB entails dividing the jejunum approximately 45 cm below the gastric outlet and anastomosing it to a 15-30 ml gastric pouch created from the proximal end of the stomach. The remaining stomach pouch with the 45 cm jejunal tail is re-anastomosed to the jejunum 75-150 cm below primary gastro-jejunal pouch [6]. RYGB has proven beneficial by improving insulin resistance, glycemic indices, and reducing excess weight by 50-75% [5-7]. Despite the benefits, there are well-characterized complications including marginal ulcers, gastric dilation, stomal stenosis, volvulus, internal hernia, and anastomotic complications among others [8]. Obstructive symptoms are typically vague (e.g., epigastric pain) and result in non-diagnostic physical exams and inconclusive imaging [9]. Due to these factors, laparoscopic examination or exploratory laparotomy is often necessary if the symptoms become burdensome to the patient. We present the rare case of a women who developed obstructive symptoms 2 years following her RYGB procedure. The patient was treated at an academic hospital with surgical intervention. A bezoar attached to a stalk of a cherry fruit-stem stapled into the JJ-anastomosis was found. This was managed with exploratory laparoscopy without need for reconsecration of the RYGB or resection of bowel.
1.2 Case Presentation
A 63-year-old female with past surgical history of a cholecystectomy with more recent gastric bypass 2 years prior presented with 3 months of crampy left upper quadrant pain and weight loss. One month prior, the patient had an ED visit for severe epigastric pain radiating to the chest and back. A CT of the abdomen and pelvis showed colonic diverticulosis without inflammation (figure 1).
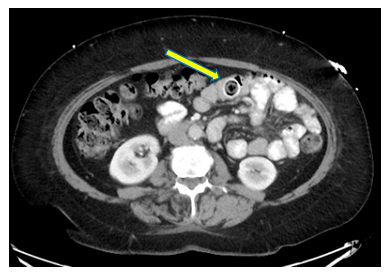
Figure 1: CT scan read as unremarkable in work up at emergency department visit with mass found in retrospect.
Interval esophagogastroduodenoscopy showed no significant findings. The patient reported that bowel movements exacerbated the epigastric pain, with dicycloverine providing relieve. She had been taking MiraLAX ™ since the gastric bypass operation, although felt it had not been helping. On presentation, repeat CT of the abdomen wand pelvis revealed a mass in the bowel near the area of the jejunojejunostomy (JJ) (figure 2). In retrospect, the prior CT demonstrated a round lesion in the proximal small bowel about the size of an olive. The lesion was suspected to be stool due to some solid dense areas and some areas of air density. There was no air in the biliary tree with a common bile duct measuring 2 cm in diameter. This combined with the prior cholecystectomy made a gallstone unlikely. To determine the etiology of the mass and suspected cause of the symptoms the patient elected for a laparoscopy, with possible conversion to open, and planned excision of the mass. An incision was made just beneath the left costal margin through which a 5 mm Optiview port was introduced into the abdomen for insufflation with carbon dioxide. An 11 mm port was then placed to the right of the umbilicus, a 5 mm port placed below the right costal margin, and a 12 mm port placed along the right of the mid-abdomen. The stomach and small bowel were thoroughly explored with particular attention of the GJ anastomosis, the JJ, biliopancreatic limb and the entire common channel down to the ileocecal valve. No masses were appreciated with this manipulation. It was decided to examine the bowel directly. A clamp was placed onto the area of the JJ laparoscopically. A midline incision about 6 cm in length with dissection through 5 cm of subcutaneous fat was made. The midline fascia was opened and the peritoneal cavity was entered. The JJ was elevated to this incision, grasped with a Babcock, and pulled out of the abdomen. With blunt examination a mass attached to a narrow stalk and downward mobility was palpable through the abdominal wall just beyond the JJ in the common channel. An anti-mesenteric incision 2 cm in length was made and we encountered a yellowish-brown structure that crumbled on gross palpation with the particulate matter subsequently suctioned out. Upon removal, a stalk was still present which was followed down to its base and excised. Further inspection revealed that the stalk was stapled into the tissue of the J-J anastomosis. A staple application used to create the JJ during the bariatric operation that passed across a cherry stem. Thus, this stem was unable to move down the bowel and was the nidus for a concretion of material. This lesion would intermittently be caught by bowel contractions and lead to crampy, abdominal pain. On post-operative day 1 she was tolerating liquids, passing flatus, ambulating well. She had not requested or received anything for pain other than Tylenol. The post-operative course was unremarkable and thus she was discharged home that afternoon. In the following months the patient developed an anterior abdominal bulge protruding along the midline. Although the patient was satisfied with the treatment of the anastomotic blockage, follow up CT displayed an incisional hernia (figure 3), requiring surgical repair with mesh.
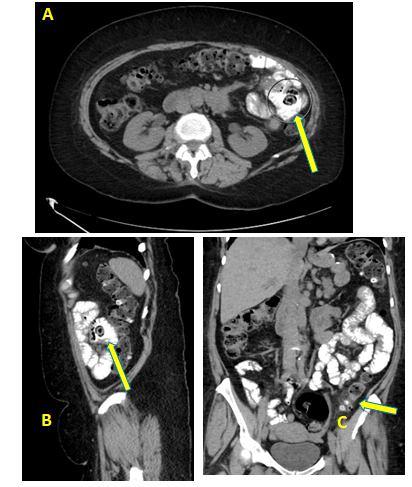
Figure 2: CT scan images identifying obstructive mass (A - axial, B - sagittal, C - coronal).
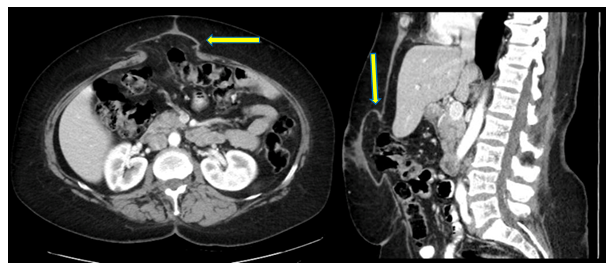
Figure 3: CT Scan demonstrating incisional hernia status post-anastomotic repair.
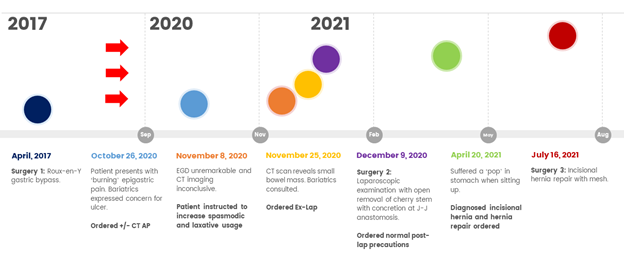
Figure 4: Timeline of events from initial Roux-en-Y gastric bypass to incisional hernia repair with mesh.
2. Discussion
Anastomotic complications after RYGB surgery, although rare, can be a cause of significant morbidity in patients [10]. Anastomotic complications are divided into early (within the first 2 weeks of the procedure) and late (greater than 2 weeks). Early complications include anastomotic leak, bleeding, and edema, whereas late complications include strictures, ulcers, obstruction and internal hernias [11]. Our patient developed late complications of SBO secondary to intermittent anastomotic herniation. The nonspecific presentations of the various RYGB complications make for a challenging diagnosis, even for the astute surgeon. Increased gallstone formation following rapid and massive weight loss in bariatric surgery is well documented. As such, gallstone complications of acute cholecystitis or cholangitis is a common source of nonspecific abdominal pain after bariatric surgery [12]. However, our patient had already undergone cholecystectomy several years prior to her RYGB procedure. The nature and timeline of her cholecystectomy without laboratory findings of hepato-biliary obstruction made acute cholecystitis or retained gallstone unlikely. Small bowel obstructions (SBO) after RYGB are an uncommon, but well-characterized post-operative complication. One study reported that SBOs occurred in 3.8% of patients after RYGB, with adhesions and internal herniations accounting for more than 60% of obstructions [13]. When SBOs do occur, they typically present more than 1 month after the operation, although it can appear years later as seen in our patient. Common etiologies of SBO after gastric bypass include intussusception, internal hernia, hemorrhagic bezoar, and adhesions [14]. The cause of obstruction differs by surgical approach: laparoscopic RYGB is more likely to have obstruction at the JJ site, while adhesive small bowel obstruction is more common following the open approach [10]. This is likely secondary to the inherent differences between open and laparoscopic surgery, as an open approach predisposes to more adhesions which act as the body’s natural defense in preventing intestinal herniation through mesenteric defects [15]. If an obstruction is significant enough to necessitate treatment through bowel resection or restructuring of the JJ anastomosis, patients have significantly worse outcomes [10]. Through the laparoscopic approach, our patient had a partial SBO at the JJ site, in line with the statistical predictability. Three months following the surgical excision of the cherry stem stapled in the JJ anastomosis, the patient developed an incisional hernia. Incisional hernias are reported to occur in 1% of patients after any open abdominal surgery [16]. Our patient then required a third operation to repair the incisional hernia with mesh. Dietary recommendations prior to bariatric surgery vary by institution and no universal guidelines currently exist [17]. Some guidelines specify a liquid-only diet for 1-2 weeks, [17] whereas other institutions recommend having only 1 meal per day with solid food [18]. Regardless of the specific recommendations, there is not an official list of foods that should be avoided preoperatively. Our case suggests that bariatric surgeons provide a specific list of foods to avoid if taking solid foods, or that patients should adhere to the 2 weeks of liquid only diet.
3. Conclusion
This case demonstrates an unusual etiology of abdominal pain following RYGB: SBO at the JJ site following the inadvertent introduction of a cherry stem into the anastomotic stapling. This stem then acted as a nidus for the development of a bezoar which intermittently obstructed the small intestine at the distal alimentary limb. Early diagnosis and surgical exploration in suspected cases can provide immediate relief and limit the suffering of patients, although it also exposes patients to increased risk of surgical complications. Our case has 2 primary lessons from which to learn. First, surgeons need to be aware of the potential complication of non-digestible food impaction at the anastomotic sites. Second, there is a need for standardized dietary guidelines for the 2-week pre-operative period. This case suggests that patients should adhere to a liquid diet leading up to the surgery to avoid inadvertent stapling of non-digestible foods.
Consent
Written patient informed consent was obtained with signature.
Conflict of interest statement
The authors have declared no conflicts of interest.
References
- Adult Obesity Facts CDC.gov: USA.gov 2017-2018.
- O'Brien PE, McPhail T, Chaston TB, et al. Systematic review of medium-term weight loss after bariatric operations. Obes Surg 16 (2006): 1032-1040.
- Osland E, Yunus RM, Khan S, et al. Late Postoperative Complications in Laparoscopic Sleeve Gastrectomy (LVSG) Versus Laparoscopic Roux-en-y Gastric Bypass (LRYGB): Meta-analysis and Systematic Review. Surg Laparosc Endosc Percutan Tech 26 (2016): 193-201.
- Li JF, Lai DD, Lin ZH, et al. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech 24 (2014): 1-11.
- DeMaria EJ, Pate V, Warthen M, et al. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 6 (2010): 347-355.
- Seeras K, Acho RJ, Lopez PP. Roux-en-Y Gastric Bypass Chronic Complications. Stat Pearls. Treasure Island (FL), (2021).
- Rubino F, Kaplan LM, Schauer PR, et al. The Diabetes Surgery Summit consensus conference: recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg 251 (2010): 399-405.
- Mustafa W, Aman MKES MD, Thomas H Magnuson, et al. Intestinal Complications after Roux-en-Y Gastric Bypass. Bariatric Times 12 (2015): 14-18.
- Elkbuli A, Santarone K, Kinslow K, et al. A rare case of internal hernia, intussusception and volvulus following gastric bypass: A case report and literature review. Int J Surg Case Rep 67 (2020): 178-182.
- Nelson LG, Gonzalez R, Haines K, et al. Spectrum and treatment of small bowel obstruction after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2 (2006): 377-383.
- Silecchia G, Iossa A. Complications of staple line and anastomoses following laparoscopic bariatric surgery. Ann Gastroenterol 31 (2018): 56-64.
- Karadeniz M, Gorgun M, Kara C. The evaluation of gallstone formation in patients undergoing Roux-en-Y gastric bypass due to morbid obesity. Ulus Cerrahi Derg 30 (2014): 76-79.
- Elms L, Moon RC, Varnadore S, et al. Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2,395 cases at a single institution. Surg Endosc 28 (2014): 1624-1628.
- Rogula T, Yenumula PR, Schauer PR. A complication of Roux-en-Y gastric bypass: intestinal obstruction. Surg Endosc 21 (2007): 1914-1918.
- Champion JK, Williams M. Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass. Obes Surg 13 (2003): 596-600.
- Adotey JM. Incisional hernia: a review. Niger J Med 15 (2006): 34-43.
- Bettini S, Belligoli A, Fabris R, et al. Diet approach before and after bariatric surgery. Rev Endocr Metab Disord 21 (2020): 297-306.
- Ward L. Pre Bariatric Surgery Diet: information for patients (2010).


 Impact Factor: * 4.2
Impact Factor: * 4.2 Acceptance Rate: 72.62%
Acceptance Rate: 72.62%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 